
Language/Idioma:
Case studies.
Use these four case studies to test your knowledge of OA in the context of real-world patient scenarios, which span the content covered in the other eight modules.
Case Study #1

Q1. What are Betty’s risk factors for OA?
A. Gender B. Age C. Weight D. Occupation E. All of the above
Rationale (E) Female sex is associated with an increased risk of OA, especially OA of the hand, foot, and knee. Advancing age is by far the most well-known risk factor for OA. Betty’s weight is also a risk factor, even though her OA symptoms are currently only present in her hands; there is research showing that obesity can increase the risk of hand OA. Certain occupations that involve repetitive motion of a joint, like sewing, can worsen OA symptoms.
On examination, both of Betty’s hands appear normal (e.g., no deformities and no visible signs of inflammation); however, Betty reports stiffness and pain (lasting for ~15-20 minutes) when she first wakes up and after resting for prolonged periods. She has not missed any days from work, but admits the pain is significantly worse compared to a year ago. When asked, Betty states she is looking for pain relief and fears the arthritis “will spread” to her other joints.
Q2. What points of information should be shared with Betty?
A. Education about OA B. Weight loss counseling C. Sample hand exercises D. Offer a referral to Occupational Therapy E. All of the above
Rationale (E): Providing Betty with education about OA and explaining that it does not “spread” is a good place to start. It is important, however, to identify Betty’s risk factors and explain the importance of self-management strategies. While weight loss may not appear relevant to hand OA and could be daunting for a patient who is obese, education on the importance of weight loss, even a modest 5-10 pounds, can significantly improve mobility and function as well as reduce pain and may even help prevent OA in other joints such as her knees. You can encourage Betty to engage in healthy eating habits as well as hand exercises. One simple suggestion to increase mobility is that while Betty is watching TV, for example, she opens and closes her hands 5-10 times when a commercial is played. You can offer to submit a referral to an occupational therapist who can evaluate her for splinting, suggest additional exercises for hands, and recommend joint protection strategies in addition to assistive devices. If you feel that Betty can handle additional information, consider giving her a handout that describes resources and programs available for adults with OA to support physical activity, weight loss, managing pain, self-care, social support, and medical care.
Q3. What drug therapy poses the least risk for Betty?
A. Topical capsaicin B. Oral NSAID C. Acetaminophen D. Glucosamine with chondroitin
Rationale (C): Given Betty’s age as well as her history of hypertension and diabetes, an NSAID should be avoided as first-line therapy. Neither glucosamine nor chondroitin will treat her acute pain and the benefit of these agents in OA is unsubstantiated. Alternatively, APAP (< 3 grams per day) may be a safe and effective treatment option for Betty. While taking APAP, Betty should be counseled to avoid other APAP-containing products (e.g., cough and cold remedies or any product claiming to be “aspirin free”).
Case Study #2
John and his wife come in for a primary care visit following his hospital discharge. John is a 70-year-old man who is slightly overweight and has dyslipidemia, hypertension, and knee OA. He recently suffered a right cerebral vascular accident (CVA) due to atrial fibrillation that resulted in mild left hemiparesis. Prior to his stroke, he was prescribed a statin, ACE-inhibitor, diuretic, and calcium channel blocker.

In addition, John has new prescriptions for novel oral anticoagulant (NOAC) for secondary stroke prevention and an NSAID for knee pain, which was exacerbated during his post-CVA physical therapy sessions in the hospital. John has been mostly sedentary since he retired 5 years ago. In fact, other than physical rehabilitation in the hospital, he has not been physically active in years. He will begin outpatient physical therapy tomorrow for post-CVA rehabilitation.
Q1. What should be your primary concern?
A. Assessing whether John is able to take care of himself at home B. Addressing a drug interaction C. Submitting a referral for occupational therapy D. Recommending community-based physical activity programs
Rationale (B): Given the significance of the drug interaction between the NSAID and NOAC, this should be your primary concern. While an oral NSAID may provide pain relief for his knee OA, John’s age, co-morbidities, and concomitant drug therapy makes an oral NSAID relatively contraindicated. You learn that a trial of acetaminophen at a dose of 3 grams per day was not helpful in relieving Johns’ increased knee pain, so you could consider a topical NSAID. While these drugs carry the same black box warnings as oral NSAIDs, research has shown that the drug interactions with the NOAC, ACE-inhibitor, and diuretic are reduced; thereby, reducing the risk of bleeding and acute renal failure.
Q2. What non-pharmacologic treatment modalities should be recommended?
A. Weight loss B. Reduce periods of physical inactivity C. Community-based physical activity programs D. All of the above
Rationale (D): It would be important to encourage John to lose even a minimal amount of weight through improved diet and increased physical activity. Reducing his periods of inactivity will also help with his knee OA pain, as sustained periods of rest can worsen OA symptoms; therefore, promoting simple activity (e.g., every 20-30 minutes) may reduce OA pain and stiffness. You can also encourage him to discuss specific exercises with his outpatient physical therapist that will target the OA in his knee; the PT can give him exercises to do on his own at home. There are also many community programs designed specifically for patients with OA that John could transition to when his PT sessions are complete.
Case wrap up and recommendations:
Now that John is home, you will likely need to help in the coordination of care by advising continued therapy with physical therapy or cardiac rehabilitation and helping him find ways of staying physically active after therapy concludes. You can also provide ongoing coaching on simple ways to increase activity around the home and to manage his weight through his diet. It might be helpful to refer him to a registered dietitian. Because of the impact of his stroke, John is at risk for falls; therefore, promotion of safety is paramount. You can encourage John that his participation in physical activity will not only help improve his OA symptoms and hypertension but will also help him strengthen his lower body to prevent falls which could cause further limitations and disability. Periodic reassessment should also take place to evaluate his current non-drug and drug therapy regimens.
Case Study #3

Q1. What are Emma’s risk factors for developing OA?
A. Having had a knee injury B. Being female C. Being overweight D. All of the above
Rationale (D): Emma has a combination of modifiable and non-modifiable risk factors for developing OA. The non-modifiable risk factors include being female and having a prior injury. Emma’s modifiable risk factor is being overweight.
Q2. What strategies would best help Emma reduce her pain and slow the progression of OA?
A. Lose weight and increase physical activity B. Oral or topical NSAIDs C. Intraarticular corticosteroid injection D. Nothing; knee pain is inevitable with aging, and she should learn to live with it.
Rationale (A): In Emma’s case, losing weight is going to help reduce her OA symptoms significantly. A 10-pound weight loss can reduce the amount of knee joint loading by 40 pounds. Increasing physical activity is definitely recommended, too; it reduces pain, strengthens muscles, helps prevent the progression of OA and is an important part of a weight loss program. Emma could use acetaminophen when she has increased pain, but she should be cautioned to avoid cold or cough remedies also containing acetaminophen. Emma can also be encouraged that OA pain is not inevitable despite her age and prior sports history and that with proper management, she can return to a pain-free lifestyle.
Q3. What might it look like to use the 5 As model with Emma to discuss her weight? The 5 As model guides you to: Ask→ Assess→ Advise→ Agree→ Assist.
A. You ask Emma to increase her physical activity because you determined that she is obese based on her BMI and because she reports being mostly sedentary on the assessment form. You recommend that she perform moderate physical activity 150 minutes per week, and you set this as her SMART goal, to which she agrees. You recommend gyms in the area that she could join. B. You ask Emma if she would like to be a healthier weight. You suggest that increased physical activity and nutrition counseling help many patients, and advise her to do both. You refer her to a physical therapist who can help her with her knee pain and develop an appropriate physical activity program. You also refer her to a registered dietitian. C. You ask Emma if she has concerns about her weight, and she says she does and that she would like to be a healthier weight. You examine her chart again and note that she commonly eats fast foot and is mostly sedentary. You suggest increased physical activity and nutrition counseling, and ask her which of these modifications is possibly achievable for her now. Emma thinks diet change is possible, so you help her set a SMART goal to improve her diet and refer her to a registered dietitian. D. You ask Emma if it would be alright if you discussed her weight, and she states that she would like to learn how to achieve a healthy weight. Based on information you learned from her chart and her assessment form that she completed, you tell her she needs to be more physically active and to change her diet to lose weight. You advise her to keep a food journal, and you tell her that diet change is an achievable SMART goal for her. You refer her to a registered dietitian.
Rationale (C): Ask : Ask if Emma would be willing to talk to you about her weight. Does she have concerns about her weight? If she answers yes to these questions, then proceed. Assess : You notice in Emma’s chart that her weight gain really escalated after the birth of her second child a couple of years ago, and from her answers on the patient information form, you see that she is getting less than 150 minutes of moderate to strenuous exercise per week. Ask Emma about other contributing factors such as diet, sleep, and depression. Advise : You can tell that Emma knows the risks of being overweight on her cardiovascular health and her chance of developing diabetes. Tell her that she has two major risk factors for osteoarthritis (OA): excess weight and previous knee injury and that her knee pain could be from OA. Let her know that she is 2-4 times more likely to develop OA because of her previous knee injury. It could also help Emma to hear that every pound of weight she loses, would mean 4 pounds less of pressure on her knee joints. Offer Emma some options for weight loss strategies (increased physical activity, nutrition counseling, food journaling, etc) and see which she thinks is most realistic right now. Agree : If Emma is willing and ready, help her set 1-2 SMART goals (Specific, Measurable, Achievable, Realistic, Time-bound) around increasing her physical activity and/or addressing her diet or sleep habits. Assist : If appropriate, ask Emma if she would like a referral to see a nutrition counselor. It might also be beneficial for Emma to see a Physical Therapist or Sports Medicine professional to get help developing a neuromuscular training program that includes strengthening, balance, and plyometric exercises; this will help her prevent future injury to her knees. These professionals could also fit her for a knee brace if appropriate. You can ask Emma if she needs any community resources for fitness programs. Finally, make a plan to follow-up with Emma. If your practice has a chronic care manager, schedule her to have a series of phone calls with the case manager. Offer to see her back for a follow-up appointment with you in 3-6 months.
Case Study #4

Q1. What additional evaluation is needed to confirm the etiology of her knee pain?
A. Bilateral standing knee x-rays B. Erythrocyte sedimentation rate C. Serum uric acid level D. MRI of the right knee E. None of the above
Rationale (E): The diagnosis of OA is generally a clinical one and can be made in this patient with very typical history without additional lab or imaging studies.
Maria was diagnosed with type II diabetes 2 years ago and had a HbA1c of 8% last month. She also has hypertension, high cholesterol, chronic kidney disease, and mild COPD from remote smoking. Her medications include metformin, glyburide, pravastatin, losartan, and an inhaler. She previously took acetaminophen but stopped as it was not helping her joint pain.
Q2. What intervention is most likely to improve her knee pain with minimal risk?
A. Oral or topical NSAIDs B. Intra-articular corticosteroid injection C. Increased physical activity D. Initiate scheduled acetaminophen
Rationale (C): Physical activity is the most important intervention in this case, not only because it is the most likely to lead to substantial improvements in knee pain and function (IDEA Trial1), but also because it can improve management of her other comorbid conditions. Topical NSAIDs might be a useful adjunct, but additional information about her CKD would be needed; oral NSAIDs are likely contraindicated given her age and comorbidities. Intra-articular corticosteroid could provide temporary relief for the right knee, but not the left, and has the potential to increase her blood sugar. She has already tried acetaminophen in therapeutic doses without help, and given the minimal efficacy of this agent, additional trials are unlikely to be of benefit.
On examination, Maria’s resting blood pressure is 150/95, heart rate is 90, and respiratory rate is 14. Her BMI is 32 kg/m2. She is in no acute distress, and examination of her head, neck, eyes, and ENT is unremarkable. She has an intermittent expiratory wheeze, but normal work of breathing. Her cardiovascular exam is unremarkable, as is her GI evaluation. There is no edema in her extremities. Her musculoskeletal examination demonstrates scattered non-painful Heberden’s nodes, mild thumb base squaring, but otherwise normal hands, wrists, elbows, and shoulders. Hip range of motion is preserved, there is no sacroiliac or trochanteric tenderness. She endorses tenderness to palpation of the medial joint lines of both knees, worse on the right. There is a trace effusion of the right knee, none on the left. She has full ROM of both knees but endorses some stiffness; crepitus is noted on the right. The ankles and feet are unremarkable. She does not have diffuse muscular tenderness.
Q3. For which of her conditions would increased physical activity be beneficial?
A. Symptomatic osteoarthritis B. Type II diabetes C. Chronic kidney disease D. COPD E. All of the above
Rationale (E): Physical activity is a mainstay of management of all of these conditions and is the most important recommendation for management of her osteoarthritis.
Case wrap up and recommendations
Increased physical activity is recommended to the patient, recognizing that while physical activity is likely to benefit many of this patient’s chronic medical comorbidities, she may experience difficulty in engaging in increased activity due to these conditions. For example, knee pain or shortness of breath may limit walking endurance when walking is recommended for improved diabetes management. It is essential to inventory the comorbid conditions that may impact a patient’s ability to follow physical activity recommendations and to tailor those recommendations accordingly. In this case, a program of aquatic therapy, supervised physiotherapy, or pulmonary rehabilitation could assist with getting started, followed by a graded land-based program, graded walking program, or group activity class (based on preferences and local resources). The key is to begin slowly with manageable recommendations (i.e., not to recommend 150 minutes per week at the first visit) and to make incremental gains up to a goal agreed upon by both the provider and the patient, recognizing that any increase in physical activity is likely to provide wide-ranging benefits. Additional medical management and adjunctive therapies can still be used, with the aim of assisting the patient to reach her physical activity goals while minimizing symptoms.
- Messier SP, Mihalko SL, Legault C, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310(12):1263-1273.
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 27-1: Approach to the Patient with Joint Pain - Case 1
Adam S. Cifu
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Chief complaint, constructing a differential diagnosis.
- RANKING THE DIFFERENTIAL DIAGNOSIS
- MAKING A DIAGNOSIS
- CASE RESOLUTION
- Full Chapter
- Supplementary Content
Mrs. K is a 75-year-old woman who complains of a painful left knee.
Figure 27-1.
Diagnostic approach: joint pain.

