- Get new issue alerts Get alerts

Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Case report for a patient with an inguinal hernia diagnosed with an Amyand’s hernia during surgery
AlKwider, Hussam A. MS a ; Froh, Mamon MD b
a Faculty of Medicine, University of Aleppo
b Faculty of Medicine, University of Aleppo, Al-Assad and Al-Mowasat Hospital, Daraa, Syrian Arab Republic
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article
Published online 24 May 2023
* Corresponding author. Address: Faculty of Medicine, University of Aleppo, Damascus, Syrian Arab Republic. Tel: +963 937 943 025; fax: +963212680111. E-mail: [email protected] (H.A. AlKwider).
This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-NC-ND), where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially without permission from the journal. http://creativecommons.org/licenses/by-nc-nd/4.0/
Introduction and importance:
Amyand’s hernia is rare, occurs when the appendix is located within the hernial sac, is difficult to diagnose prior to surgery, and is considered to be discovered during surgery.
Case presentation:
A 4-year-old child was brought to the medical clinic by her mother with a swelling complaint in the right inguinal region. Following clinical diagnosis and imaging tests, an indirect inguinal hernia was found to be present. It was decided to perform surgery on the child, and he was taken to the operating room and given general anesthesia. An incision was made on the right inguinal side, reaching the spermatic cord and the ostium internum, where a hernia sac was found containing the inflamed appendix. The appendix was removed from the edges of the hernia sac, tied off at its base, and cut. Finally, the hernia sac was closed without the use of a mesh, the surgical incision was closed, and the wound was dressed.
Clinical discussion:
The diagnosis of inguinal hernia is initially made based on the symptoms presented by the patient, as well as through ultrasound imaging. For surgical management, there is a classification called Losanoff and Basson, which discusses the surgical treatment options necessary for different types of Amyand hernias. The hernia is classified into four types based on the clinical presentation of the patient and the condition of the appendix, and each type has its own treatment.
Conclusion:
Amyand’s hernia is an uncommon condition diagnosed during surgery.
Introduction
- Amyand hernia is uncommon, accounting for 0.5–1% of all hernias, and occurs in 0.1% of inguinal hernias.
- Amyand’s hernia is an uncommon condition that occurs when the appendix is in the inguinal hernial sac.
- It is discovered during surgery.
Amyand’s hernia is a rare type of inguinal hernia in which the appendix becomes trapped in the hernia sac 1–7 . It was first described by Claudius Amyand in 1735 1–2 . These hernias are uncommon and occur in less than 1% of all inguinal hernias 3 . They can affect both adults and children, with men being more frequently affected than women 1 . Amyand’s hernia can be clinically significant, as it may lead to inflammation or infection of the appendix, requiring surgical intervention. In this case report, we present a clinical case of a 4-year-old child diagnosed with an Amyand hernia during surgery.
Presentation of case
Complaint: A 4-year-old child was brought to the doctor’s clinic by his mother, where she noticed a swelling in the right inguinal area. When asked about the swelling, the mother told us that it increases during crying and coughing.
Medical and allergy history: There are no previous medical or allergy histories.
Family history: One family member underwent surgery to repair an inguinal hernia.
On clinical examination, an indirect inguinal hernia was found on the right side. It was noted that the swelling increased during coughing and that there was pain at the site of the swelling.
Ultrasound revealed a hernial sac.
After taking a pathological history, conducting a clinical examination, and performing an ultrasound examination, it was decided to perform surgery on the child, and he was taken to the operating room and given general anesthesia. An incision was made on the right inguinal side, reaching the spermatic cord and the ostium internum, where a hernia sac was found containing the inflamed appendix. The appendix was removed from the edges of the hernia sac, tied off at its base, and cut. Finally, the hernia sac was closed without the use of a mesh, the surgical incision was closed, and the wound was dressed (see Fig. 1 ).

After the operation, the child’s condition was stable and fluids were given. Vital signs were monitored, and gas and urine were passed.
The child was discharged the day after the operation and prescribed antibiotics.
Amyand’s hernia refers to the presence of the appendix within an inguinal hernia and was first treated by the French surgeon Claudius Amyand in 1735 1 .
Amyand’s hernia is a very rare disease that accounts for only 0.1% of inguinal hernia cases and is difficult to diagnose, often discovered during surgery. Right-sided hernias occur more often than left-sided hernias due to the anatomical location of the appendix on the right, and Amyand’s left-sided hernia is extremely rare. Clinical evaluation using ultrasound and computed tomography is useful in assessing the condition of an inguinal hernia in cases of acute abdomen without acute appendicitis, which helps to make the decision to surgically open the abdomen to prevent the patient’s condition from deteriorating, and the inflamed appendix is removed during surgery. Surgery is the main treatment method, but in recent years, the laparoscopic approach has been widely used, which provides benefits such as shorter hospital stays, faster recovery, and less pain after surgery 1 .
For surgical management, the Losanoff and Basson classification outlines four types of Amyand’s hernias 2 :
Type 1: refers to an Amyand hernia with no inflammatory changes; management includes reducing the hernia, inserting a mesh, and in young patients, an appendectomy may be done.
Type 2: refers to Amyand hernia with septic changes restricted to the hernial sac; management involves an appendectomy done through the hernia along with a primary repair of the hernia. In this case, no mesh is inserted.
In the case of the child discussed, the management falls under the second type.
Type 3: refers to Amyand hernia involving the spread of sepsis outside the hernial sac; management includes laparotomy, appendectomy, and primary repair of the hernia without mesh.
Type 4: refers to Amyand hernia with acute appendicitis and other related or unrelated abdominal lesions; management of type 4 is similar to type 1–3 hernia management, along with appropriate treatment of the second pathology.
We report a case managed by open surgery. This case report is in accordance with the SCARE (Surgical CAse REport) 2021 guidelines 8 .
The diagnosis of inguinal hernia is initially made based on the symptoms presented by the patient as well as through ultrasound imaging. Amyand’s hernia is typically discovered incidentally during surgery. Laparoscopy provides a diagnostic and treatment method for this type of hernia.
Ethical approval
Informed consent.
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
There are no funding sources.
Author contribution
Hussam Akram AlKwider and Mamon Issa Froh.
Conflicts of interest disclosure
There are no conflicts of interest.
Research registration unique identifying number (UIN)
No, case report.
Hussam Akram AlKwider.
Data availability statement
Provenance and peer review.
Not commissioned, externally peer-reviewed.
- Cited Here |
- Google Scholar
acute appendicitis; Amyand hernia; case report; hernia repair; inguinal hernia; sac hernia
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Retinal artery macroaneurysm complicated with subhyaloid hemorrhage: two case....
- Case report
- Open access
- Published: 29 April 2019
Vasitis: a rare diagnosis mimicking inguinal hernia: a case report
- Chih-Wei Chen 1 ,
- Chin-Ho Lee 1 ,
- Tsung-Yi Huang 2 &
- Yi-Ming Wang 1
BMC Urology volume 19 , Article number: 27 ( 2019 ) Cite this article
89k Accesses
15 Citations
2 Altmetric
Metrics details
Vasitis or inflammation of the vas deferens is a rare condition, and few case reports with computed tomography images have been published since 1980.
Case presentation
A 50-year-old man presented with severe right inguinal and lower abdominal pain. Initial diagnosis at the emergency department was incarcerated or strangulated inguinal hernia. The computed tomography scan revealed diffuse edematous changes of right spermatic cord and vas deferens with peripheral fat stranding. Correlating with his clinical symptoms, signs, and imaging findings, the diagnosis of vasitis was made. We report a case of acute vasitis about the cause, symptom, pathogen, differential diagnoses, image findings, and treatment.
Although very rare, vasitis should be listed as one of the differential diagnosis for inguinal mass lesions. Cross-sectional imaging may be necessary to confirm the diagnosis and exclude differentials such as an inguinal hernia. Recognition of the characteristic image findings can help to make the correct diagnosis and avoid unnecessary surgery.
Peer Review reports
Acute vasitis or inflammation of the vas deferens is an extremely rare disease, with only about twenty adult case reports published since 1980. Few of these contain computed tomography (CT) images [ 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 ]. Clinically, it presents with nonspecific symptoms of inguinal swelling and local pain that can mimic orchitis, epididymitis, testicular torsion, and inguinal hernia. Familiarity with symptoms, image findings, and differential diagnoses is essential to prevent unnecessary surgery, especially when symptoms mimic an inguinal hernia.
A middle-aged male presented to our emergency department with severe right inguinal and lower abdominal pain, exaggerated by walking and Valsalva’s maneuver. He did not have a fever or chillness. The patient has no other prior medical history, no trauma history, no recent travel history, and no habitual alcohol and cigarette consumption. The patient is of Han Chinese origin and is currently working as an office clerk. He denied any family history of similar symptoms, no recent heavy lifting activities, and no high-risk sexual behaviors. The physical examination revealed tenderness and swelling in the right inguinal area. The laboratory tests revealed leukocytosis (11.39 × 103 /uL), elevated C reactive protein (35.4 mg/L) and leukocyturia, but a negative result of the urine culture. Due to the progression of localized right inguinal pain, the emergency doctor arranged computed tomography scan to rule out incarcerated inguinal hernia. The scan revealed diffuse edematous changes of right spermatic cord and vas deferens with peripheral fat stranding and no herniated bowel loop [Figs. 1 , 2 ]. Correlating the patient’s clinical symptoms, signs, and, imaging findings, the emergency doctor was able to overturn the initial diagnosis of an inguinal hernia and confirm vasitis. Empirical antibiotic treatment (Levofloxacin) was prescribed with good response.
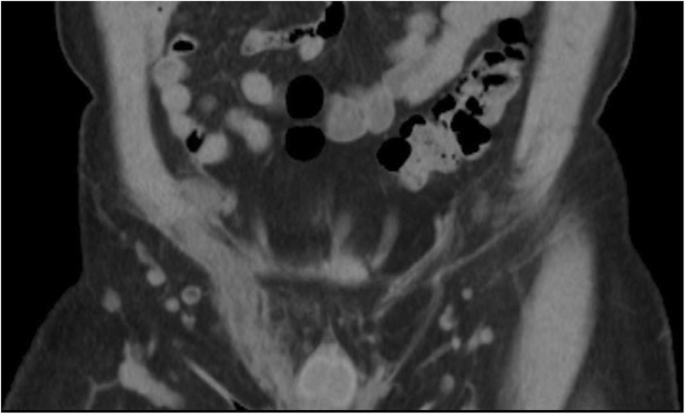
Non-enhanced coronal CT image revealed diffuse edematous change of right spermatic cord (white arrow)