The causes of joint pain range from common to rare and from bothersome to life-threatening. Even the most benign causes of joint pain can lead to serious disability. The evaluation of a patient with joint pain calls for a detailed history and physical exam (often focusing on extra-articular findings) and occasionally the analysis of joint fluid, serologies, and radiologic tests.
The differential diagnosis of joint pain can be framed with the use of 3 pivotal questions. First, is a single joint or are multiple joints involved (is the joint pain monoarticular or polyarticular)? If the pain involves just 1 joint, the next question is, is the pain monoarticular or extra-articular? Although this distinction may seem obvious, abnormalities of periarticular structures can mimic articular disease. Finally, are the involved joints inflamed or not? Further down the differential, the acuity of the pain may also be important.
Figure 27-1 shows a useful algorithm organized according to these pivotal points. Because periarticular joint pain is almost always monoarticular, the first pivotal point differentiates monoarticular from polyarticular pain. Periarticular syndromes are discussed briefly at the end of the chapter.
The differential diagnosis below is organized by these 3 pivotal points as well. When considering both the algorithm and the differential diagnosis, recognize that all of the monoarticular arthritides can present in a polyarticular distribution, and classically polyarticular diseases may occasionally only affect a single joint. Thus, this organization is useful to organize your thinking but should never be used to exclude diagnoses from consideration.
Monoarticular arthritis
Inflammatory
Nongonococcal septic arthritis
Gonococcal arthritis
Lyme disease
Crystalline
Monosodium urate (gout)
Calcium pyrophosphate dihydrate deposition disease (CPPD or pseudogout)
Noninflammatory
Osteoarthritis (OA)
Avascular necrosis
Polyarticular arthritis
Rheumatologic
Rheumatoid arthritis (RA)
Systemic lupus erythematosus (SLE)
Psoriatic arthritis
Other rheumatic diseases
Bacterial endocarditis
Hepatitis B
Postinfectious
Rheumatic fever
Noninflammatory: OA
Mrs. K’s symptoms started after she stepped down from a bus with unusual force. The pain became intolerable within about 6 hours of onset and has been present for 3 days now. She otherwise feels well. She reports no fevers, chills, dietary changes, or sick contacts.
Get Free Access Through Your Institution
Pop-up div successfully displayed.
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
- Case Report
- Open access
- Published: 16 September 2008
A woman living with osteoarthritis: A case report
- Jane C Richardson 1 ,
- Christian D Mallen 1 , 2 &
- Helen S Burrell 1
Cases Journal volume 1 , Article number: 153 ( 2008 ) Cite this article
23k Accesses
Metrics details
Osteoarthritis is a common condition that is typically associated with older adults. Other causes of osteoarthritis, such as those cases resulting from childhood Perthes disease, can affect younger people and frequently have a major impact on the lives of those affected. This case report describes the experiences of one patient with osteoarthritis, using examples of her poetry to illustrate her social, psychological and emotional transformation.
Introduction
Osteoarthritis (OA) is the most common joint disease and one of the most widespread of all chronic conditions managed in general practice. Whilst the prevalence of OA increases with age, a significant minority of adults experience symptoms earlier in life. Most cases of osteoarthritis are not extraordinary, yet the individual experiences of those affected provide a unique opportunity for health care practitioners and researchers to more fully understand the impact that common conditions have on their patients.
This case report was triggered by a patient (HB) wanting to tell her story. The importance of narrative in medicine is increasingly being recognised as a powerful tool that can strengthen clinical practice and help to create an alliance with patients. This alternative case report, written by a researcher (JCR), a general practitioner (CDM) and a patient (HB), presents a fairly typical case of a younger adult with osteoarthritis. However, rather than presenting laboratory results or X-ray findings, we use Helen's poems to highlight her experiences and her journey with osteoarthritis.
Case presentation
Helen is 46 years old and has generalised osteoarthritis. Her hips and hands are the most severely affected joints. Helen's health problems started at the age of 11, following a fall on a cross-country run. She consulted her general practitioner and the accident unit multiple times with increasing levels of pain and disability before she was eventually diagnosed with Perthes disease, a diagnosis that has had a huge impact on her subsequent life. Over the years Helen has tried the full range of pain medications. A review of her past prescriptions reveals trials of over 15 different analgesics and anti-inflammatory drugs, covering the full range of the analgesic ladder. Her current medication, oxycodone, has so far been the best choice, optimising pain relief whilst minimising side effects. Helen continues to be under the care of local orthopaedic surgeons, who are contemplating further revisions to her failed total hip replacement. Helen remains independent and self-caring despite deterioration in her levels of pain and physical functioning.
Helen trained as a radiographer, but following the failure of a hip replacement she became a wheelchair user, which was not felt to be compatible with her job. This loss has had significant impact on Helen's identity: she describes it as being ' picked up from one life, where I could focus on me and what I wanted to happen, and put in another, where someone else was in control '. The issues of identity and social roles are key for Helen, in knowing how to define herself – 'A m I disabled? a woman? a disabled woman? a carer ?' – and in the huge loss of identity caused by loss of her job, associated financial security and her increasing disabilities. This meant radical changes to her social life, independence, choices, freedom of movement, interests and hobbies.
The nature of Helen's condition does not mean she has necessarily lost all other social roles. Helen's parents live close to her and suffer from a number of physical and mental health conditions. For Helen, being her parents' main carer is a source of positive identity and pride, although it also means she can be called to provide physical or emotional help at any time during the day or night. Her father's illness also meant that Helen took on some of his caring responsibilities, in looking after her elderly aunt who had dementia.
Relationships and friendships have been very important to Helen and have been affected by her condition. She had been engaged at age 21, shortly before a period of hospitalisation. The relationship ended, she felt, because of her depression during this period and her fiancé's lack of experience of dealing with such a situation. She describes the problems with actually meeting people with whom to have a relationship, but also the dilemma and difficulty of attempting to " build an equal partnership, when somebody does have to take on a carer's role ." She also describes conflict in relationships with people who had had disabilities since birth, both from their perspective, and from expectations of other people who thought she 'should' have a relationship with a non-disabled person.
Helen describes the process of learning " to become disabled ." An event she found helpful in this process was a disability awareness training course, because, " you're put into this situation but you don't get given a tablet to make you be disabled, ...to understand being disabled and impaired and 'all the rest of it"." This enabled her to write her own disability awareness course, including issues that were important to her as a woman and as a person who had acquired her disabilities.
Helen's relationship with her GP (CDM) is important to her, particularly as he is also her parents' GP and therefore has an understanding of the context in which she is managing her disability. She also feels strongly about the benefits of having a relationship with her GP in which she is seen as a person and is able to " be herself ", without being concerned that she is seen as a problem or that people are worrying about her.
We have presented a case of a woman with osteoarthritis secondary to Perthes disease in childhood. We have described her emotional, social and psychological transformation using her poetry to illustrate different life experiences. The notion of biographical disruption[ 1 ] can be used to describe the identity changes experienced by Helen. This 'breaking down' of one's life is eloquently described by Arthur Frank, a medical sociologist who has himself experienced critical illness: " What happens when my body breaks down happens not just to that body but also to my life, which is lived in that body. When the body breaks down, so does the life. Even when medicine can fix the body, that doesn't always put the life back together again ." [ 2 ] One response to biographical disruption is to attempt to repair the narrative of one's life[ 3 ]. Creativity, through poetry, writing or art, can be seen as one way of trying to make sense of this disruption. This type of creativity may be actively encouraged as part of a healing process [ 4 – 6 ], although Helen's poems were originally written solely for and by herself.
This is not a traditional case report, yet we believe that our approach can be equally as informative, by allowing doctors and researchers to more fully understand the impact a disease has on all aspects of their patient's lives.
Patient's perspective
Where have I gone?
Where's the woman who weighed less than 9 stone?
Who wore a dress size 12 and didn't need to wear shapeless clothes or jogging suits?
Who had shaped and tidy eyebrows that would complement her latest hair colour and style?
Whose painted nails, with manicured hands and feet, were perfect for holidays in the sun?
Where's the woman who had a vocation not just a job, but who exists on benefits, a step away from poverty?
Where's the woman who owned her own home that gave her safety and privacy, it was her pride and joy?"
Where's the woman whose hobbies include travel, gardening, decorating, furniture restoring, sewing, reading and studying at home?
Here I am and life before my impairment has gone, the only thing I can do is hold a pen with a special grip and writing is agony .
Where has she gone?
WHERE HAVE I GONE?
Do you see me?
How can you ever know me, when all you see is my chair?
My limitations are all you see and you say they complicate your life .
Will you ever see the deep pools of love in my eyes for you?
When you half close yours with pity and turn away from me .
The beating of my heart in expectation of your closeness is
quickly cooled by your fleeting hug or, worse, patting my shoulder .
I wait in anticipation remembering the taste and softness of
your kiss, you offer me a warm 'peck' on the cheek .
I smell your aftershave ... you say I smell clean!
I remember running my fingers through your hair ,
Ripping buttons off your shirt but that's difficult when you
stand behind me pushing my chair, we can't even hold hands anymore .
The power of my emotions makes me feel strong ,
Then I catch that pitying look in your eye ,
They die in my heart .
I do not speak, my smile fills my face but you will never know ...
You'll never see the real woman who is me
Who sits and is seen by the world framed by a wheelchair
Cut off emotionally just because I cannot stand or walk .
Thank you to those who take the time to listen to difficult and unclear speech, for you help us to know that if we persevere we can be understood
Thank you to those who walk with us in public places, ignoring stares and whispers from strangers, for in your friendship we find enjoyment, laughter and happiness
Thank you for never asking us to 'hurry up', but even more special is you don't snatch our tasks from us or offer 'Care' in such a way as to make us feel that we are still children, with no control and respect
Thank you for standing beside us when we enter new experiences and try new adventures
Though our success may be outweighed by our failure, the experience will stay with us forever and there will be many occasions when we surprise ourselves and maybe even you!
Thank you for asking for our help and expertise ,
As self-confidence and awareness come from being needed by you and others
Thank you for giving us respect
You acknowledge our value as experts in our fields and that we require to live with equality in society
We shouldn't have to ask or have laws to enforce it or remind you
Thank you for assuring us that the things that make us individuals are not our medical impairments, as everyone has those and they don't define ONE'S SELF, it's people's attitudes that create barriers that exclude us from you .
Treat us as we treat you .
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Bury M: Chronic illness as biographical disruption. Sociology of Health & Illness. 1982, 4: 167-182. 10.1111/1467-9566.ep11339939.
Article CAS Google Scholar
Frank AW: At the will of the body. 1992, Houghton Mifflin
Google Scholar
Frank AW: The Wounded Storyteller. Explore (NY). 2005, Chicago: Chicago University Press, 1 (2): 142-143.
http://www.lapidus.org.uk : aims to promote the use of creative writing for health and wellbeing.
Sampson F: The Healing Word. The Poetry Society. 1999
Hatem D, Rider EA: Sharing stories: narrative medicine in an evidence-based world. Patient Educ Couns. 2004, 54 (3): 251-253.
Article PubMed Google Scholar
Download references
Author information
Authors and affiliations.
Arthritis Research Campaign National Primary Care Centre, Keele University, Keele, Staffs, ST5 5BG, England
Jane C Richardson, Christian D Mallen & Helen S Burrell
Kingsbridge Medical Practice, Kingsbridge Avenue, Clayton, Newcastle-under-Lyme, Staffordshire, ST5 3BR, England
Christian D Mallen
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jane C Richardson .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
"JCR interviewed HSB and wrote the article based on the interviews. CDM wrote the medical aspects of the article and helped with the drafting of the article. HSB wrote the patient perspective section. HSB and CDM helped revise the manuscript".
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Richardson, J.C., Mallen, C.D. & Burrell, H.S. A woman living with osteoarthritis: A case report. Cases Journal 1 , 153 (2008). https://doi.org/10.1186/1757-1626-1-153
Download citation
Received : 12 August 2008
Accepted : 16 September 2008
Published : 16 September 2008
DOI : https://doi.org/10.1186/1757-1626-1-153
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Osteoarthritis
- Disable Woman
- Perthes Disease
- Biographical Disruption
Cases Journal
ISSN: 1757-1626
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Sacroiliac joint dysfunction: a case study
Affiliation.
- 1 US Army, Nurse Corps, Kailua, HI, USA.
- PMID: 21422895
- DOI: 10.1097/NOR.0b013e31820f513e
Pain is a widespread issue in the United States. Nine of 10 Americans regularly suffer from pain, and nearly every person will experience low back pain at one point in their lives. Undertreated or unrelieved pain costs more than $60 billion a year from decreased productivity, lost income, and medical expenses. The ability to diagnose and provide appropriate medical treatment is imperative. This case study examines a 23-year-old Active Duty woman who is preparing to be involuntarily released from military duty for an easily correctable medical condition. She has complained of chronic low back pain that radiates into her hip and down her leg since experiencing a work-related injury. She has been seen by numerous providers for the previous 11 months before being referred to the chronic pain clinic. Upon the first appointment to the chronic pain clinic, she has been diagnosed with sacroiliac joint dysfunction. This case study will demonstrate the importance of a quality lower back pain assessment.
PubMed Disclaimer
Similar articles
- [Sacroiliac joint dysfunction presented with acute low back pain: three case reports]. Hamauchi S, Morimoto D, Isu T, Sugawara A, Kim K, Shimoda Y, Motegi H, Matsumoto R, Isobe M. Hamauchi S, et al. No Shinkei Geka. 2010 Jul;38(7):655-61. No Shinkei Geka. 2010. PMID: 20628193 Japanese.
- Stabilization of the sacroiliac joint. Shaffrey CI, Smith JS. Shaffrey CI, et al. Neurosurg Focus. 2013 Jul;35(2 Suppl):Editorial. doi: 10.3171/2013.V2.FOCUS13273. Neurosurg Focus. 2013. PMID: 23829837
- Impairment-based examination and disability management of an elderly woman with sacroiliac region pain. Godges JJ, Varnum DR, Sanders KM. Godges JJ, et al. Phys Ther. 2002 Aug;82(8):812-21. Phys Ther. 2002. PMID: 12147010
- The sacroiliac joint: an underappreciated pain generator. Daum WJ. Daum WJ. Am J Orthop (Belle Mead NJ). 1995 Jun;24(6):475-8. Am J Orthop (Belle Mead NJ). 1995. PMID: 7670870 Review.
- 13. Sacroiliac joint pain. Vanelderen P, Szadek K, Cohen SP, De Witte J, Lataster A, Patijn J, Mekhail N, van Kleef M, Van Zundert J. Vanelderen P, et al. Pain Pract. 2010 Sep-Oct;10(5):470-8. doi: 10.1111/j.1533-2500.2010.00394.x. Pain Pract. 2010. PMID: 20667026 Review.
- Biomechanics of the Sacroiliac Joint: Surgical Treatments. Joukar A, Kiapour A, Elgafy H, Erbulut DU, Agarwal AK, Goel VK. Joukar A, et al. Int J Spine Surg. 2020 Jun 30;14(3):355-367. doi: 10.14444/7047. eCollection 2020 Jun. Int J Spine Surg. 2020. PMID: 32699758 Free PMC article.
- Comparison of the costs of nonoperative care to minimally invasive surgery for sacroiliac joint disruption and degenerative sacroiliitis in a United States commercial payer population: potential economic implications of a new minimally invasive technology. Ackerman SJ, Polly DW Jr, Knight T, Schneider K, Holt T, Cummings J Jr. Ackerman SJ, et al. Clinicoecon Outcomes Res. 2014 May 24;6:283-96. doi: 10.2147/CEOR.S63757. eCollection 2014. Clinicoecon Outcomes Res. 2014. PMID: 24904218 Free PMC article.
- Comparison of the costs of nonoperative care to minimally invasive surgery for sacroiliac joint disruption and degenerative sacroiliitis in a United States Medicare population: potential economic implications of a new minimally-invasive technology. Ackerman SJ, Polly DW Jr, Knight T, Schneider K, Holt T, Cummings J. Ackerman SJ, et al. Clinicoecon Outcomes Res. 2013 Nov 20;5:575-87. doi: 10.2147/CEOR.S52967. eCollection 2013. Clinicoecon Outcomes Res. 2013. PMID: 24348055 Free PMC article.
- Minimally invasive sacroiliac joint fusion: one-year outcomes in 40 patients. Sachs D, Capobianco R. Sachs D, et al. Adv Orthop. 2013;2013:536128. doi: 10.1155/2013/536128. Epub 2013 Aug 13. Adv Orthop. 2013. PMID: 23997957 Free PMC article.
- Sacroiliac Joint Arthrodesis-MIS Technique with Titanium Implants: Report of the First 50 Patients and Outcomes. Rudolf L. Rudolf L. Open Orthop J. 2012;6:495-502. doi: 10.2174/1874325001206010495. Epub 2012 Nov 30. Open Orthop J. 2012. PMID: 23284593 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Wolters Kluwer