Non-enhanced axial CT image revealed dilated right vas deferens with peripheral fat stranding (white arrows)
Dates | Patient Relevant Past Medical History and Interventions | ||
No previously medical or surgical history. No family medical history. | |||
Dates | Summaries from Initial Emergency and Follow-up Visits | Diagnostic Testing | Interventions |
2017-Feb | Came to the emergency department due to severe right inguinal and lower abdominal pain. | Physical examination: Right inguinal mass with pain, exaggerated when walking and Valsalva’s maneuver. | Prescribed oral antibiotic use: 500 mg of Levofloxacin (Cravit) daily for two weeks. |
laboratory data: leukocytosis, elevated C reactive protein and leukocyturia, | |||
CT: Revealed unilateral edematous spermatic cord without evidence of herniated bowel loop. | |||
7 Days later | Out-patient department follow-up. | Symptoms improved. | |
14 Days later | Out-patient department follow-up. | Symptoms improved. | |
Discussion and Conclusions
Inflammation of the vas deferens or vasitis is a rare condition categorized by Chan and Schlegel as acutely painful infective vasitis or asymptomatic vasitis nodosa [ 8 ]. Vasitis nodosa was first described in 1943 by Benjamin [ 9 ] as asymptomatic, chronic inflammatory reactions associated with blockage of the vas deferens, which causes high intra-luminal pressure with spermatozoa leakage and inflammatory process. Clinical presentation is with asymptomatic nodular lesions in the vas deferens, and most cases have a history of vasectomy. No specific treatment is required [ 4 ].
Acute infective vasitis is thought to be due to the retrograded spread of common urinary pathogens including Haemophilus influenza and Escherichia coli . However, urinary culture is usually negative. Other rare pathogens reported include Chlamydia trachomatis and Mycobacterium tuberculosis [ 4 , 6 ].
Most cases of the previously reported vasitis patients have histories of surgeries in close proximity to the affected vas deferens. Due to the low prevalence nature of acute vasitis, other risk factors have not been credited to this condition. A retrospective review was conducted by Clavijo et al. in 2010 where the clinical characteristics of eleven patients were thoroughly evaluated [ 10 ]. Of the eleven subjects, eight had previous surgeries in the neighboring regions, such as herniorrhaphy, prostatectomy, and perianal fistulectomy. The review also proposed other risk factors such as trauma history, concurrent human immunodeficiency virus/herpes simplex virus infections, and smoking habits [ 10 ]. Interestingly, our patient had none of the aforementioned risks factors.
Clinical symptoms include localized pain or palpable mass in the scrotal or inguinal region, some of them with leukocytosis or fever. Acute vasitis could be classification as three groups depending on involved site: scrotal, suprascrotal, and prepubic. It can be easily confused when there is isolated site involvement [ 11 ]. The common differential diagnoses include orchitis, epididymitis, testicular torsion, and inguinal hernia. Correct diagnosis is essential because the treatment of vasitis is via antibiotics, and operation is not required [ 6 ].
The diagnosis of vasitis could be a challenge by its rarity and unclear image findings. We review past reports that suggest appropriate tools include ultrasound, computed tomography and magnetic resonance imaging (MRI). Ultrasound can be used to exclude orchitis, epididymitis, and testicular torsion by color Doppler. Acute vasitis often reveals heterogeneous, hypoechoic spermatic cord and echogenic fat surrounding the lesions. However, ultrasound is relatively challenging to differentiate from incarcerated inguinal hernia to vasitis [ 12 ]. CT and MRI are more recommended to confirm the diagnosis. Spiral CT has high resolution and short scanning time. Acute vasitis typically reveals unilateral edematous spermatic cord without evidence of herniated bowel loop. MRI can provide more soft tissue detail, abnormal signal intensities of inflamed or ischemic structures, with the additional benefits of no radiation exposure [ 3 , 6 , 7 , 12 ].
Based on the available literature, the majority of the reported vasitis can be resolved with the use of anti-inflammatories and antibiotics alone [ 3 , 8 ]. Some authors prescribed oral antibiotics while others started with intravenous antibiotics in combination with oral antibiotics [ 6 ]. A reported pediatric vasitis case suggested only partial regression of the inguinal swelling symptoms with 7 days of oral antibiotic use, and the patient was later admitted and treated successfully with intravenous antibiotics [ 13 ]. Surgical exploration and drainage may be necessary in more severe cases that are not responsive to antibiotic treatment [ 10 ]. En bloc excision of the vas deferens is uncommon and is usually performed for the exceptionally rare cases of Tuberculous vasitis [ 14 ]. For our patient, we prescribed empirical antibiotic treatment with 500 mg of Levofloxacin once daily for two weeks. The patient’s symptoms improved drastically upon the scheduled weekly follow-ups.
In summary, we present a rare case mimicking incarcerated inguinal hernia, and although vasitis is very rare, physicians should keep in mind that patients might present with similar symptoms, especially when the patient has risk factors such as previous vasectomy and concurrent leukocyturia. CT or MRI scan can play an important role to prevent unnecessary surgery.
Abbreviations
Computed tomography
Magnetic resonance imaging
Wilson SR, Katz DS. Computed tomography demonstration of epididymitis with extension to vas deferens. Urology. 2006;68:1339–40.
Article Google Scholar
Yang DM, Kim HC, Lee HL, et al. Sonographic findings of acute vasitis. J Ultrasound Med. 2010;29:1711–5.
Eddy K, Connell D, Goodacre B, et al. Imaging findings prevent unnecessary surgery in vasitis: an under-reported condition mimicking inguinal hernia. Clin Radiol. 2011;66:475–7.
Article CAS Google Scholar
Dylewksi J, Sygal V. Infectious vasitis caused by chlamydia trachomatis. Infec Dis Clin Pract. 2014;22:e16–7.
You SH, Sung DJ, Han NY, et al. Emphysematous vasitis misdiagnosed as strangulated inguinal hernia. J Emerg Med. 2014;47:e15–7.
Patel K, Lamb B, Pathak S, Peters J. Vasitis: the need for imaging and clinical acumen. BMJ Case Rep. 2014;2014. https://doi.org/10.1136/bcr-2014-206994 .
Google Scholar
Kerkeni W, Saadi A, Ben Miled A, et al. Vasitis: an uncommon diagnosis mimicking incarcerated inguinal hernia. Urology. 2016;93:e1.
Chan PTK, Schlegel PN. Inflammatory conditions of the male Excurrent ductal system. Part II. J Androl. 2002;23:461–9.
PubMed Google Scholar
Benjamin JA, Robertson TD, Cheetham JG. Vasitis nodosa: a new clinical entity simulating tuberculosis of the vas deferens. J Urol. 1943;49:575–82.
Clavijo RI, Rose-Nussbaumer J, Turek PJ. Clinically symptomatic vasitis: clinical correlations in a rare condition. Syst Biol Reprod Med. 2010;56(6):445–9.
Middleton WD, Dahiya N, Naughton CK, et al. High-resolution sonography of the normal extrapelvic vas deferens. J Ultrasound Med. 2009;28:839–46.
Eddy K, Piercy GB, Eddy R. Vasitis: clinical and ultrasound confusion with inguinal hernia clarified by computed tomography. Can Urol Assoc J. 2011;5:E74–6.
Schurr E, Cytter-Kuint R, Ehrlichman M, Weiser G. Pediatric vasitis: a rare complication of epididymitis. Can Urol Assoc J. 2014;8(5–6):E436–8.
PubMed PubMed Central Google Scholar
Yang DM, Kim HC, Kim SW, Lee HL, Min GE, Lim SJ. Sonographic findings of tuberculous vasitis. J Ultrasound Med. 2014;33(5):913–6.
Download references
Acknowledgements
Not applicable.
There are no funding sources for this case report.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and affiliations.
Department of Radiology, Kaohsiung Medical University Hospital, Kaohsiung Medical University, No. 100, Ziyou 1st Rd., Sanmin District, Kaohsiung City, 80756, Taiwan, Republic of China
Chih-Wei Chen, Chin-Ho Lee & Yi-Ming Wang
Department of Urology, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung City, Taiwan
Tsung-Yi Huang
You can also search for this author in PubMed Google Scholar
Contributions
CC and YW were responsible for the concept and drafted the manuscript. CL and TH gave intellectual content and critically reviewed the manuscript. YW was responsible for the official radiology report. All authors have given final approval of the version to be published. All authors have participated sufficiently in the work to take public responsibility for appropriate portions of the content; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Correspondence to Yi-Ming Wang .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Chen, CW., Lee, CH., Huang, TY. et al. Vasitis: a rare diagnosis mimicking inguinal hernia: a case report. BMC Urol 19 , 27 (2019). https://doi.org/10.1186/s12894-019-0460-x
Download citation
Received : 09 March 2018
Accepted : 12 April 2019
Published : 29 April 2019
DOI : https://doi.org/10.1186/s12894-019-0460-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Vas deferens
- Inguinal hernia
BMC Urology
ISSN: 1471-2490
- General enquiries: [email protected]
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
49 templates

44 templates

61 templates
american history
85 templates

el salvador
34 templates

63 templates
Hernias Clinical Cases
It seems that you like this template, hernias clinical cases presentation, free google slides theme, powerpoint template, and canva presentation template.
How do you know if you’ve developed a hernia? What are the risk factors? Can they be prevented or treated? Is surgery involved? Here’s a template that lends itself to answering all these questions by citing clinical case studies you’ve made of patients with hernias. Download these slides for Google Slides or PowerPoint and add your content to them - they’re fully editable so it’s easy! - and bring your colleagues up to speed on your discoveries or informa your patients about the disease.
Features of this template
- 100% editable and easy to modify
- 33 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Register for free and start downloading now
Related posts on our blog.


How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.
Premium template
Unlock this template and gain unlimited access

- Search Menu
- Sign in through your institution
- Volume 2024, Issue 8, August 2024 (In Progress)
- Volume 2024, Issue 7, July 2024
- Bariatric Surgery
- Breast Surgery
- Cardiothoracic Surgery
- Colorectal Surgery
- Colorectal Surgery, Upper GI Surgery
- Gynaecology
- Hepatobiliary Surgery
- Interventional Radiology
- Neurosurgery
- Ophthalmology
- Oral and Maxillofacial Surgery
- Otorhinolaryngology - Head & Neck Surgery
- Paediatric Surgery
- Plastic Surgery
- Transplant Surgery
- Trauma & Orthopaedic Surgery
- Upper GI Surgery
- Vascular Surgery
- Author Guidelines
- Submission Site
- Open Access
- Reasons to Submit
- About Journal of Surgical Case Reports
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, case presentation, conflict of interest statement, authors' contributions.
- < Previous
Obturator hernia: case report
- Article contents
- Figures & tables
- Supplementary Data
Esubalew Taddese Mindaye, Dereje Giduma, Tesfaye H Tufa, Obturator hernia: case report, Journal of Surgical Case Reports , Volume 2020, Issue 10, October 2020, rjaa389, https://doi.org/10.1093/jscr/rjaa389
- Permissions Icon Permissions
Obturator hernia, protrusion of abdominal content through the obturator foramen, is a rare type of abdominal wall hernia. Late patient presentation is associated with significant morbidity and mortality. We present rare case of obturator hernia causing small bowel obstruction in a 65-year-old-female patient. She presented with crampy abdominal pain, nausea and vomiting of three days duration. She was diagnosed with acute surgical abdomen and managed surgically at Arsi University College of health sciences, Assela, Ethiopia. Intraoperative finding revealed left-side obturator hernia, which is an extremely rare occurrence. Despite delayed presentation, our patient had smooth postoperative recovery. Obturator hernia is exceedingly rare, and it poses a diagnostic challenge as signs and symptoms are often nonspecific, making a preoperative diagnosis difficult. So, it should be considered as differential diagnosis in elderly patients presenting with acute surgical abdomen.
Although it accounts for only 1% of all abdominal wall hernias, obturator hernia has relatively higher morbidity and mortality (15–25%), mainly due to delayed diagnosis with infarcted bowel (60–75%) [ 1 , 2 ]. It was first described by Pierre Roland Arnaud de Ronsil in 1724 as a rare type of pelvic hernia [ 3 ]. The typical patients are elderly, multiparous, chronically ill and thin women being named as ‘the skinny old lady hernia’ [ 2 , 4–6 ]. This is because women have broader pelvis and larger obturator canal [ 6 ]. In emaciated elderly people, loss of fatty tissue coupled with increased intraabdominal pressure facilitates the hernia formation [ 6 , 7 ]. Obturator hernia commonly occurs on the right side due to larger sigmoid on the left side protecting the canal [ 6 ].
Accurate pre-operative diagnosis of obturator hernia is usually difficult, and most patients are operated as intestinal obstruction of unknown cause [ 8 ]. Patient presentations are nonspecific ranging from thigh or knee pain in the affected side to recurrent bouts of intestinal obstruction with cramping abdominal pain, nausea and vomiting [ 7 , 8 ]. Howship–Romberg sign, which refers to ipsilateral groin pain aggravated by extension, abduction and medial rotation, radiating down the thigh as a result of irritation of the obturator nerve, is a characteristic sign of obturator hernia. However, it is present in only 15–50% of the patients with obturator hernia [ 2 , 5 , 8 ].
Plain radiographs often show nonspecific findings of small bowel obstruction and are seldom helpful in diagnosing obturator hernia [ 9 ]. Ultrasonography is also useful and reliable in the diagnosis of obturator hernia [ 10 ], but it is often limited by the relative inaccessibility of this deep region and is operator dependent. A computed tomography scan can accurately diagnose not only an obturator hernia but also other conditions of bowel obstruction [ 2 , 9 ].
Surgical management through midline abdominal incision is preferred for an obturator hernia, as it gives adequate exposure, allows reduction of hernia content and facilitates bowel resection if necessary [ 9 ].
Sixty-five-year-old-female patient with known cardiac illness on follow-up for the last 10 years presented with crampy central abdominal pain associated with nausea, frequent bilious vomiting of 3 days duration. She has no previous experience of similar compliant and has no previous abdominal surgery. For the above compliant, she went to nearby clinic from where she was referred to Assela referral hospital for better evaluation and management. On arrival to emergency surgical department, she was emaciated, acutely sick looking with tachycardia of 110 beat/minutes and blood pressure of 130/75mmhg. Abdominal examination revealed distended, hypertympanic abdomen with hyperactive bowel sound, but there was no sign of peritoneal irritation. Hernial sites were free, and digital rectal examination was unremarkable. Nasogastric tube insertion revealed bilious gastrointestinal content, and her basic laboratory examinations showed leukocytosis of 12,000 with left shift (neutrophil 85%), while plain abdominal X ray ( Fig. 1 ) showed dilated small bowel loops with absent rectal gas shadow.