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Case Report
- Open access
- Published: 15 August 2024
Arthroscopic reduction and hollow screw internal fixation for Eyres Type IIIA scapular coracoid fracture: a case report
- Weizhao Xie 1 na1 ,
- Dahai Hu 1 na1 ,
- Huige Hou ORCID: orcid.org/0009-0008-7766-6560 1 &
- Xiaofei Zheng 1
BMC Musculoskeletal Disorders volume 25 , Article number: 645 ( 2024 ) Cite this article
12 Accesses
Metrics details
A coracoid process fracture combined with an acromioclavicular (AC) joint dislocation is an uncommon injury that typically causes significant pain and limits shoulder movement. Open reduction and internal fixation have been the traditional treatment approach. However, arthroscopic techniques are emerging as a promising alternative for managing these injuries.
Case representation
A 35-year-old woman presented with right shoulder pain following an accidental fall. Imaging studies revealed a coracoid process fracture along with an AC joint dislocation. The fracture was classified as an Eyres Type IIIA, which warranted surgical intervention. Our team performed arthroscopic coracoid fracture reduction and internal fixation surgery, as well as AC joint dislocation repair using Kirschner wires. Six months after surgery, the patient demonstrated a satisfactory functional outcome with complete bone healing.
This case report highlights the potential of arthroscopic reduction and fixation as a novel treatment option for fractures of the coracoid base.
Peer Review reports
Scapular coracoid fractures are uncommon, accounting for only 0.5–1.0% of all fractures and representing just 3–13% of scapular fractures themselves [ 1 , 2 ]. These fractures can be classified into different types depending on their location. Traditionally, treatment involved open reduction and internal fixation of the displaced coracoid. The goal was to achieve either an anatomical reduction or a non-anatomical reduction. However, advancements in arthroscopic technology have made it possible to perform arthroscopic reduction and internal fixation for fractures at the base of the coracoid process [ 3 ]. This case report describes an Eyres Type IIIA fracture treated with osteosynthesis using an arthroscopic approach.
Fourteen days after an accidental fall, a 35-year-old woman presented with right shoulder pain. She described the pain as a dull ache located on the medial aspect of the joint. The pain worsened with any movement of the shoulder, and she also reported limitations in her right shoulder mobility.
Digital radiographs of the right shoulder joint, obtained at a local hospital, suggested a dislocation of the right acromioclavicular (AC) joint. However, no treatment was initiated at that facility.
Specialist physical examination
On physical examination, the right shoulder joint exhibited mild swelling without any visible deformity. However, there was significant tenderness on palpation near the medial aspect of the glenohumeral joint. Additionally, abnormal movement was detectable at this tender point. The active range of motion in the right shoulder joint was limited: flexion: 30°, extension: 15°, abduction: 40°, internal rotation: 5°, and external rotation: 5°. Due to the patient’s pain, the remainder of the physical examination was not completed.
Sensation in both upper limbs remained largely normal, and peripheral movement and circulation were unimpaired. Preoperative imaging is presented in Fig. 1 . Based on the clinical findings, a preoperative diagnosis of right coracoid process fracture and right AC joint dislocation was established.

A : The preoperative shoulder joint DR shown like this. Acromioclavicular joint dislocation and coracoid fracture area were indicated by the arrow. B : CT 3D reconstruction image of the coracoid fracture as seen in the main view. C : CT 3D reconstruction of the coracoid fracture seen from the top view
Intraoperative findings
Following general anesthesia with a brachial plexus block, the patient was positioned in a left lateral decubitus position with a 30° posterior tilt. The right upper limb was then externally rotated and secured in a position of forward flexion. Preoperative markings were made on the bony landmarks of the acromion, AC joint, and scapular spine.
A single incision, 2 cm below the posterolateral corner of the acromion and 1 cm medial, was created. Through this incision, a trocar was inserted towards the coracoid process to establish a standard posterior arthroscopic approach. An additional incision was made midway between the coracoid process and the acromion to create the anterior portal for shoulder arthroscopy.
Both standard anterior and posterior portals were used to visualize the glenohumeral joint. After entering the joint, the coracoacromial ligament was followed anteriorly to explore the coracoid process. A plasma knife was then used to meticulously dissect the surrounding synovium and attached tendons from the coracoid process.
Dissection continued until the superior surface of the coracoid base was fully exposed. Here, a fracture line with a displacement exceeding 3 mm was evident (Fig. 2 A). The area was further debrided to expose the inferior surface, ultimately achieving visualization of the superior, inferior, and lateral aspects of the coracoid base (Fig. 2 B).

A : The surrounding tissues were cleared to expose the fracture line at the base of the coracoid process under arthroscopy. B : Exposed the superior, inferior, and lateral aspects of the fracture line. The area indicated by the arrow is the fracture line
Surgical treatment plan
Through the posterior portal, a plasma knife and shaver were used to meticulously clear the synovium and fatty tissue around the coracoid process. Once a clear view of the superior aspect of the coracoid was obtained, the surgical approach was slightly widened.
Arthroscopy revealed an AC joint dislocation. Two Kirschner wires were strategically placed to temporally fix the dislocated joint. This facilitated the reduction of the fractured coracoid by minimizing resistance and creating favorable conditions for realignment.
Dissection continued until the base of the coracoid process was fully visualized under the arthroscope. The observed fracture displacement was consistent with the preoperative computed tomography (CT) reconstruction.
A suture was passed through the conjoint tendon superior to the coracoid process (Fig. 3 A and B). This suture served a dual purpose: securing the suture and utilizing the conjoint tendon to retract and mobilize the coracoid fragment.

A : During the operation, two K-wire needles were taken to fix the dislocated acromioclavicular joint, and the acromioclavicular joint was well reduced. B : The suture is inserted from the conjoint tendon to pull the fractured coracoid process under arthroscopy. C : The displaced coracoid process is pulled back to its original position by suture traction
Once anatomical reduction of the coracoid fracture was achieved (Fig. 3 C), two guide pins were strategically inserted through the coracoid process to stabilize the displaced bone (Fig. 4 A and B). Intraoperative confirmation ensured both anatomic reduction of the fracture fragments and stable guide pin fixation.

A : Intraoperative radiograph can be seen: after the reduction of the coracoid process is completed, two Guide Pins are placed to fix it. B : The direction of the two Guide Pins in vitro view is shown. C : The hollow screws were inserted along the Guide Pins, and the coracoid process is well reduced and fixed in place
Following guide pin placement, two hollow screws (diameter 3 mm, inner diameter 2.1 mm, length 36 mm and 32 m, Kaiwei Yierling) were inserted along the guide pin tracks. Post-screw insertion radiographs (Fig. 4 C) and arthroscopic visualization confirmed satisfactory fracture reduction (Fig. 4 C). The surgical procedure lasted approximately 150 min, with minimal blood loss (70 mL).
Postoperative Rehabilitation
For the first six weeks after surgery, the patient wore a sling to immobilize the affected shoulder. Restricted elbow flexion exercises were also initiated during this period. A physical therapist then guided the patient through a program of passive motion exercises for the shoulder joint with limited range.
At six weeks postoperatively, the range of motion in the shoulder joint was limited to 45° of abduction and 90° of forward flexion. Radiographs and CT scans confirmed bony union at the fracture site three months after surgery (Fig. 5 ).

A : CT of the shoulder joint showed that the coracoid fracture line was slightly blurred, and the fracture was initially healed (1 month postoperatively). B : CT of the shoulder joint showed that the fractured end of the coracoid process had healed significantly, and the fracture line had gradually disappeared (2 months postoperatively). C : Radiograph of the shoulder joint shows that the patient’s acromioclavicular joint is in place, and the coracoid fracture is healed(3 months postoperatively)
By the six-month follow-up, the patient’s range of motion had significantly improved, forward flexion: 150°, extension: 40°, abduction: 170°, internal rotation: 70°, and external rotation: 80°.
Discussion and conclusion
Current treatment guidelines for coracoid fractures recommend surgery for displaced fractures or those involving the shoulder’s superior suspensory complex [ 4 , 5 , 6 , 7 ]. Our patient’s Eyres Type IIIA coracoid fracture fulfilled these criteria. However, based on CT scans (Fig. 4 B and C) and arthroscopic visualization, the displacement was relatively minor. Therefore, we opted for arthroscopic reduction and internal fixation.
For fractures with severe displacement where arthroscopic reduction is not feasible, open surgery remains an option. Shariff et al [ 8 ]. suggest that most coracoid fractures can be managed conservatively without surgery, with intervention reserved for specific cases like athletes or patients with non-unions. Similarly, Caroline et al [ 9 ]. propose surgical indications including fracture displacement exceeding 1 cm on imaging, multiple disruptions, or persistent rotator cuff dysfunction. Both studies by Shariff et al. and Caroline et al. emphasize the importance of thorough preoperative assessment [ 8 , 9 ], highlighting the role of CT scans in guiding surgical planning.
Caroline et al [ 9 ]. suggest that AC joint dislocations with intact coracoclavicular ligaments may improve solely with coracoid process reduction, potentially avoiding AC joint fixation. However, our patient presented with a partial tear of this ligament, necessitating AC joint stabilization.
Current fixation techniques for AC joint dislocations include the Tight Rope technique and Kirschner wires [ 8 ]. While both hook plate and Tight Rope methods offer good fixation, they may have drawbacks such as longer surgery times and larger incisions, potentially increasing infection risk. Arthroscopic surgery itself carries a risk of intra-articular infection if complications arise.
Furthermore, the possibility of nonunion of coracoid process when coracoclavicular reconstruction (C-C reconstruction) is performed for coracoid process fractures can be one of the reasons for AC fixation with Kirschner wire [ 10 ]. Therefore, considering the advantages, we opted for Kirschner wire fixation for the AC joint.
This case highlights the potential of arthroscopy for treating a combined Eyres Type IIIA coracoid fracture and AC joint dislocation. The coracoid process plays a critical role in shoulder stability, forming part of the superior suspensory complex. It serves as an attachment site for several muscles (pectoralis minor, biceps brachii, and coracobrachialis muscles) and provides the origin for key ligaments (coracoclavicular, coracoacromial, coracohumeral, and superior transverse scapular). Additionally, vital neurovascular structures (brachial plexus nerves, axillary artery, and axillary vein) course near the deep surface of the pectoralis minor muscle [ 11 ].
These anatomical considerations make open surgical exposure of the coracoid base challenging, potentially risking damage to nearby structures. Arthroscopy offers a minimally invasive approach that overcomes these limitations. Utilizing both anterior and posterior portals, the surgeon can safely access the area around the glenohumeral joint with a plasma knife. This arthroscopic view allows for the meticulous removal of obstructing soft tissues, revealing the fracture line. The conjoint tendon above the coracoid can then be utilized for traction and reduction of the fractured segment.
Following reduction and internal fixation, an intraoperative radiograph confirmed the anatomical reduction of the coracoid process and proper placement of the implants. Over multiple follow-up visits within three months postoperatively, the patient’s progress aligned with the expected outcomes for arthroscopic treatment of coracoid base fractures.
The arthroscopic approach offers several advantages, including minimal tissue disruption, leading to faster recovery and reduced blood loss.
In conclusion, this case demonstrates the feasibility of arthroscopic treatment for fractures at the base of the coracoid process. Compared to traditional open reduction and internal fixation with a hook plate, as described by Zhang et al. [ 12 ], our arthroscopic approach with Kirschner wire fixation may minimize the size of the surgical wound and reduce the risk of infection. By three months postoperatively, the patient had regained near-normal shoulder function, and satisfactory outcomes were maintained at six-month follow-up. These findings suggest that arthroscopic treatment for coracoid process fractures with AC joint dislocation can achieve excellent clinical results. Further validation through multicenter, randomized controlled trials would strengthen this conclusion.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
Acromioclavicular
Coracoclavicular reconstruction
Computed tomography
van Doesburg PG, El Saddy S, Alta TD, van Noort A, van Bergen CJA. Treatment of coracoid process fractures: a systematic review. Arch Orthop Trauma Surg. 2021;141(7):1091–100.
Article PubMed Google Scholar
Rabbani GR, Cooper SM, Escobedo EM. An isolated coracoid fracture. Curr Probl Diagn Radiol. 2012;41(4):120–1.
Brusalis CM, Mizels J, Moverman MA, Chalmers PN. Symptomatic coracoid fracture Nonunion treated with arthroscopic reduction and suture Anchor fixation: a Case Report. JBJS Case Connect 2024, 14(1).
Eyres KS, Brooks A, Stanley D. Fractures of the coracoid process. J Bone Joint Surg Br. 1995;77(3):425–8.
Article CAS PubMed Google Scholar
Bartoníček J, Tuček M, Strnad T, Naňka O. Fractures of the coracoid process - pathoanatomy and classification: based on thirty nine cases with three dimensional computerised tomography reconstructions. Int Orthop. 2021;45(4):1009–15.
Thompson G, Van Den Heever A. Coracoid stress fracture in an elite fast bowler: description of a technique for CT-guided percutaneous screw fixation of coracoid fractures. Skeletal Radiol. 2019;48(10):1611–6.
Ruchelsman DE, Christoforou D, Rokito AS. Ipsilateral nonunions of the coracoid process and distal clavicle–a rare shoulder girdle fracture pattern. Bull NYU Hosp Jt Dis. 2010;68(1):33–7.
PubMed Google Scholar
Bishai SK, Ball GRS, Maceroni MR, Howard SD. Arthroscopic internal fixation of Coracoid fractures: Surgical technique guide. Arthrosc Tech. 2022;11(8):e1509–14.
Article PubMed PubMed Central Google Scholar
Passaplan C, Beeler S, Bouaicha S, Wieser K. Arthroscopic management of a coracoid fracture Associated with Acromioclavicular dislocation: technical note. Arthrosc Tech. 2020;9(11):e1767–71.
Furuhata R, Tanji A. Symptomatic Nonunion of the coracoid process following Osteosynthesis using a suture button for coracoid process and distal clavicle fracture: a Case Report. Am J Case Rep. 2024;25:e943108.
Galvin JW, Kang J, Ma R, Li X. Fractures of the Coracoid process: evaluation, management, and outcomes. J Am Acad Orthop Surg. 2020;28(16):e706–15.
Zhang W, Huang B, Yang J, Xue P, Liu X. Fractured coracoid process with acromioclavicular joint dislocation: a case report. Medicine. 2020;99(39):e22324.
Download references
Acknowledgements
Not applicable.
This work was supported by Funded by Science and Technology Projects in Guangzhou (2023A03J1015, 2024A03J0971, 202201020087, 2024A04J4173),the Fundamental Research Funds for the Central Universities (21623119, 21623319), Science and Technology Innovation and Sports Culture Development Research Project of Guangdong Provincial Sports Bureau (GDSS2022M002), Project of China University Sports Association (202203007), Medical Scientific Research Foundation of Guangdong Province (A2023143), the Clinical Frontier Technology Program of the First Affiliated Hospital of Jinan University, China (No. JNU1AF-CFTP-2022-a01204), Project of Clinical Medical Research in the First Affiliated Hospital of Jinan University (2018009), Medical Joint Fund of Jinan University (YXJC2022005), the Research Fund Program of Guangdong Provincial Key Laboratory of Speed Capability Research (2023B1212010009).
Author information
Weizhao Xie and Dahai Hu contributed equally to this work.
Authors and Affiliations
Department of Sports Medicine, The First Affiliated Hospital, Guangdong Provincial Key Laboratory of Speed Capability, The Guangzhou Key Laboratory of Precision Orthopedics and Regenerative Medicine, Jinan University, Guangzhou, 510630, PR China
Weizhao Xie, Dahai Hu, Huige Hou & Xiaofei Zheng
You can also search for this author in PubMed Google Scholar
Contributions
WZX and DHH: data acquisition, literature search, manuscript preparation. WZX and DHH: data acquisition, literature search. HGH: medical management. WZX and DHH: pathological interpretation, manuscript preparation and editing. XFZ and HGH: revised and reviewed the manuscript for the final publication. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Dahai Hu , Huige Hou or Xiaofei Zheng .
Ethics declarations
Ethics approval and consent to participate.
This study was performed in line with the principles of the Declaration of Helsinki. The patient agreed to participate in this study. Informed consent was obtained from the patient prior to the study. This study was approved by the Ethics Committee of the First Affiliated Hospital of Jinan University.
Consent for publication
Written informed consent has been obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Xie, W., Hu, D., Hou, H. et al. Arthroscopic reduction and hollow screw internal fixation for Eyres Type IIIA scapular coracoid fracture: a case report. BMC Musculoskelet Disord 25 , 645 (2024). https://doi.org/10.1186/s12891-024-07767-6
Download citation
Received : 18 March 2024
Accepted : 08 August 2024
Published : 15 August 2024
DOI : https://doi.org/10.1186/s12891-024-07767-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Scapular coracoid fracture
- Internal fixation
- Arthroscopy
- Hollow screw
BMC Musculoskeletal Disorders
ISSN: 1471-2474
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Get new issue alerts Get alerts
- Submit a Manuscript
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Rehabilitation of a Painful Shoulder – A Perspective Biomechanical Approach
Raj, V. Vijay Samuel; Ukil, Kundan Das 1 ; Shetty, Aparna 2
Department of Sports Sciences, JSS College of Physiotherapy, Mysore, Karnataka, India
1 Department of Musculoskeletal and Sports Physiotherapy, Brainware School of Medical and Allied Health Sciences, Brainware University, Barasat, West Bengal, India
2 Department of Musculoskeletal and Sports Physiotherapy, JSS College of Physiotherapy, Mysore, Karnataka, India
Address for correspondence: Dr. V. Vijay Raj, Department of Sport Science, JSS College of Physiotherapy, Mg Road, Mysore - 570 004, Karnataka, India. E-mail: [email protected]
Received March 30, 2022
Received in revised form November 16, 2022
Accepted December 16, 2022
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
The deltoid muscle is often forgotten when it comes to the evaluation and planning of treatment in shoulder conditions. Shoulder dysfunction, rotator cuff tendinopathy, and frozen shoulder are the conditions that affect functioning in major cases. The study involved an exploration of possible causes of dysfunction, especially pain and overhead activities. The patient presented with chronic pain and decreased shoulder function. A suitable shoulder rehabilitation program was designed keeping the deltoid muscle denervation into consideration. The shoulder pain, range of motion, strength, and function were evaluated at the baseline and the end of 6 weeks. The results were correlated and explored to identify the involvement of the deltoid muscle. The study showed a positive test of deltoid muscle involvement, which was identified through the strength-duration curve. There was a clinically significant improvement observed in the patients' function. Hence, the study hypothesized that along with scapular stabilization, it is important to consider deltoid equally during the assessment and treatment plan in shoulder rehabilitation program.
INTRODUCTION
The shoulder complex is an intricately designed combination of the glenohumeral joint, sternoclavicular joint, acromioclavicular joint, and scapulothoracic joint formed by the clavicle, scapula, and humerus. Shoulder articular structures are intended primarily for mobility, allowing for a wide range of motion (ROM).[ 1 ] The freedom of movement at the shoulder complex requires both mobility and stability which rely on both static and dynamic stabilization.[ 2 ] Dynamic stabilization results from a unique functional balance between mobility and stability through forces by the muscles that rely on dynamic muscular control rather than passive forces. The shoulder complex, muscles provide a stable base for the upper limb movements, it is important that the stability of scapula is essential to carry out an efficient function. When there is a loss of stabilization factors due to various reasons, the shoulder complex is susceptible to instability and dysfunction.
The common nerves that are involved in the shoulder are the axillary, long thoracic, and suprascapular and musculoskeletal nerves. The axillary nerve (AN) supplies the deltoid muscle, musculoskeletal nerve supplies the biceps, and may be entrapped or diseased. AN injury may present with axillary neuropathies caused due to various traumatic and compression injuries, also weakness of deltoid may be causative due to pathologies including subdeltoid bursa, acromion, and lateral clavicle.[ 3 ] Men are prone to AN injury than women at the ratio of 3:1.[ 4 ] Among the shoulder injuries, 9%–65% is AN injury.
The deltoid weakness can contribute to active loss of shoulder abduction, flexion, and extension and may be also caused due to AN injury, and caused due to anterior inferior dislocation, fracture, and fall on outstretched arm. The free portion of AN can be elongated due to displacement of the head of the humerus and may result in the avulsion of AN.[ 5 ] A special consideration needs to be made on the evaluation and functional diagnosis of shoulder dysfunction. The stability and mobility factors and ratio of contribution during upper limb function have to be considered in the assessment and plan of care during shoulder rehabilitation. This manuscript presents the interesting case study with an aim to present the importance of biomechanical evaluation and treatment, emphasizing on the evaluation of the auxiliary nerve involvement.
CASE REPORT
The client was a 63-year-old adult male, who visited the physiotherapy department at a tertiary hospital with complaints of pain at the left shoulder and arm for the past 6 months. He reported 1 st episode of injury during performing sumo squat, which included squats with wider base and holding a kettlebell and also later during bicep curl of 5 kg and triceps curls of 5 kg. The pain aggravated on any of the weightlifting activities since then. He consulted the orthopedic surgeon and diagnosed with partial width tear of the supraspinatus, subacromial impingement of rotator cuff, subdeltoid bursitis, and bicipital tenosynovitis. He was prescribed analgesics, advised to rest for 10 days, and referred to physiotherapy. He was treated with joint mobilization emphasizing on inferior glides with stretching of trapezius, and strengthening, and went for acupuncture. There was a 60%–70% reduction in the Visual Analog Scale (VAS) after treatment, but with a reoccurrence of pain intermittently. Three months later, during his trip abroad, with no specific reason mentioned, the pain increased in the night, for which he took therapy for 2 days from a joint specialist, where he found symptomatic relieve. The second episode occurred after lifting a suitcase of 23 kg to place it at the high head plank, which gave sudden sharp shooting pain to the patient at the left shoulder, which disabled him from lifting any weight. He had his visit to the department after this incident.
The sumo squat included standing with wide feet at shoulder width apart holding a kettlebell with both arms in front. Normally, the squat would include dropping the hips back and down, as sitting in a chair, allowing the kettlebell to swing down in between the legs, one would use the knee and hip to swing the kettlebell up and not the shoulders or one's arms. Probably, altered biomechanics would have been followed by the patient using more of his arms and shoulders, leading to a hypothesis of the shoulder muscles involvement leading to strain or AN injury.
The subjective and objective data were collected and presented with clinical reasoning form using a visual analysis. The data were plotted using Microsoft Office Excel software at baseline, before intervention and after 4 weeks of planned exercise program, and 6 weeks for discharge. Written consent was obtained from the client and the physiotherapy plan was clearly explained in his own language.
Patient evaluation and treatment planning
The client was interviewed with detailed subjective evaluation before starting of the exercise program. The client could not perform activities of daily living involving reach to the back by the left hand, and he complained about the difficulty in overhead activities and pain limiting the function. The initial evaluation of pain assessment, postural deformity, girth, muscle strength, and ROM evaluation was recorded and documented. The sensation over the neck and upper limb was intact. In the outcome measure, the Shoulder Pain and Disability Index (SPADI) of 71.53% was reported. In pain level, initial intensity of the pain was VAS 8 out of 10, the characteristics were chronic dull aching and most of the time patient experienced pain in the morning time, aggravating factor was due to stretch, weight lifting, sleeping on the affected side, and relieving factors were rest and heat application.
On observation, muscle atrophy in infraspinatus, supraspinatus, deltoid, triceps, and biceps was noticed. The posture assessment on the postural grid depicted a protracted shoulder, elevated shoulder on the left side, and winging of the scapula. The shoulder ROM during flexion, extension, abduction, and external and internal rotation was limited [ Table 1 ], with a firm end feel, pain onset (P1) followed by resistance limit (R2). The muscle strength and girth measurements were also taken shown in the table and abnormal glenohumeral rhythm (scapular dyskinesia) was noticed. Special tests for the shoulder were done to identify the underlying pathology. Empty can test, superior and inferior scratch test, Neer impingement test, speed's test, and Yergason's test, all were considered positive, these were in turn the interpretation of patient and the impingement of supraspinatus and biceps were possibly confirmed, with joint capsule involvement. Correlating the finding of special tests and kinetics, possibly a compression at the quadrilateral space may be considered for further evaluation.[ 6 , 7 ] The presenting symptoms of the patient were night pain and weakness in the shoulder–glenohumeral abduction and external rotator, without numbness to the lateral shoulder area. Thus, leading to a hypothesis of the involvement of the middle deltoid and the AN, this may be caused due to primary shoulder impingement syndrome, caused due to faulty shoulder position.