Plain abdominal X-ray showing dilated small bowel loops with visible valvulae conniventes.
With the diagnosis of acute abdomen secondary to small bowel obstruction, she was prepared and operated through midline abdominal incision. Intraoperatively, there was herniated anti-mesenteric side of ileum about 20 cm proximal to ileocecal valve through the left obturator foramen (Richter type) ( Fig. 2 ). The bowel proximal to the hernia was dilated, while the distal segment was collapsed. Upon reduction, the hernia content was viable. The orifice of the obturator canal was closed with simple interrupted silk sutures, and laparotomy incision was closed in layers. Subsequently, the patient showed a remarkable improvement and was discharged from the hospital in a stable condition after 4 days of stay. Her follow-up for 6 months following surgery showed a normal post-operative course, and the patient was happy with her treatment.

Intraoperative picture showing herniated small bowel through the left obturator foramen.
Obturator canal is an opening in the superolateral part of the obturator foramen containing the obturator nerve and vessels. It is 2–3 cm long and 1 cm wide, and is usually filled with fat, allowing no space for hernia [ 2 ]. Loss of body fat and increase in intra-abdominal pressure are the major factors that lead to the development of hernia [ 2 , 5 ]. Weakened pelvic floor with multiple pregnancy, older age and emaciation due to her chronic illness are contributing factors in our patient. The commonest content of the sac is ileum with about 50% being of the Richter’s type, and our patient fits to this common type [ 2 ]. The most common clinical presentation is intestinal obstruction of an unknown cause as has occurred in our patient [ 2 , 8 ]. Although abdominopelvic CT scan is sensitive to diagnose obturator hernia preoperatively [ 2 ], most patients’ diagnosis are reached intraoperatively like our patient as it is an uncommon cause of acute surgical abdomen. Unlike the common finding in literatures, this patient has left obturator hernia, which is extremely a rare occurrence.
Mainstay of treatment is surgery [ 4 ]. The approach can be via transperitoneal approach (lower midline laparotomy), abdominal extraperitoneal approach or laparoscopically [ 8 ]. Lower midline laparotomy is the most common surgical approach in emergency cases as it gives the best exposure, allows reduction of hernia content and facilitates bowel resection if necessary [ 6 , 9 ]. The hernia repair can be a simple closure of the entrance of the canal with interrupted sutures or repair with mesh [ 5 ].
Patients with advanced age, associated respiratory and cardiovascular diseases and with late diagnosis have higher mortality rate up to 70% [ 5 , 8 ]. Although our patient fulfills some of these risks, she had smooth recovery likely due to absence of bowel infarction.
Obturator hernia as a cause of bowel obstruction is one of the rare surgical phenomenon. Preoperative diagnosis of obturator hernia is challenging due to nonspecific presentation and usually made intraoperatively. Delay in diagnosis, medical comorbidity and old age are associated with poor outcome. Despite having delayed presentation, our patient has good postoperative outcome.
None declared.
E.M. was involved in the surgery, conceived and conducted the study, did literature search and critical revision of the manuscript. D.G. was involved in the surgery, over all supervision of the manuscript and critical revision of the manuscript, T.T. did the overall supervision of the manuscript and critical revision of the manuscript. All authors have read and approved the manuscript.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Cuschieri A . Disorders of the abdominal wall, peritoneal cavity and retroperitoneum. In: Cuschieri A, Hanna G, eds., Essential Surgical Practice . London: CRC Press , 2015 , 473 – 516 .
Google Scholar
Google Preview
Mantoo S , Mak K , Tan T . Obturator hernia: diagnosis and treatment in the modern era . Singap Med J 2009 ; 50 : 866 – 70 .
Rogers FA . Strangulated obturator hernia . Surg 1960 ; 48 : 394 – 403 .
Kulkarni SR , Punamiya AR , Naniwadekar RG , Janugade HB , Chotai TD , Singh TV , et al. Obturator hernia: a diagnostic challenge . Int J Surg Case Rep 2013 ; 4 : 606 – 8 .
Goon HK , Bahari HM . Obturator hernia: a case report . Med J Malaysia 1983 ; 38 : 200 – 2 .
Kammori M , Mafune K , Hirashima T , Kawahara M , Hashimoto M , Ogawa T , et al. Forty-three cases of obturator hernia . Am J Surg 2004 ; 187 : 549 – 52 .
Schmidt P , Bull W , Jeffery K , Martindale R . Typical versus atypical presentation of obturator hernia . Am Surg 2001 ; 67 : 191 .
Sá NC , Silva VCM , Carreiro PRL , Matos Filho AS , Lombardi IA . Rare case of incarcerated obturator hernia: case report and review of literature . Int J Surg Case Rep 2017 ; 37 : 157 – 60 .
Lin H-H , Juan C-W , Chew B-T , Chao J-H . Obturator hernia: Little old lady’s hernia . Int J Gerontol. 2010 ; 4 : 3 .
Yokoyama T , Munakata Y , Ogiwara M , Kamijima T , Kitamura H , Kawasaki S . Preoperative diagnosis of strangulated obturator hernia using ultrasonography . Am J Surg 1997 ; 174 : 76 – 8 .
- acute abdomen
- hernia, obturator
- intestinal obstruction
- obturator foramen
| Month: | Total Views: |
|---|---|
| October 2020 | 98 |
| November 2020 | 52 |
| December 2020 | 35 |
| January 2021 | 33 |
| February 2021 | 20 |
| March 2021 | 51 |
| April 2021 | 33 |
| May 2021 | 38 |
| June 2021 | 50 |
| July 2021 | 28 |
| August 2021 | 28 |
| September 2021 | 46 |
| October 2021 | 37 |
| November 2021 | 27 |
| December 2021 | 11 |
| January 2022 | 32 |
| February 2022 | 52 |
| March 2022 | 45 |
| April 2022 | 41 |
| May 2022 | 47 |
| June 2022 | 26 |
| July 2022 | 32 |
| August 2022 | 22 |
| September 2022 | 22 |
| October 2022 | 22 |
| November 2022 | 16 |
| December 2022 | 19 |
| January 2023 | 11 |
| February 2023 | 17 |
| March 2023 | 20 |
| April 2023 | 6 |
| May 2023 | 19 |
| June 2023 | 15 |
| July 2023 | 22 |
| August 2023 | 12 |
| September 2023 | 15 |
| October 2023 | 28 |
| November 2023 | 22 |
| December 2023 | 14 |
| January 2024 | 11 |
| February 2024 | 26 |
| March 2024 | 10 |
| April 2024 | 14 |
| May 2024 | 18 |
| June 2024 | 14 |
| July 2024 | 18 |
| August 2024 | 8 |
Email alerts
Citing articles via, affiliations.
- Online ISSN 2042-8812
- Copyright © 2024 Oxford University Press and JSCR Publishing Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals
You are here
- Volume 13, Issue 9
- Diagnostic difficulties in obturator hernia: a rare case presentation and review of literature
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-4644-5550 Tharun Ganapathy Chitrambalam ,
- Pradeep Joshua Christopher ,
- Jeyakumar Sundaraj and
- Sundeep Selvamuthukumaran
- General Surgery , SRM Institute of Science and Technology , Kattankulathur , India
- Correspondence to Dr Tharun Ganapathy Chitrambalam; tharungc{at}srmist.edu.in
Hernia arising from obturator canal is rare and it contributes to about less than 1% of incidence of all hernias. Diagnosing an obturator hernia clinically is a challenging one and nearly impossible. These hernias usually present as an intestinal obstruction as more than 50% of obturator hernias goes in for strangulation. Here, we report an unusual presentation of an obturator hernia in a 70-year-old woman who presented to emergency room with acute abdomen and uncomplicated reducible inguinal hernia. Radiological imaging showed obstructed inguinal hernia while on diagnostic laparoscopy, a strangulated and perforated obturator hernia of Richter’s type was seen in addition to an uncomplicated inguinal hernia. Obturator hernia, although very rare, is associated with high morbidity and mortality as it is often underdiagnosed as in our case. Laparoscopy bailed us out from missing out a perforation from an occult obturator hernia.
- ultrasonography
- general surgery
- gastrointestinal surgery
- small intestine
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bcr-2020-235644
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Obturator hernia is the protrusion of both intraperitoneal or extraperitoneal contents through the obturator canal. 1 Incidence of obturator hernia is about 0.73% of all hernias. 2 Obturator hernia typically affects women, elderly, multiparous, emaciated and those with increased intra-abdominal pressure. 3 It is never externally visible nor palpable, so it is often undiagnosed or unsuspected. The obturator hernia is most often the Richter's type, which can be a diagnostic challenge as focal strangulation of the bowel can progress to gangrene with or without overt signs of intestinal obstruction. 4 Richter’s hernia is a type of abdominal hernia in which only part of the circumference of the bowel is entrapped and strangulated in the hernial orifice. The segment of the engaged bowel is nearly always the lower portion of the ileum. 5
Case presentation
A 70-year-old woman was brought to the emergency room with uncomplicated reducible swelling in the right inguinal region for the past 3 years with sudden onset of pain over the swelling for 3 days. Pain was severe, gripping in character and constant which was relieved partly on flexion of the thigh. No history of any medical illness nor any previous surgeries. On physical examination, the patient was moderately nourished and built. Her heart rate was 102 beats/min and blood pressure was 130/70 mm Hg. Abdomen was soft, not distended with diffuse tenderness present over lower abdominal quadrants with no guarding or rigidity. On local examination, a swelling of size 4×3 cm was seen in the right inguinal region which was reducible with expansile impulse on coughing.
INVESTIGATIONS
Ultrasonogram of the abdomen revealed a possible right inguinal/femoral hernia with features of obstruction, and advised CT correlation. CT scan of the abdomen was done subsequently which showed a 3×3 cm defect in the right inguinal region with herniating bowel loops and overcrowding of ileal loops over the defect with free fluid noted around the ileal loops suggestive of obstructed inguinal hernia as seen in figure 1 .
- Download figure