Baseline tests and follow-up were conducted before the start of the exercise program. The tests are joint ROM, muscle strength, VAS, and strength-duration curve (SDC). The follow-up tests were conducted every week and 4 weeks after to check the improvement, and with obtained results, the exercise program was changed for consecutive sessions based on the assessment using the same test methods and finally at 6 weeks for discharge. A minimal clinically important difference (MCID) for ROM of ≥9° was considered. The shoulder function was assessed using SPADI, considering a MCID of 8–13 points.[ 8 ] The muscle girth was assessed using a standard flexible inch tape and measured in centimeter (cm).[ 9 ]
Rehabilitation program
The exercise program was composed of 6 weeks [Annexure 1], planned in five phases, which included the baseline tests and every week follow-up tests. To reduce the pain at left shoulder ultrasound therapy (UST), faradic muscle stimulation for supraspinatus, biceps, and anterior and middle deltoid 30 contractions [Annexure 1].
Visual Analog Scale
The level of subjective pain was measured using VAS when the shoulder joint was moved, with 10 as the highest level of pain. Pain at the shoulder joint before the exercise was 8, and the pain level reduced to 6 in 4 days and to 4 in 2 weeks at the maximum joint range.
Muscle girth, strength, and function
The girth measurement showed an improvement with a difference of 4.5 cm in the left arm girth. Similarly, at left forearm showed a difference of 1 cm. The significant improvement in muscle strength was noted in shoulder flexors (anterior fibers of deltoid, long head of biceps, and supraspinatus) with a difference of 10 lbs and similarly in biceps muscle with a difference of 19 lbs. However, the strength of shoulder extensors, abductors, internal rotators, and external rotators showed improvement, it was negligible as the difference was <6 lbs. The results of the strength measured by handheld dynamometer are depicted in Table 1 . Improvement in function was achieved; SPADI outcome was noted at 71.53% in the baseline and 86.55% in the posttest, with a difference of improvement of 15%, with difference score of 40 points, which was far above the MCID.
The measurements were taken in the following order: shoulder flexion, abduction, internal rotation, and external rotation. Joint motion observed an increased range in all movements with an evident increase in shoulder internal and external rotation. The ROM improvement in flexion and abduction can be ignored considering the MCID and errors. The results of the ROM of shoulder joint are shown in Table 1 .
Strength duration curve
The SDC responses for the biceps muscle (AN) showed abnormal chronaxie (2.2 ms), with the curve representing a compression, showing a minimal kink [ Figure 1 ]. The posttest responses recorded a normal chronaxie (0.38 ms) representing a normal curve. An evident improvement in the strength response was observed depicting that the nerve function may be restored.

The study was conducted in five phases. In the first phase, the treatment plan was made after evaluating the patient. In the second phase, preliminary tests were conducted. In the third phase, the exercise protocol was programmed. In the fourth phase, reevaluation was done, and in the fifth phase redesigning of exercise program over 6 weeks, each of the sessions lasted for 1 h.
Historically, the assessment of musculoskeletal problems in the shoulder joint has been based on the premise that it is possible to isolate the individual structure at fault. In the differential diagnosis of shoulder dysfunction, it is essential to rule out the origin of pain, in this case, the evaluation findings hypothesized that it might be due to AN pathology involving the deltoid muscle. In this case, postexercise, there was a lag in the shoulder flexor strength, in contrary to the biceps brachii muscle showing an excellent improvement in strength, when compared with the unaffected side. This leads to the confirmation of the anterior deltoid muscle involvement. This study further concludes that in spite of strong improvement in the deltoid group of muscles, the strength was not achieved to match the unaffected side. Exercise programs of longer duration exceeding 6 weeks may be necessary to achieve actual strength with change in the resistance training programs.[ 10 ] Patient reported that the sumo squat with kettlebell exercises caused the first episode, this supports with the possibilities of abnormal kinematics and kinetics[ 11 ] of the shoulder and scapula, leading to AN injury. This study emphasizes, the biomechanical evaluation including movement analysis may aid in functional decision-making and planning an appropriate physiotherapy intervention. This may be evidently followed in sports injury management. Many times, the deltoid muscle is ignored during the shoulder evaluation. However, the shoulder stabilizers involving the scapula stability play an essential function during static and dynamic activities, it is necessary to consider the deltoid along with the scapular muscles during the assessment of shoulder dysfunction and plan an appropriate plan of care. In this study, the patients, glenohumeral accessory movements (glides) were optimal, but pain limiting the movement, and due to the reason passive mobilization techniques were not delivered. There was a significant improvement observed in the patients' function, both subjectively and objectively. The parameters such as SPADI, muscle strength, and muscle girth measurements have shown significant clinical improvement in recovery. The patient was enthusiastic and cooperative throughout the treatment session, and there were no difficulties observed by the patient to follow the exercise protocol.
The study showed a positive test of deltoid muscle involvement, which was identified through the strength-duration curve. There was a clinically significant improvement observed in the patients' function. Hence, the study hypothesized that along with scapular stabilization, it is important to consider deltoid equally during assessment and treatment plan in shoulder rehabilitation program.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Shoulder Rehabilitation Protocol:
- Passive and active stretching of pectorals and biceps muscle
- Faradic Stimulation – Deltoid inhibition techniques – Intermittent 100 Hz, 1 ms pulse duration, rest time 5–10 s. 20–30 contractions
- UST (1 Mhz, pulsed 1:1, 0.8 W/cm 2 , 4–6 min) calculated based on the standard operating procedure of the department of physiotherapy, and treatment calculation chart. (Watson, T. (2002). “Ultrasound Dose Calculations“ In Touch 101;14-17)
- Strengthening exercises comprised.
- Muscle setting exercises (isometrics)
- Resistance exercise with resistance band and dumbbells for shoulder flexors and abductors (10 rep × 3 sets) each in supine lying
- Horizontal abduction was planned to improve eccentric contraction of retractors and active stretching of pectorals (10reps × 3 sets)
- Retractor strengthening using resistance band (10 reps × 3 sets)
- Bicep curl-ups using 60%–80% 1 RM graded increment using dumbbells (10 reps × 3 sets)
- Triceps strengthening using resistance band (10 reps × 3 sets)
- Home exercise program with plans to improve the retractor strength and shoulder mobility and strength was planned for 5 days/week
- Safe lifting techniques and ergonomic measures were advised.
Axillary nerve; deltoid; physiotherapy; rehabilitation; shoulder dysfunction; shoulder pain
- + Favorites
- View in Gallery
The relationship between MRI-detected hip abnormalities and hip pain in hip osteoarthritis: a systematic review
- Systematic Review
- Open access
- Published: 13 August 2024
Cite this article
You have full access to this open access article

- Haonan Fang 1 ,
- Xiaoyue Zhang 1 ,
- Junjie Wang 1 ,
- Xing Xing 1 ,
- Ziyuan Shen 1 , 2 &
- Guoqi Cai 1 , 2
154 Accesses
1 Altmetric
Explore all metrics
Magnetic resonance imaging (MRI) is increasingly used in the classification and evaluation of osteoarthritis (OA). Many studies have focused on knee OA, investigating the association between MRI-detected knee structural abnormalities and knee pain. Hip OA differs from knee OA in many aspects, but little is known about the role of hip structural abnormalities in hip pain. This study aimed to systematically evaluate the association of hip abnormalities on MRI, such as cartilage defects, bone marrow lesions (BMLs), osteophytes, paralabral cysts, effusion-synovitis, and subchondral cysts, with hip pain. We searched electronic databases from inception to February 2024, to identify publications that reported data on the association between MRI features in the hip joint and hip pain. The quality of the included studies was scored using the Newcastle-Ottawa Scale (NOS). The levels of evidence were evaluated according to the Cochrane Back Review Group Method Guidelines and classified into five levels: strong, moderate, limited, conflicting, and no evidence. A total of nine studies were included, comprising five cohort studies, three cross-sectional studies, and one case-control study. Moderate level of evidence suggested a positive association of the presence and change of BMLs with the severity and progress of hip pain, and evidence for the associations between other MRI features and hip pain were limited or even conflicting. Only a few studies with small to modest sample sizes evaluated the association between hip structural changes on MRI and hip pain. BMLs may contribute to the severity and progression of hip pain. Further studies are warranted to uncover the role of hip MRI abnormalities in hip pain. The protocol for the systematic review was registered with PROSPERO ( https://www.crd.york.ac.uk/PROSPERO/ , CRD42023401233).
Similar content being viewed by others

Osteoarthritis of the hip: is radiography still needed?