- Open in new tab
- Download powerpoint
CT image depicting groin defect with overcrowding of bowel loops.
On a diagnosis of obstructed inguinal hernia, patient was posted for diagnostic laparoscopy and proceeded. After insufflation and creating pneumoperitoneum figure 2 , overcrowding of small bowel loops was seen in right inguinal region and pelvis with localised bilious collection of 50 mL in favour of early perforative peritonitis. On releasing the adhesions and bowel loops, a 3×3 cm defect was noted in the right inguinal region with viable bowel loops. On further release, 1.5×1.0 cm defect was noted in the obturator canal with perforation of entrapped bowel loop of Richter’s type seen. Laparotomy was done and a 1 cm perforation in terminal ileum with unhealthy edges was noted 20 cm from ileocaecal junction as seen in figure 3 . Thorough lavage was given. Perforation site resection and anastomoses were done in two layers. Anatomical repair of both the defects was done. Obturator defect was closed at first primarily with 1-polypropylene followed by closure of inguinal defect with interrupted 1-polypropylene sutures as depicted in figure 4 .
Hernial orifice filling with CO 2 after insufflation with veress needle.
Obturator and inguinal defects with perforated ileum on laparotomy after adhesiolysis.
Picture taken after obturator defect closure, while closure of inguinal defect is in process as labelled in figure.
Outcome and follow-up
The patient tolerated the procedure well with nil postoperative complications. Orals were started on postoperative day 4 after good bowel sounds, escalated to soft solids and discharged on postoperative day 7. The patient was periodically followed up for a period of 1 year who remained asymptomatic.
Obturator hernia is the protrusion of abdominal viscera through obturator canal in which the obturator nerve and vessels pass. This hernia is about six to nine times more common in women than men due to their broader triangular pelvis and greater transverse diameter. It affects women of around 70–90 years of age, the reason being attributed to atrophy of the preperitoneal fat around the obturator vessels in the canal thereby predisposing hernia formation and hence the name ‘little old woman’s hernia’. 3 The major risk factors for obturator hernia are chronic obstructive pulmonary disease, chronic constipation and ascites. Diagnosing an obturator hernia at the earliest is very difficult as it usually presents with non-specific signs and symptoms. Although it is a rare abdominal hernia, the mortality rate is as high as 70%. Major clinical symptoms are due to intestinal obstruction like abdominal pain, distension, nausea, vomiting and constipation. They may also have recurrent attacks of intestinal obstruction in the past with or without a palpable mass in the groin. 6
Emergency CT scanning could lead to rapid diagnosis and early surgical intervention and thus optimising the outcome. The use of CT scan in detecting obturator hernia was first reported by Meziane et al in 1983. 7 The common CT scan finding is herniated loop of distal small bowel extending through the obturator foramen between the pectineus and obturator externus muscles. In incarcerated hernia, CT scan shows associated bowel loop dilatation in the abdomen. Since the use of CT scan, preoperative diagnosis rate was improved from 43% to 90% in some reports. 8 However, it is not always possible to diagnose all obturator hernias using CT of the abdomen as seen in our case. Diagnostic laparoscopy serves as a tool in diagnosing and treating occult, suspected and missed obturator hernias on imaging. In our institution, we routinely practice and advocate laparoscopic method for uncomplicated groin hernias including suspected obturator hernias without bowel complications due to advantages like diagnostic accuracy of occult hernias, lesser postoperative pain and other complications. But in this case scenario, due to perforated ileum with peritonitis on laparoscopy and the need for resection and anastomosis, we converted to open surgical approach. Open approach with lower midline is considered the most preferred by many authors as it gives good exposure to the obturator ring and also aids in performing bowel resections when required. 9 In view of peritonitis in this case, mesh (non-absorbable or absorbable) was not employed for further reinforcement as non-absorbable meshes have higher chances of mesh rejection and absorbable meshes can get dissolved in the presence of bacterial infection.
Learning points
Obturator hernia, although very rare, is associated with high morbidity and mortality.
It is often underdiagnosed as in our case; the preoperative finding of hernia was because of the inguinal hernia with no bowel obstruction and it was an obturator hernia which did not show up clinically was strangulated with a perforated bowel of Richter’s type within it. The same could have been easily missed if an inguinal approach had been followed. Laparoscopy bailed us out from missing out a perforation from an occult obturator hernia.
Laparoscopy should be considered as a tool of choice in cases of an occult obturator hernia and unclear hernias arising from the myopectineal orifice of Fruchaud.
- Susmallian S ,
- Ponomarenko O ,
- Barnea R , et al
- Silva VCM ,
- Carreiro PRL , et al
- Yokoyama Y ,
- Yamaguchi A ,
- Isogai M , et al
- Kulkarni SR ,
- Punamiya AR ,
- Naniwadekar RG , et al
- Nishina M ,
- Ogino R , et al
- Chuang C-H , et al
- Hodgins N ,
- Cieplucha K ,
- Conneally P , et al
Twitter @15jo12
Contributors TGC is the major contributor of this study. Study design, data analysis, interpretation, drafting, critical revision and final approval of the article were done by him and he is completely accountable for the research work. PJC, Dr Jeyakumar Sundaraj and SS have helped in planning and reporting, extending administrative support, technical writing and proofreading.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Surg Case Rep
- v.85; 2021 Aug
Morgagni hernia in adult: A case report
Sandip kuikel.
a Maharajgunj Medical Campus, Tribhuvan University, Institute of Medicine, Kathmandu, Nepal
Sanjib Shrestha
Sital thapa, narendra maharjan.
b Department of GI and General Surgery, Tribhuvan University Teaching Hospital, Maharajgunj Medical Campus, Institute of Medicine, Kathmandu, Nepal
Bishnu Prasad Kandel
Paleswan joshi lakhey, introduction and importance.
Morgagni Hernia is a congenital diaphragmatic hernia but can rarely present in adults. It occurs due to a congenital defect in the development of the diaphragm. Here we present a case of symptomatic Morgagni hernia diagnosed in a 53 years' female.
Case presentation
A 53 years' female presented with recurrent chest symptoms and was found to have bowel contents herniated into the right hemithorax on chest X-ray and CECT. Reduction of hernia was done laparoscopically and the hernia was repaired with non-absorbable suture in an interrupted manner.
Clinical discussion
Morgagni hernias are mostly diagnosed incidentally on a chest radiograph or can present with cardiorespiratory or abdominal symptoms. Our case was an adult who was diagnosed to have Morgagni hernia presenting with chest symptoms. The investigation of choice to diagnose and evaluate this condition is CECT of chest and repair of hernia without the use mesh is advised in asymptomatic cases also due to feared complications like strangulation and incarceration.
The treatment of Morgagni Hernia is primary surgical repair which can be done either transthoracically or transabdominally. It is advised that surgical repair should be done even in asymptomatic cases.
- • Morgagni Hernia is a congenital diaphragmatic hernia but can rarely present in adults.
- • Treatment of Morgagni Hernia is primary surgical repair which can be done either transthoracically or transabdominally with or without the use of Mesh.
- • It is advised that surgical repair should be done even in asymptomatic cases.
1. Introduction
Diaphragm is a muscular structure developed from multiple embryonic sources namely, the septum transversum, the pleuroperitoneal folds, and the somites [1] . If the anterior pleuroperitoneal membrane fails to fuse with the sternum and costal cartilages, it results in an anatomical defect in the costosternal trigone which is known as foramina of Morgagni [2] , [3] . Abdominal contents can herniate through this anterior defect resulting in the hernia known as the Morgagni hernia. It is one of the four possible congenital diaphragmatic herniae (CDH) accounting for 1–9% of them. The four types of CDH include Bochdalek hernia, Morgagni hernia, diaphragm eventration, and central tendon defects of the diaphragm [4] , [5] . CDH can be symptomatic or be diagnosed incidentally. The symptoms of CDH include nonspecific respiratory or gastrointestinal signs and symptoms [2] . Except for some rare cases, Morgagni hernia usually presents in childhood. Here in this case report, we present a case of a 53 years' female who had angina-like symptoms and later diagnosed to have Morgagni hernia. This case has been reported in line with the SCARE 2020 criteria [6] .
2. Case report
A 53 years' nonsmoker hypertensive female was admitted to our hospital to evaluate chest pain. Her chest pain was insidious in onset, localized to right side which was intermittent, pricking type, with no radiation, and aggravated on lying down. She had no history of cough, shortness of breath and orthopnea. She had no history of abdominal pain, altered bowel habit and abdominal trauma. She was evaluated four years back and diagnosed to have stable angina for which relevant treatment was done. But the symptoms recurred and this time, in chest X-ray there were bowel loops in the thoracic cavity ( Fig. 1 ). To further evaluate the case, a contrast-enhanced Computed Tomography (CECT) scan of the chest was done which showed a defect in the anterior aspect of right hemi diaphragm through which the ascending colon, hepatic flexure and right portion of the transverse colon along with omental fat were herniating into the right hemithorax, thus the diagnosis of Morgagni hernia was made ( Fig. 2 ).