Quantification of hip effusion-synovitis and its cross-sectional and longitudinal associations with hip pain, MRI findings and early radiographic hip OA
Bone marrow lesions in osteoarthritis: biomarker or treatment target? A narrative review
Explore related subjects.
- Medical Imaging
Avoid common mistakes on your manuscript.
Intruduction
Osteoarthritis (OA) is a common musculoskeletal disease of the entire joint, characterized by pain and disability [ 1 ]. The hip joint is a frequently affected site of OA [ 2 ], affecting more than 240 million people in the world [ 3 ]. The pathophysiology of OA involves multiple tissues, including cartilage, bone, ligaments, synovium, and muscles [ 2 , 4 ]. Understanding the involvement of these tissues in joint symptoms is crucial for developing effective treatment strategies. Although conventional x-rays are frequently used for the diagnosis and classification of OA, soft tissues cannot be adequately evaluated using this technique. Moreover, the available evidence does not show a consistent association between radiographic features and OA pain [ 5 , 6 ]. More advanced imaging techniques, especially magnetic resonance imaging (MRI), offer much higher sensitivity in detecting early signs of joint damage, making it an invaluable tool for evaluating OA and its associated pain [ 7 , 8 ].
In contrast to the extensive body of research examining factors associated with knee pain, there has been much fewer studies investigating the source of hip pain [ 9 ]. The xcharacteristics of hip OA differ significantly from knee OA in many aspects including epidemiology, prognosis, pathophysiology, anatomical and biomechanical factors, clinical presentation, and pain management [ 10 ]. Thus, the etiology and contributing factors for hip pain can differ from those of knee pain. It has been shown that knee pain is associated with several MRI features such as bone marrow lesions (BMLs) [ 11 ], effusion/synovitis [ 12 , 13 ], meniscus tear, infrapatellar fat pad [ 14 ], osteophytes [ 15 ] and cartilage defects [ 16 ]. Clinical studies have gone further to explore the use of BMLs and effusion-synovitis as treatment targets for knee OA [ 17 , 18 , 19 , 20 ]. However, few studies have evaluated the role of MRI features in the hip in the assessment, prognosis, and treatment of hip OA. Therefore, this study aimed to systematically review studies evaluating the association between MRI abnormalities and hip pain.
Materials and methods
Protocol registration.
The protocol for the systematic review was registered with PROSPERO ( https://www.crd.york.ac.uk/PROSPERO/ , CRD42023401233). This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [ 21 ]. The report of this study followed the Cochrane Handbook for Systematic Reviews of Interventions [ 22 ]. This study was a systematic review and ethics committee review was not applicable.
Data source and search strategy
We searched Medline (via Ovid), Web of science, Embase (via Ovid), and Cumulative Index to Nursing & Allied Health Literature (CINAHL) from inception to June 2024, for relevant studies evaluating the association of MRI abnormalities in the hip with hip pain. The following search terms were used: ‘hip’, ‘hip joint’, ‘pain’, ‘MRI’, ‘osteoarthritis’, detailed search strategies are provided in the Supplementary Methods. We also checked the citation lists of the included studies and relevant systematic reviews and gray literature (e.g. conference abstract) for additional studies.
Study selection
Two authors (HF and XZ) conducted an independent review of the titles and abstracts of all identified studies, followed by retrieving the full texts of relevant studies for further screening. The full-text reviews were performed in accordance with the selection criteria outlined in the registered protocol. Specifically, observational studies evaluating the association between MRI abnormalities (e.g. BMLs or cartilage defect) and pain in the hip joint were included. Animal studies or studies without data on MRI features and/or hip pain were excluded. There was no restriction on language.
Data extraction
Two authors (HF and XZ) independently extracted data from each included study. The extracted data included: (1) study characteristics (the first author, year of publication, place (country/territory), study design, and sample size); (2) characteristics of the study population (e.g. age, sex, OA patients or community-dwelling participants); (3) MRI features (e.g. subchondral cysts, paralabral cysts, cartilage defects, BMLs, osteophytes, and effusion/synovitis) (Table 1 ); (4) assessment of hip pain, (5) main findings for the association between MRI features and hip pain; and (6) adjusted covariates.