Preoperative (a) chest X-ray posteroanterior view showing herniated bowel loops in the right thoracic cavity and postoperative (b) chest X-ray anteroposterior view showing expansion of lung field.

Transverse section of CECT scan of chest showing herniated bowel loops in the right thoracic cavity.
She was evaluated and laparoscopic repair of the defect was done using three ports (10 mm port at infraumbilicus for camera, two 5 mm ports at midclavicular line 3 cm above the umbilicus on each side). During the laparoscopic repair, transverse colon and omentum were seen to be herniated in the foramen Morgagni of approximately 3 cm size, thus confirming the pre-operative diagnosis of Morgagni Hernia ( Fig. 3 ). The hernia contents were reduced under direct vision, and foramen closed with a non-absorbable suture (polyester no.1) in an interrupted manner ( Fig. 4 ). The sac was not excised. A close suction drain of 10 Fr. size was inserted through the epigastric port into the hernia cavity. The drain was kept in negative suction and removed on the third postoperative day. A post-operative X-ray was done which showed expansion of lung field and reduction of hernia contents into the abdomen ( Fig. 1 ). The patient had asymptomatic hypoxia (SPO2 = 84 to 88% in room air) for 5 days postoperatively, which was treated with oxygen support via nasal cannula at two liters per minute, chest physiotherapy and oral mucolytic (Bromhexine). Imaging and physical examinations during this period revealed no abnormalities. On the 6th day, she had complete resolution of symptoms and was discharged on the seventh postoperative day.

Laparoscopic view of abdomen showing herniation of abdominal content through foramen Morgagni.

Laparoscopic view of hernia orifice after reduction of hernia (a) and after its repair (b).
3. Discussion
Morgagni hernia is the rarest of all CDH, presenting mostly in childhood [4] , [5] . There are some reports documenting its presentation in adulthood [7] , [8] , [9] , [10] . The present case, a 53 years' female was diagnosed as having CDH after developing cardiovascular and respiratory symptoms repeatedly. CDH was suspected due to visualization of bowel loops in the right side of the thoracic cavity on chest X-ray and was confirmed by CECT scan of the chest which showed herniating bowel loops along with omental. The defect was closed laparoscopically using nonabsorbable suture as the size of the defect was small (approximately 3 cm).
Most of the cases of Morgagni hernia are diagnosed incidentally on a chest radiograph and they are mostly right-sided. They are seen as homogenous mass along with (if hollow viscus is herniated) or without air-fluid level. If symptomatic, symptoms can mimic respiratory or cardiovascular diseases. Abdominal pain is seen in cases where the viscera get strangulated or incarcerated. Most commonly the herniated mass comprises of omentum followed by the colon and small intestine. However, stomach is the most common herniated part in left-sided Morgagni hernia [11] , [12] .
The investigation of choice for cases like this is CECT scan of the chest. It is preferred as it can provide the anatomical details of the hernia, its contents and its complications if any. If there is presence of a retrosternal mass of fat density or a combination of omentum and a hollow viscus organ, then the diagnosis is established [13] . In cases of diagnostic difficulty, magnetic resonance imaging (MRI) has been reported to be used to differentiate CDH from other mediastinal masses [14] . Complication of Morgagni hernia can be strangulation; thus surgical repair of the defect is advised even in asymptomatic cases [15] . Morgagni hernia can be repaired via abdominal approach (laparotomy or laparoscopically) or transthoracic approach [11] , [16] . There is no common consensus on which approach is better, however abdominal approach via laparotomy is preferred in cases of suspected strangulation or dense adhesions. The hernia orifice can be repaired using Mesh or simply by non-absorbable sutures. Mesh or no mesh depends on hernia size and the possibility of achieving a tension-free repair without a prosthesis. It is reported by a case series of 36 patients that there can be successful repair of the defect without using Mesh and have no recurrence [17] . There is no strong recommendation on the cutoff size of the hernia defect to advise use of mesh. Mesh can be considered in cases where there is marked tissue loss of the diaphragm and primary repair is not possible [10] , [18] . Although removal of sac has many advantages like reduction of tissue trauma, low risk of fluid collection and low recurrence, it is advised that the sac not be removed due to the feared complication of massive pneumo-mediastinum [19] , [20] . Drain was used in our case to minimize the risk of fluid collection in the dead space created by the reduction of hernia sac but there is no strong evidence for use of drain in laparoscopic repair of Morgagni hernia.
4. Conclusion
Morgagni hernia is a rare type of CDH which is usually identified in childhood but occasionally in adult. It can present with acute chest symptoms or can be asymptomatic. Diagnosis of this condition is done by CECT chest and treatment is primary surgical repair without Mesh wherever possible. This can be done either transthoracically or transabdominally. It is advised that surgical repair should be done even in asymptomatic cases.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
No funding was provided for the preparation of this manuscript.
Ethical approval
Case reports do not require ethical approval by our institution.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
All authors contributed to the manuscript preparation including data acquisition, literature review and writing. NM, BPK and PJL were involved in the performing the procedure.
Research registration
Not applicable.
Dr. Sandip Kuikel
Maharajgunj Medical Campus, Tribhuvan University Institute of Medicine.
Declaration of competing interest
None declared.
Annals of Emergency Surgery