Assessment of study quality and credibility of evidence
Two authors (HF and XZ) independently assessed the methodological quality of the included studies using the Newcastle-Ottawa Scale (NOS) for cohort studies [ 23 ] and case-control studies [ 24 ], and an extension for cross-sectional studies [ 25 ]. Differences in scoring were resolved by discussion or by consulting the third author (GC). The possible scores of study quality ranged from 0 to 9 for cohort studies, 0–8 for cross-sectional and case-control studies, with higher scores indicating higher quality. A score of ≥ 7 was considered high study quality for cohort studies [ 26 ], cross-sectional studies [ 27 ] and case-control studies [ 28 ].
The same two authors independently evaluated the credibility of evidence for the association between each MRI feature and hip pain on the basis of the guidelines of the Cochrane Collaboration Back Review Group [ 29 ]. The credibility of evidence was categorized into five levels based on the following criteria: (1) Strong: multiple high-quality cohort studies show generally consistent findings, (2) Moderate: One high-quality cohort study and at least two high-quality cross-sectional studies or only at least three high-quality cross-sectional studies show generally consistent findings, (3) Limited: a single cohort study, or up to two cross-sectional studies show less consistent findings, (4) Conflicting: no consistent findings were reported, (5) No evidence: no studies were published.
Literature search
The flowchart of the study selection process is shown in Fig. 1 . We identified a total of 1878 potentially relevant records from electronic search. After screening the titles and abstracts, 1864 were excluded. From the remaining 14 records, we further excluded 5 irrelevant studies, leaving 9 studies in this systematic review. Among the studies included, 5 were cohort studies [ 30 , 31 , 32 , 33 , 34 ], 3 were cross-sectional studies [ 35 , 36 , 37 ], and 1 was a case-control study [ 38 ].
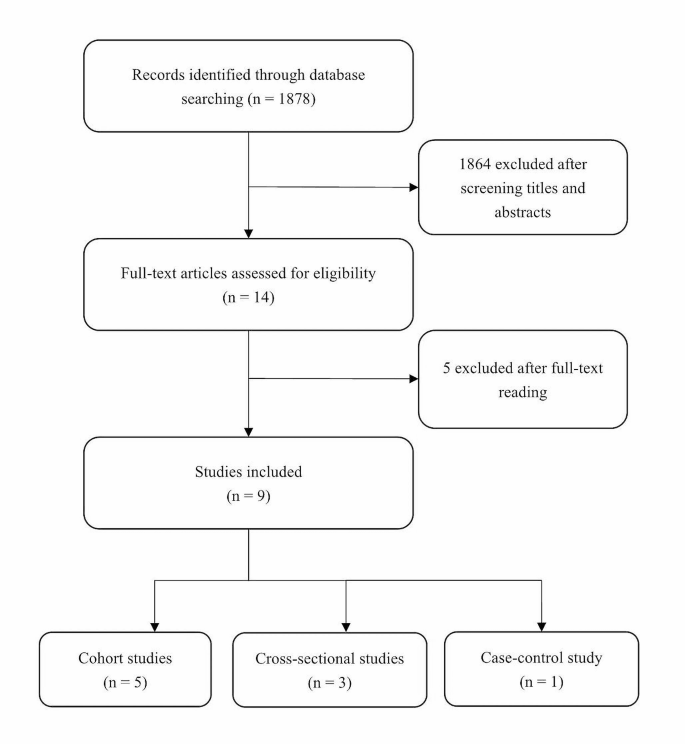
Flowchart of study selection
Characteristics of included studies
Table 2 shows the characteristics of included studies. Overall, the sample size of the studies were small to modest ( n = 19 to 237), and the follow-up time of the 5 cohort studies ranged from 1 to 2.3 years. Among the 9 included studies, 4 examined multiple MRI features [ 32 , 35 , 37 , 38 ] and 5 examined a single MRI feature [ 30 , 31 , 33 , 34 , 36 ]. Three studies were conducted in the same population [ 30 , 33 , 34 ]. Four studies used a 1.5T MRI [ 30 , 33 , 34 , 36 ], four used a 3T scanners [ 31 , 32 , 35 , 38 ], and the remaining one did not report the strength of MRI used [ 37 ]. Most of the studies used sagittal imaging [ 30 , 32 , 33 , 34 , 37 , 38 ], with two studies using both sagittal, coronal and oblique axial imaging [ 32 , 38 ], only one study used coronal and sagittal imaging [ 35 ], and one study used coronal imaging alone [ 36 ]. The patients investigated in the included studies were essentially middle-aged and older adults (mean age 46.5 to 66 years, 27.6-57.9% males), except for one study that examined high-impact athletes in their 20s and 30s [ 38 ].
Assessment of study quality
Five of the 9 studies (55.6%) were scored above the high-quality threshold (i.e. ≥7) according to the NOS assessment. For cross-sectional studies, only 1 of the 3 studies was scored high-quality, with the main issues being small sample size, sample representativeness, and the lack of comparison between respondents and non-respondents. Meanwhile, 4 of the 5 cohort studies were above the high-quality threshold, and only 1 study had issues with the representation and selection of exposed and non-exposed groups (Supplementary Tables 1–3).
Association between MRI features and hip pain
Subchondral cysts.
One cross-sectional study [ 35 ], one case-control study [ 38 ] and one cohort study [ 32 ] evaluated the association between subchondral cysts and hip pain (Table 3 ). The credibility of the evidence was limited. The cross-sectional study showed a positive correlation between total subchondral cyst score (grade 0–2) and more severe hip pain score, assessed by the Harris Hip Score and Hip Disability and Osteoarthritis Outcome Score (HOOS) pain subscale (rank correlation coefficient = 0.37, P = 0.001) [ 35 ]. The case-control study did not observe a significant difference in subchondral cysts (grade 0–2) between symptomatic and control hips in athletes (8% vs. 7%, odds ratio (OR) = 1.29, 95% confidence interval (CI) 0.51 to 3.23) [ 38 ]. The cohort study showed a boardline significant association between baseline subchondral cyst score (grade 0–2) and change in hip pain (rank correlation coefficient = 0.30, p = 0.051) [ 32 ]. Moreover, the cohort study found a significant correlation between progression of subchondral cysts and change in HOOS symptoms other than pain (i.e. functional disability and stiffness) (rank correlation coefficient = 0.30, p = 0.03) but not hip pain score over 1.5 years (rank correlation coefficient = 0.18, p = 0.19) [ 32 ].
Paralabral cyst
One cross-sectional study [ 37 ] and one cohort study [ 32 ] evaluated the association between paralabral cyst and hip pain (Table 3 ). The credibility of the evidence was limited. The cross-sectional study found that paralabral cyst scores, based on the Hip Osteoarthritis MRI Scoring System (HOAMS), were similar in painless and painful hips (mean paralabral cyst score: 0.81 vs. 0.91, p = 0.39) [ 37 ]. Consistently, the cohort study found that neither baseline nor progression of paralabral cysts was associated with change in HOOS pain or other subscales, except that progression of paralabral cysts was associated with HOOS activity of daily living subscale (rank correlation coefficient = 0.30, p = 0.03) [ 32 ].
Effusion-synovitis
One cross-sectional study [ 37 ], one case-control study [ 38 ] and one cohort study [ 34 ] showed inconsistent findings for the association between hip effusion-synovitis and hip pain (Table 3 ). The credibility of the evidence was conflicting. The cohort study observed a significant positive correlation between presence of hip effusion-synovitis at two/three sites and presence of hip pain (PR (95% CI): 1.42 (1.05, 1.93)), although there was no significant correlation between change in effusion-synovitis size and change in hip pain [ 34 ]. By contrast, the case-control study showed an inverse correlation between effusion-synovitis and the presence of hip symptoms (OR (95% CI) 0.46 (0.26, 0.81)), before and after adjusting for age, sex, and BMI [ 38 ]. The remaining cross-sectional study reported no significant associations between joint effusion/synovitis and hip pain [ 37 ].
Cartilage defects
One cohort study [ 33 ], one case-control study [ 38 ] and two cross-sectional studies [ 35 , 37 ] examined the association between cartilage defects and hip pain (Table 3 ). The credibility of the evidence was limited. The cohort study reported higher levels of Western Ontario and McMaster Universities Arthritis Index (WOMAC) hip pain in individuals with any type of hip cartilage defects (PR (95% CI): 1.20 (1.02, 1.35)) and secondary cartilage defects (PR (95% CI): 1.40 (1.09, 1.80)) [ 33 ]. One cross-sectional study reported a significant linear correlation between cartilage defects score and Visual Analogue Scale (VAS) hip pain ( r = 0.46, P < 0.001), although cartilage defects score was not statistically significantly different between individuals with and those without hip pain (mean cartilage defects score: 1.23 vs. 0.75, p = 0.18) [ 37 ], another cross-sectional study found a significant correlation between acetabular cartilage score and HOOS pain ( r = 0.25, p = 0.026), but there’s no correlation between femoral cartilage score and HOOS pain (r s =0.17, p = 0.146) [ 35 ].
Osteophytes
One cross-sectional study [ 37 ] examined the relationship between MRI-detected osteophytes and hip pain (Table 3 ), showing a positive correlation between osteophyte score and VAS pain ( r = 0.5811, p < 0.0001), and there was a higher osteophyte score in the inferomedial compartment in individuals with hip pain than those without (3.0 vs. 2.0, p = 0.03) [ 37 ]. The credibility of evidence was limited.
Three cohort studies [ 30 , 31 , 32 ], three cross-sectional studies [ 35 , 36 , 37 ], and one case-control study [ 38 ] evaluated the association between BMLs and hip pain (Table 3 ). The credibility of evidence was moderate. All three cohort studies consistently reported a significant association between BMLs and hip pain, with one showing that change in BML size was significantly associated with change in hip pain (regression coefficient [β] (95% CI): 0.85 (0.00, 1.71)), and the severity of hip pain was associated with a per square centimeter increase in the size of acetabular BML (regression coefficient [β] (95% CI): 4.18 (1.54, 6.88)) [ 30 ]. The second cohort study found that Modified Harris Hip Score (MHHS) pain score was significantly lower in individuals with BMLs than those without, regardless of the size of BMLs ( p < 0.05) [ 31 ], and the third cohort study indicated that baseline BML size was significantly associated with worsening of HOOS pain subscale (regression coefficient [β] (95% CI): 0.690 (0.464, 0.913)) [ 32 ]. All three cross-sectional studies reported positive correlations between BML scores and hip pain ( r = 0.29 to 0.51, p < 0.05) [ 35 , 36 , 37 ], and the remaining case-control study did not observe a significant differences in BML scores between symptomatic and control hips [ 38 ].
This systematic review screened and evaluated studies that described the association between MRI-detected hip abnormalities and hip pain, and several MRI features were identified, such as osteophytes, subchondral cysts, paralabral cysts, effusion-synovitis, BMLs and cartilage defects. Overall, the number, sample size, and quality of included studies were inferior to studies focusing on the knee, and current evidence suggests that BMLs, cartilage defects, and osteophytes may be associated with the presence and severity of hip pain, while subchondral and paralabral cysts may not. Moreover, the association between effusion-synovitis and hip pain was conflicting. Considering the paucity of studies examining their association, a robust conclusion cannot be reached [ 39 ]. Thus, more studies are required to validate whether these MRI features contribute to the presence and severity of hip pain.
The credibility of evidence for the association between each of the hip MRI features and hip pain was limited or even conflicting, except that there was a moderate level of evidence for the association between BMLs and hip pain. This can be attributed to various reasons. Firstly, the limited number of included studies may have restricted the breadth and depth of the analysis, potentially leading to less robust conclusions. Secondly, some of the included studies might have exhibited lower overall quality of evidence due to factors such as small sample sizes and inadequate representativeness, impacting the reliability and validity of the findings. Moreover, our research methodology, which involved aggregating study results and applying uniform criteria, while simple, may have hindered the effective synthesis and interpretation of the data, potentially resulting in less accurate or comprehensive outcomes.
We found moderate evidence of a positive association between BMLs and hip pain. These findings are similar to other studies showing a significant association between BMLs and knee pain [ 11 , 40 ], suggesting that BMLs could be a potential cause or indicator of both knee and hip OA. This could contribute to the management of hip OA, as effectively managing the progression of BMLs may reduce knee pain in knee OA with BMLs [ 18 ]. The additional MRI features in this study, despite showing limited or conflicting evidence, play a role in semi-quantitative evaluation of hip OA [ 41 ]. These features, awaiting further study, hold promise for distinguishing hip OA subtypes and informing its diagnosis and treatment.
The strength of this study is that we systematically screened studies that evaluated the association between hip MRI abnormalities and hip pain and employed a pre-specified assessment system to qualitatively evaluate the credibility of evidence. There are several limitations in this study. First, we categorized the results of the included studies as either negative or positive based solely on statistical significance, without considering the influence of sample size on the outcomes, and this may have overlooked false negative findings. However, the limited number of studies disabled us from conducting a meta-analysis to pool these results. Second, we scored the methodological quality of the included studies with different designs. The subjective awareness of the evaluator can have an impact on the results of the assessment, leading to biases, although the scores were rated by different authors to reach a consensus.
In conclusion, only a few studies with small to modest sample sizes evaluated the association between hip structural changes on MRI and hip pain. BMLs may contribute to the severity and progression of hip pain. Further studies are warranted to uncover the role of hip MRI abnormalities in hip pain.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Hutton CW (1987) Generalised osteoarthritis: an evolutionary problem? Lancet. (London England) 1(8548):1463–1465. https://doi.org/10.1016/s0140-6736(87)92209-4
Article CAS Google Scholar
Lespasio MJ, Sultan AA, Piuzzi NS, Khlopas A, Husni ME, Muschler GF, Mont MA (2018) Hip osteoarthritis: a primer. Permanente J 22:17–084. https://doi.org/10.7812/tpp/17-084
Article Google Scholar
Katz JN, Arant KR, Loeser RF (2021) Diagnosis and treatment of hip and knee osteoarthritis: a review. JAMA 325(6):568–578. https://doi.org/10.1001/jama.2020.22171
Article CAS PubMed PubMed Central Google Scholar
Loeser RF, Goldring SR, Scanzello CR, Goldring MB (2012) Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum 64(6):1697–1707. https://doi.org/10.1002/art.34453
Article PubMed PubMed Central Google Scholar
Neogi T, Felson D, Niu J, Nevitt M, Lewis CE, Aliabadi P, Sack B, Torner J, Bradley L, Zhang Y (2009) Association between radiographic features of knee osteoarthritis and pain: results from two cohort studies. BMJ (Clinical Res ed) 339:b2844. https://doi.org/10.1136/bmj.b2844
Kim C, Nevitt MC, Niu J, Clancy MM, Lane NE, Link TM, Vlad S, Tolstykh I, Jungmann PM, Felson DT, Guermazi A (2015) Association of hip pain with radiographic evidence of hip osteoarthritis: diagnostic test study. BMJ (Clinical Res ed) 351:h5983. https://doi.org/10.1136/bmj.h5983
Guermazi A, Roemer FW, Haugen IK, Crema MD, Hayashi D (2013) MRI-based semiquantitative scoring of joint pathology in osteoarthritis. Nat Rev Rheumatol 9(4):236–251. https://doi.org/10.1038/nrrheum.2012.223
Article PubMed Google Scholar
Roemer FW, Guermazi A, Demehri S, Wirth W, Kijowski R (2022) Imaging in Osteoarthritis. Osteoarthr Cartil 30(7):913–934. https://doi.org/10.1016/j.joca.2021.04.018
Sandhar S, Smith TO, Toor K, Howe F, Sofat N (2020) Risk factors for pain and functional impairment in people with knee and hip osteoarthritis: a systematic review and meta-analysis. BMJ open 10(8):e038720. https://doi.org/10.1136/bmjopen-2020-038720
van der Hall M, Hinman RS, Peat G, de Zwart A, Quicke JG, Runhaar J, van der Knoop J, de Rooij M, Meulenbelt I, Vliet Vlieland T, Lems WF, Holden MA, Foster NE, Bennell KL (2022) How does hip osteoarthritis differ from knee osteoarthritis? Osteoarthr Cartil 30(1):32–41. https://doi.org/10.1016/j.joca.2021.09.010
Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, Kazis L, Gale DR (2001) The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med 134(7):541–549. https://doi.org/10.7326/0003-4819-134-7-200104030-00007
Article CAS PubMed Google Scholar
Hill CL, Hunter DJ, Niu J, Clancy M, Guermazi A, Genant H, Gale D, Grainger A, Conaghan P, Felson DT (2007) Synovitis detected on magnetic resonance imaging and its relation to pain and cartilage loss in knee osteoarthritis. Ann Rheum Dis 66(12):1599–1603. https://doi.org/10.1136/ard.2006.067470
Wang X, Jin X, Han W, Cao Y, Halliday A, Blizzard L, Pan F, Antony B, Cicuttini F, Jones G, Ding C (2016) Cross-sectional and longitudinal associations between knee joint effusion synovitis and knee Pain in older adults. J Rhuematol 43(1):121–130. https://doi.org/10.3899/jrheum.150355
Pan F, Han W, Wang X, Liu Z, Jin X, Antony B, Cicuttini F, Jones G, Ding C (2015) A longitudinal study of the association between infrapatellar fat pad maximal area and changes in knee symptoms and structure in older adults. Ann Rheum Dis 74(10):1818–1824. https://doi.org/10.1136/annrheumdis-2013-205108
Zhu Z, Laslett LL, Jin X, Han W, Antony B, Wang X, Lu M, Cicuttini F, Jones G, Ding C (2017) Association between MRI-detected osteophytes and changes in knee structures and pain in older adults: a cohort study. Osteoarthr Cartil 25(7):1084–1092. https://doi.org/10.1016/j.joca.2017.01.007
Everhart JS, Abouljoud MM, Flanigan DC (2019) Role of full-thickness cartilage defects in knee osteoarthritis (OA) incidence and progression: data from the OA Initiative. J Orthop Res 37(1):77–83. https://doi.org/10.1002/jor.24140
Eriksen EF (2015) Treatment of bone marrow lesions (bone marrow edema). BoneKEy Rep 4:755. https://doi.org/10.1038/bonekey.2015.124
Callaghan MJ, Parkes MJ, Hutchinson CE, Gait AD, Forsythe LM, Marjanovic EJ, Lunt M, Felson DT (2015) A randomised trial of a brace for patellofemoral osteoarthritis targeting knee pain and bone marrow lesions. Ann Rheum Dis 74(6):1164–1170. https://doi.org/10.1136/annrheumdis-2014-206376
Cai G, Aitken D, Laslett LL, Pelletier JP, Martel-Pelletier J, Hill C, March L, Wluka AE, Wang Y, Antony B, Blizzard L, Winzenberg T, Cicuttini F, Jones G (2020) Effect of Intravenous Zoledronic Acid on Tibiofemoral cartilage volume among patients with knee osteoarthritis with bone marrow lesions: a Randomized Clinical Trial. JAMA 323(15):1456–1466. https://doi.org/10.1001/jama.2020.2938
Wang Z, Jones G, Winzenberg T, Cai G, Laslett LL, Aitken D, Hopper I, Singh A, Jones R, Fripp J, Ding C, Antony B (2020) Effectiveness of Curcuma longa Extract for the treatment of symptoms and effusion-synovitis of knee osteoarthritis : a Randomized Trial. Ann Intern Med 173(11):861–869. https://doi.org/10.7326/m20-0990
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Higgins JPTTJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2023) Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). www.training.cochrane.org/handbook
Wells GA, Wells G, Shea B, Shea B, O’Connell D, Peterson J, Welch, Losos M, Tugwell P, Ga SW, Zello GA, Petersen JA (2014) The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. In
Burfield M, Sayers M, Buhmann R (2023) The association between running volume and knee osteoarthritis prevalence: a systematic review and meta-analysis. Phys Therapy Sport : Official J Association Chart Physiotherapists Sports Med 61:1–10. https://doi.org/10.1016/j.ptsp.2023.02.003
Moskalewicz A, Oremus M (2020) No clear choice between Newcastle-Ottawa Scale and Appraisal Tool for cross-sectional studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J Clin Epidemiol 120:94–103. https://doi.org/10.1016/j.jclinepi.2019.12.013
Mahdi SS, Allana R, Battineni G, Khalid T, Agha D, Khawaja M, Amenta F (2022) The promise of telemedicine in Pakistan: a systematic review. Health Sci Rep 5(1):e438. https://doi.org/10.1002/hsr2.438
Neal BS, Lack SD, Lankhorst NE, Raye A, Morrissey D, van Middelkoop M (2019) Risk factors for patellofemoral pain: a systematic review and meta-analysis. Br J Sports Med 53(5):270–281. https://doi.org/10.1136/bjsports-2017-098890
Su B, Qin W, Xue F, Wei X, Guan Q, Jiang W, Wang S, Xu M, Yu S (2018) The relation of passive smoking with cervical cancer: a systematic review and meta-analysis. Medicine 97(46):e13061. https://doi.org/10.1097/md.0000000000013061
van Tulder M, Furlan A, Bombardier C, Bouter L (2003) Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 28(12):1290–1299. https://doi.org/10.1097/01.Brs.0000065484.95996.Af
Ahedi H, Aitken D, Blizzard L, Cicuttini F, Jones G (2014) A population-based study of the association between hip bone marrow lesions, high cartilage signal, and hip and knee pain. Clin Rheumatol 33(3):369–376. https://doi.org/10.1007/s10067-013-2394-0
Koyama T, Fukushima K, Uchida K, Ohashi Y, Uchiyama K, Takahira N, Takaso M (2022) Is bone marrow oedema in patients with labral tear an indicator of hip pain? J Orthop Surg Res 17(1):420. https://doi.org/10.1186/s13018-022-03243-w
Schwaiger BJ, Gersing AS, Lee S, Nardo L, Samaan MA, Souza RB, Link TM, Majumdar S (2016) Longitudinal assessment of MRI in hip osteoarthritis using SHOMRI and correlation with clinical progression. Semin Arthritis Rheum 45(6):648–655. https://doi.org/10.1016/j.semarthrit.2016.04.001
Ahedi HG, Aitken DA, Blizzard LC, Ding CH, Cicuttini FM, Jones G (2016) Correlates of hip cartilage defects: a cross-sectional study in older adults. J Rhuematol 43(7):1406–1412. https://doi.org/10.3899/jrheum.151001
Ahedi H, Aitken D, Blizzard L, Cicuttini F, Jones G (2020) Quantification of hip effusion-synovitis and its cross-sectional and longitudinal associations with hip pain, MRI findings and early radiographic hip OA. BMC Musculoskelet Disord 21(1):533. https://doi.org/10.1186/s12891-020-03532-7
Kumar D, Wyatt CR, Lee S, Nardo L, Link TM, Majumdar S, Souza RB (2013) Association of cartilage defects, and other MRI findings with pain and function in individuals with mild-moderate radiographic hip osteoarthritis and controls. Osteoarthr Cartil 21(11):1685–1692. https://doi.org/10.1016/j.joca.2013.08.009
Taljanovic MS, Graham AR, Benjamin JB, Gmitro AF, Krupinski EA, Schwartz SA, Hunter TB, Resnick DL (2008) Bone marrow edema pattern in advanced hip osteoarthritis: quantitative assessment with magnetic resonance imaging and correlation with clinical examination, radiographic findings, and histopathology. Skeletal Radiol 37(5):423–431. https://doi.org/10.1007/s00256-008-0446-3
Kijima H, Yamada S, Konishi N, Kubota H, Tazawa H, Tani T, Suzuki N, Kamo K, Okudera Y, Fujii M, Sasaki K, Kawano T, Iwamoto Y, Nagahata I, Miura T, Miyakoshi N, Shimada Y (2020) The differences in imaging findings between painless and painful osteoarthritis of the hip. Clin Med Insights Arthritis Musculoskelet Disorders 13:1179544120946747. https://doi.org/10.1177/1179544120946747
Heerey JJ, Srinivasan R, Agricola R, Smith A, Kemp JL, Pizzari T, King MG, Lawrenson PR, Scholes MJ, Souza RB, Link T, Majumdar S, Crossley KM (2021) Prevalence of early hip OA features on MRI in high-impact athletes. The femoroacetabular impingement and hip osteoarthritis cohort (FORCe) study. Osteoarthr Cartil 29(3):323–334. https://doi.org/10.1016/j.joca.2020.12.013
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O’Connell D, Oxman AD, Phillips B, Schünemann HJ, Edejer T, Varonen H, Vist GE, Williams JW Jr., Zaza S (2004) Grading quality of evidence and strength of recommendations. BMJ (Clinical Res ed) 328(7454):1490. https://doi.org/10.1136/bmj.328.7454.1490
Yusuf E, Kortekaas MC, Watt I, Huizinga TW, Kloppenburg M (2011) Do knee abnormalities visualised on MRI explain knee pain in knee osteoarthritis? A systematic review. Ann Rheum Dis 70(1):60–67. https://doi.org/10.1136/ard.2010.131904
Jaremko JL, Lambert RG, Zubler V, Weber U, Loeuille D, Roemer FW, Cibere J, Pianta M, Gracey D, Conaghan P, Ostergaard M, Maksymowych WP (2014) Methodologies for semiquantitative evaluation of hip osteoarthritis by magnetic resonance imaging: approaches based on the whole organ and focused on active lesions. J Rhuematol 41(2):359–369. https://doi.org/10.3899/jrheum.131082
Download references
Acknowledgements
No AI or editing software was employed for writing and editing this manuscript.
Open Access funding enabled and organized by CAUL and its Member Institutions. This work is supported by the National Natural Science Foundation of China (NSFC, 82103933) and the Scientific Research Level Upgrading Project of Anhui Medical University (2021xkjT006).
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and affiliations.
Department of Epidemiology and Biostatistics, School of Public Health, Anhui Medical University, Hefei, 230032, Anhui, China
Haonan Fang, Xiaoyue Zhang, Junjie Wang, Xing Xing, Ziyuan Shen & Guoqi Cai
Menzies Institute for Medical Research, University of Tasmania, Hobart, TAS, 7000, Australia
Ziyuan Shen & Guoqi Cai
You can also search for this author in PubMed Google Scholar
Contributions
The guarantor (GC) had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. GC conceived, initiated, and supervised the project. CG, HF and XZ cleaned and analyzed the data. HF, XZ, JW, XX, ZY and GC contributed to the interpretation of the results and writing and revision of the manuscript. All authors gave final approval of the version submitted. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Correspondence to Guoqi Cai .
Ethics declarations
Ethics approval.
Inapplicable.
Conflict of interest
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Fang, H., Zhang, X., Wang, J. et al. The relationship between MRI-detected hip abnormalities and hip pain in hip osteoarthritis: a systematic review. Rheumatol Int (2024). https://doi.org/10.1007/s00296-024-05678-2
Download citation
Received : 30 April 2024
Accepted : 03 August 2024
Published : 13 August 2024
DOI : https://doi.org/10.1007/s00296-024-05678-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hip osteoarthritis
- Magnetic resonance imaging
- Find a journal
- Publish with us
- Track your research
- Qazi Corner
- Biosimilars Spotlight
- DME & nAMD On-Demand Presentation