A Rare Case of Elective Hernia Surgery: Littre Hernia
- 1. Department of Surgery, Izmir Katip Celebi University, Turkey
Meckel diverticulum (MD) is the most frequently seen congenital anomaly of the gastrointestinal system. Littre hernia (LH) is defined as the presence of MD in a hernia sac. Although LH is commonly seen in emergency surgeries such as incarceration and obstruction or hemorrhage, it is rare in elective surgeries. Herein, we present a rare case of MD which was detected during elective inguinal hernia surgery.
Meckel diverticulum, Littre hernia, Elective surgery, Inguinal hernia
Kamer E, Orse A, Er A, Cengiz F, Ozogul M, et al. (2017) A Rare Case of Elective Hernia Surgery: Littre Hernia. Ann Emerg Surg 2(1): 1004.
ABBREVIATIONS
MD: Meckel Diverticulum; LH: Littre Hernia
INTRODUCTION
Meckel diverticulum (MD) is the most commonly seen congenital anomaly of the gastrointestinal system, accounting for 1 to 3% of cases [1]. It occurs due to theimproper closure of the omphalomesenteric duct [1]. It was first described by Wilhelm FabriciusHildanus in 1598 [2]. Incarceration of MD was first described anecdotally in 1700 by Littre, a French surgeon [1,2]. However, this anomaly was named and its pathophysiology was first explained in 1809 by Johann Friedrich Meckel [1]. It frequently occurs on the terminal ileum [2]. It has clinical relevance, as it may cause complications such as intestinal obstruction, diverticulitis, hemorrhage, and perforation [1,2].
Littre hernia (LH) is defined as the presence of MD in a hernia sac [1]. It was first described in 1700 by Alexis Littre; however, the term LD was used for the first time in 1841 by Reinke [2]. About 50% of LH can occur in the inguinal region, 20% in the femoral site, 20% in the umblical site, and the remaining 10% in other locations [3]. In this report, we present a rare case of MD which was detected during elective inguinal hernia surgery.
CASE PRESENTATION
A 62-year-old male patient was admitted to our outpatient clinic with complaints of pain and swelling in his left inguinal region and left inguinal hernia was detected. He had hypertension with no incarceration. His physical examination findings and laboratory test results were normal. A written informed consent was obtained from the patient. He underwent standard preoperative examinations, and elective hernia surgery was performed with left inguinal incision. During surgery, indirect inguinal hernia was detected. Upon opening the hernia sac, omentum and loops of small intestine were found within. A MD of 6-cm in length and 2-cm in size was detected on the wall of the small intestine (Figure 1).
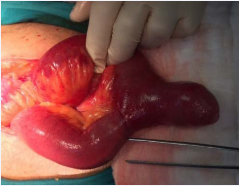
Figure 1: A large amount of small bowel with Meckel’s diverticulum in hernia sac.
Stapler-assisted wedge resection was, then, performed, and followed by inguinal hernia repair using a standard prolene mesh. Stapler was applied to the base of the diverticulum, perpendicular to the base of the diverticulum but transverse to the longitudinal axis of the bowel. The stapler was fired and the diverticulum was resected off the ileum. Small bleeding points at the edge of the staple line, if present, were sutured intracorporeally with 3-0 Vicryl. The postoperative period was uneventful, and the patient was discharged next day. Patient was followed up for 9 months, and was found to be symptom-free.
Meckel diverticulum, which is the most frequently seen congenital anomaly of the gastrointestinal system, is a true diverticulum that contains all layers of the intestinal wall [4]. It occurs due to the failure of the omphalomesenteric duct to close, which should take place around seventh to eight weeks of pregnancy [6]. It is usually asymptomatic [4]. The definite diagnosis is made during surgery for complications such as hemorrhage, ulceration, infection or ileus [4]. In adults, 4 to 10% of MD cases are incidentally diagnosed during surgery for other reasons [3]. It is seen twice as much in males as females [4]. Obstruction of the small intestine in adults and hemorrhage in children are most common complications [5,6]. One of the complications of MD is LH, which is observed in 10% of the cases, and is usually seen during infancy [2,5,6]. It most commonly involves the abdomen in infants, and the inguinal region in adults [3,6]. It usually occurs in the right inguinal region [7]. In our case, LH was also localized in the right inguinal region.
In case of incomplete reduction of incarcerated hernias, fecal fistula in hernia, rectal hemorrhage or recurring stomach pain, diagnosis should be made intraoperatively, although LH is initially suspected [3,6]. In the literature, there are reported cases with hemorrhage, obstruction and perforation, and most frequently, incarceration [7-9]; however, the number of cases of LH diagnosis during elective surgery is very limited [9]. In our case, LH was detected during elective hernia surgery.
Treatment is controversial in MD. In patients with symptoms and complications, surgical treatment is indispensible. In case of an incidental diagnosis, there is a consensus on performing resection among pediatric surgeons; however, indication of prophylactic MD resection still remains controversial in adults [3,4]. In case of a broad-based diverticulum, segmental resection is recommended, whereas diverticulectomy would be sufficient in the narrow-based ones. Biel et al. performed wide-V wedge resection in a case with MD which was detected during elective inguinal hernia surgery [9,10]. Similarly, our case underwent wedge resection.
In conclusion, this report highlights that the detection of MD in the hernia sac during elective inguinal hernia surgery is rare and resection of MD is recommended.
1. Gerdes C, Akkermann O, Krüger VGerdes A, Gerdes B. Incarceration of Meckel’s diverticulum in a leftparaduodenalTreitz’ hernia.World J Clin Cases. 2015; 3: 732-735.
2. Pantongrag-Brown L, Levine MS, Buetow PC, Buck JL, ElsayedAM. Meckel’s enteroliths: clinical, radiologic, and pathologic findings. AJR Am J Roentgenol. 1996; 167: 1447-1450.
3. Pujar VC, Joshi SS. Littré hernia: A surgicalsurprise. J SciSoc. 2015; 42: 198-200.
4. Sinha R. Bowel obstruction due to Littre hernia: CT diagnosis. Abdom Imaging. 2005; 30: 682-684.
5. Moorthy SN, Arcot R. In a ileal diverticulum (Meckel’sdiverticulum) – Gastric perforation: Report of a fatal case. Int J Morphol. 2010; 28: 1273-1276.
6. Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P. Littre hernia: Surgical anatomy, embryology, andtechnique of repair. Am Surg. 2006; 72: 238-243.
7. Racy M, Ramesh S. Littré meets de Garengeot: Meckel’sdiverticulum and appendix in a femoral hernia.Ann R Coll Surg Engl. 2013; 95: e97-e98.
8. Messina M, Ferrucci E, Meucci D, Di Maggio G, Molinaro F, Buonocore G. Littre’shernia in newborn infants: Report of twocases. Pediatr Surg Int. 2005; 21: 485-487.
9. Biel A, Vilallonga R, López-de-Cenarruzabeitia I, Rodríguez N, Armengol M. Littré s hernia: unusual find in inguino-scrotal hernial repair. Rev Esp Enferm Dig. 2010; 102: 506-507.
10. John J, Pal K, Singh VP. Perforated Meckel’s diverticulum causing giant pseudo cyst and secondary appendicitis. Indian Pediatr. 2006; 43: 988-990.

FILE - Dr. Anthony Fauci speaks during the presentation of his book “On Call” at Lincoln Theatre Friday, June 21, 2024, in Washington. ( AP Photo/Jose Luis Magana, File)

- Copy Link copied
Dr. Anthony Fauci, the former top U.S. infectious disease expert, spent time in the hospital after being infected with West Nile virus and is now recovering at home, a spokesperson confirmed Saturday.
Fauci is expected to make a full recovery, the spokesperson said on condition of anonymity due to security concerns.
West Nile virus is commonly spread through the bite of an infected mosquito. While most people don’t experience symptoms, about 1 in 5 can develop a fever, headache, body aches, vomiting, diarrhea, or rash, according to the Centers for Disease Control and Prevention. About 1 out of 150 infected people develop a serious, sometimes fatal, illness.
CBS News’ chief medical correspondent, Dr. Jonathan LaPook, wrote in a social media post that he spoke Saturday with Fauci, who said he was likely infected from a mosquito bite that he got in his backyard.
“Dr. Fauci was hospitalized about ten days ago after developing fever, chills, and severe fatigue,” the post on X said. It said Fauci spent a week in the hospital.
As chief White House medical adviser, Fauci was the public face of the U.S. government during the COVID-19 pandemic, a role that made him both a trusted voice to millions and also the target of partisan anger. He left the government in 2022 but was back before Congress in June to testify as part of Republicans’ yearslong investigation into the origins of COVID-19 and the U.S. response to the disease.
Fauci last summer joined the faculty at Georgetown University as a distinguished university professor.
There are no vaccines to prevent West Nile, or medicines to treat it. As of Aug. 20, the CDC had recorded 216 cases in 33 states this year. It’s best prevented by avoiding mosquito bites.
Thompson reported from Buffalo, N.Y.


IMAGES
COMMENTS
Case presentation: A 4-year-old child was brought to the medical clinic by her mother with a swelling complaint in the right inguinal region. Following clinical diagnosis and imaging tests, an indirect inguinal hernia was found to be present. It was decided to perform surgery on the child, and he was taken to the operating room and given general anesthesia. An incision was made on the right ...
Presentation of case A 87-year-old male presented in the emergency department due to a persistent right inguinal pain. Clinical examination revealed a tender right groin mass. Under the diagnosis of an right inguinal hernia, an operation was taken. Intraoperatively, an inflamed appendix and a part of the cecum were found in the hernia sac. The operation was completed with an ileocecal ...
Presentation of case A 59-year-old male with a history of a previously reducible right inguinal hernia presented to the Emergency Department with acute abdominal pain, right groin mass. Computed tomography (CT) confirmed a right incarcerated inguinal hernia with herniated loops of bowel within the right inguinal region.
Pantaloon hernia is an uncommon variety of inguinal hernia that may rarely present with two distinct inguinal swellings. Most of these hernias are identified intraoperatively. Misidentification, incomplete ligation of the sac and a missed small indirect sac of saddle bag hernia during surgery are the common causes of recurrence.
Despite recent advances in hernia repairs, the recurrence rates of hernias did not significantly diminished, even after the introduction of meshes. The aim of this article is to report a case of a ventral incisional hernia in a 37-year-old man and its successful treatment with a procedure known as the Alcino-Lázaro technique repair.
Case presentation In this paper, the case of a 39-year-old patient with left paraduodenal hernia will be presented. He arrived in the emergency department with sudden onset of abdominal pain. The diagnosis was established using computed tomography and an open surgical procedure was successfully performed.
Inguinal Hernia - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. An inguinal hernia occurs when abdominal contents, such as fat or part of the small intestine, bulge through a weak area in the lower abdominal muscles. The patient presented with a 5 cm bulging mass in their right inguinal area. Physical exam found ...
THE WHITE ARMY Comprehensive Clinical Class INGUINAL HERNIA Clinical Case Presentation by Ms.Rekha S, BGSGIMS, Bengaluru.
Background Vasitis or inflammation of the vas deferens is a rare condition, and few case reports with computed tomography images have been published since 1980. Case presentation A 50-year-old man presented with severe right inguinal and lower abdominal pain. Initial diagnosis at the emergency department was incarcerated or strangulated inguinal hernia. The computed tomography scan revealed ...
Hernias Clinical Cases Presentation Free Google Slides theme, PowerPoint template, and Canva presentation template How do you know if you've developed a hernia? What are the risk factors? Can they be prevented or treated? Is surgery involved?
#ComprehensiveClinicalClassBilateral Inguinal Hernia Clinical case presentation by Ms. Ashmita Jain, 4th year MBBS, Seth G S Medical College and KEM Hospital...
Obturator hernia, protrusion of abdominal content through the obturator foramen, is a rare type of abdominal wall hernia. Late patient presentation is associated with significant morbidity and mortality. We present rare case of obturator hernia causing small bowel obstruction in a 65-year-old-female patient. She presented with crampy abdominal ...
Hernia arising from obturator canal is rare and it contributes to about less than 1% of incidence of all hernias. Diagnosing an obturator hernia clinically is a challenging one and nearly impossible. These hernias usually present as an intestinal obstruction as more than 50% of obturator hernias goes in for strangulation. Here, we report an unusual presentation of an obturator hernia in a 70 ...
Popular Audio original "Cassette-Clinics" since 1981, Revised and updated. The ideal case presentations in Surgery. Written and recorded by Dr Ghanashyam Vai...
Morgagni Hernia is a congenital diaphragmatic hernia but can rarely present in adults. It occurs due to a congenital defect in the development of the diaphragm. Here we present a case of symptomatic Morgagni hernia diagnosed in a 53 years' female.A ...
CASE PRESENTATION HERNIA 1.pdf - Free download as PDF File (.pdf), Text File (.txt) or view presentation slides online. This document presents a case of an 84-year-old man with a left inguinal hernia that has been present for one year without pain or other symptoms. On examination, a 4x3x2 cm reducible swelling was found in the left groin that increased in size with coughing. Based on the ...
THE WHITE ARMYClinical case presentation of Inguinal HerniaPresented by Dr.Koushik, 2nd Year MS General Surgery, AGMC, Agartala.Mentor: Prof. Sriram Bhat, HO...
Biel et al. performed wide-V wedge resection in a case with MD which was detected during elective inguinal hernia surgery [9,10]. Similarly, our case underwent wedge resection. In conclusion, this report highlights that the detection of MD in the hernia sac during elective inguinal hernia surgery is rare and resection of MD is recommended.
A spokesperson says Dr. Anthony Fauci spent time in the hospital with a case of West Nile virus and is now recovering at home. He is expected to make a full recovery. ... FILE - Dr. Anthony Fauci speaks during the presentation of his book "On Call" at Lincoln Theatre Friday, June 21, 2024, in Washington. ( AP Photo/Jose Luis Magana, File)
#ComprehensiveClinicalClassClinical case presentation by Mr.O Neil Akash Biswas, St Johns Medical College, BengauruMentor: Dr Srikantaiah Hiremath, Associate...
Making their case for change the Northern Trust said while there will be greater surgical activity in Antrim they have recently invested in Causeway with the new ambulatory unit and the move would ...