- Multimedia Series
- Conferences
- Advisory Board
Case Study: 40-year-old man with joint pain
A 40-year-old man presents to his primary care doctor complaining of pain in his ankles, knees, feet, heels, lower back and buttocks. What's your diagnosis?

A 40-year-old man presents to his primary care doctor complaining of pain in his ankles, knees, feet, heels, lower back and buttocks. What's your diagnosis? (©Angkhan,AdobeStock)

A 40-year-old man presents to his primary care doctor complaining of pain in his ankles, knees, feet, heels, lower back and buttocks. His eye also appears to be inflamed. And, he reports having a burning sensation when urinating, which has become much more frequent. He has been experiencing these symptoms for three months and at times, the joint pain is so severe, he is bedridden.
The patient reports not having fallen or injured himself, nor does he have a history of painful joints or other arthritic condition. He stated that he has always been in excellent health.
The patient is exhibiting signs of:
A) SpA B) Sciatica C) Reactive arthritis D) Chlamydia infection of the lower urinary tract E) Age-related wear and tear on joints
See the next page for the answer…
Answer: C and D
This patient is exhibiting signs of reactive arthritis possibly caused by a chlamydia infection of the lower urinary tract. Reactive arthritis is usually caused by an infection, such as C. trachomatis, or infections of the gut such as a salmonella infection. It is also more common in patients with a family history of spondyloarthritis, which includes ankylosing spondylitis, psoriatic arthritis and arthritis associated with inflammatory bowel diseases.
The likelihood of developing reactive arthritis is higher-approximately 30-50 percent-for patients who have the gene HLA-B27. Its presence can indicate the severity of the course of disease.
In HLA-B27 positive patients, the condition can be triggered by an infection. According to a study published in 2000 in the journal Arthritis and Rheumatology, 75 percent of patients with a salmonella infection were positive for HLA-B27. These gene carriers who have reactive arthritis may also have conjunctivitis or anterior uveitis. They may also have severe disease with spine involvement and frequent arthritis flares, especially of the lower extremities. And, they are more likely to present with extra-articular features as urethritis, mucocutaneous lesions (circinate balanitis, keratoderma blennorrhagicum and nail dystrophy), cardiac and neurological involvement, amyloidosis, thrombophlebitis, pleuritis and ocular involvement.
“Overall, patients who show the classical triad arthritis, urethritis and conjunctivitis, have a poorer prognosis,” wrote Manuela Di Franco, M.D., of the University of Rome, Italy, in a review article published in the journal Clinical and Experimental Rheumatology published earlier this year.
---- Related article "A Review of Reactive Arthritis"
REFERENCE B. Lucchino, F. R. Spinelli, C. Perricone, et al. “Reactive arthritis: current treatment challenges and future perspectives.” Clinical and Experimental Rheumatology . May 22, 2019

Emerging Agents in the Treatment of Rheumatic Diseases

Vitamin D Associated With Lower Risk of Mortality in Patients With Gout, Hyperuricemia

Challenges with Step Therapy Protocols in Treating Rheumatoid Arthritis

Bimekizumab Shows Consistent Efficacy With Or Without Concomitant Methotrexate in PsA

Study Reveals Higher Economic, Quality of Life Burden With Rheumatoid Arthritis
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
Website maintenance is scheduled for Saturday, August 17, and Sunday, August 18. Short disruptions may occur during these days.

RAMSEY SHEHAB, MD, AND MARK H. MIRABELLI, MD
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2013;87(8):568-573
Author disclosure: No relevant financial affiliations.
Patients with wrist pain commonly present with an acute injury or spontaneous onset of pain without a definite traumatic event. A fall onto an outstretched hand can lead to a scaphoid fracture, which is the most commonly fractured carpal bone. Conventional radiography alone can miss up to 30 percent of scaphoid fractures. Specialized views (e.g., posteroanterior in ulnar deviation, pronated oblique) and repeat radiography in 10 to 14 days can improve sensitivity for scaphoid fractures. If a suspected scaphoid fracture cannot be confirmed with plain radiography, a bone scan or magnetic resonance imaging can be used. Subacute or chronic wrist pain usually develops gradually with or without a prior traumatic event. In these cases, the differential diagnosis is wide and includes tendinopathy and nerve entrapment. Overuse of the muscles of the forearm and wrist may lead to tendinopathy. Radial pain involving mostly the first extensor compartment is commonly de Quervain tenosynovitis. The diagnosis is based on history and examination findings of a positive Finkelstein test and a negative grind test. Nerve entrapment at the wrist presents with pain and also with sensory and sometimes motor symptoms. In ulnar neuropathies of the wrist, the typical presentation is wrist discomfort with sensory changes in the fourth and fifth digits. Activities that involve repetitive or prolonged wrist extension, such as cycling, karate, and baseball (specifically catchers), may increase the risk of ulnar neuropathy. Electrodiagnostic tests identify the area of nerve entrapment and the extent of the pathology.
Musculoskeletal problems are responsible for up to 20 percent of all visits to primary care offices in the United States. 1 Family physicians are often the first to evaluate and treat wrist pain. Wrist pain is traditionally classified as acute pain caused by a specific injury or as subacute/chronic pain not caused by a traumatic event ( Tables 1 and 2 ) . Injuries that cause acute pain may result in contusions, fractures, ligament sprains or tears, and instability. Subacute or chronic pain may result from overuse, have neurologic or systemic causes, or be a sequela from an old injury. Patients with these injuries may have a history of repetitive wrist movement, either occupationally or recreationally. The addition of sensory disturbances, such as numbness or tingling, points to nerve involvement.
| Anatomic snuffbox swelling, scaphoid tubercle tenderness, and pain with axial pressure on the first metacarpal bone are sensitive but not specific tests for diagnosing scaphoid fractures. | C | , |
| If plain radiography results are negative in a suspected scaphoid fracture, then the wrist should be protected in a thumb spica cast with repeat plain radiography in 10 to 14 days or a bone scan one to two days after injury. | C | , |
| The Finkelstein test has good sensitivity and specificity for diagnosing de Quervain tenosynovitis. | C | , |
| Carpal instability | Trauma, carpal tenderness, audible clunk with radial or ulnar deviation | Radiography with views in radial/ulnar deviation or advanced imaging (CT, MRI, bone scan) |
| Fracture | Trauma, bony tenderness | Radiography or advanced imaging (CT, MRI, bone scan) |
| Joint subluxation | Trauma, instability with movement | Radiography or MRI |
| Ligament tears | Trauma, painful motion | MRI |
| Neurologic (ulnar, median, and radial nerve entrapment) | Pain with sensory and possibly motor difficulties | Radiography, electrodiagnostic tests |
| Old trauma (nonunion, avascular necrosis) | Remote history of injury with noimprovement | Plain radiography, magnetic resonance imaging |
| Systemic (rheumatoid arthritis, amyloidosis, gout) | Constitutional symptoms, swelling, constant pain | Complete blood count, erythrocyte sedimentation rate, C-reactive protein level |
| Tendinopathy | Painful movement | Tests usually not needed |
History and physical examination lead to the correct diagnosis in most cases. The location, nature, timing, and quality of the pain are important clues for narrowing the differential diagnosis. In acute wrist injuries, plain radiography should be obtained with anteroposterior, lateral, and oblique views. When the diagnosis remains unclear, further imaging, such as bone scan, ultrasonography, computed tomography, or magnetic resonance imaging (MRI), may help identify the cause. Because nontraumatic wrist pain has a wide differential diagnosis, the patient history should include a review of systems with neurologic or constitutional symptoms, as well as a social history of vocational and recreational activities. The following case studies discuss the background and presentation of three causes of wrist pain, as well as diagnostic tests and strategies.
Case 1. Scaphoid Fracture
A 21-year-old man presents with dorsal left wrist pain after falling onto his outstretched hand while inline skating. He noted immediate swelling and painful wrist extension. Physical examination reveals soft tissue swelling with limited motion, mostly in extension, secondary to pain. There is bony tenderness along the distal radius as well as the anatomic snuff box. His sensory and vascular examination results are unremarkable.
The wrist comprises eight carpal bones ( Figure 1 2 ) , but only the lunate and scaphoid articulate with the radius and absorb significant impact during a fall onto an outstretched hand. The scaphoid is the most commonly fractured carpal bone. The primary vascular supply to the scaphoid originates distally from retrograde branches of the distal radial artery, making the proximal pole of the scaphoid relatively avascular and at higher risk of nonunion and avascular necrosis. Fractures of the proximal and distal portions of the scaphoid each account for 20 percent of scaphoid fractures, and the middle portion accounts for the remaining 60 percent. 3
The peak incidence of scaphoid fractures occurs at about 15 years of age. 4 Because of the weakness of the distal radius compared with the scaphoid, scaphoid fractures are not common in older persons. In young children, the supportive cartilage surrounding the ossific nucleus of the immature scaphoid creates protection, making physeal injuries of the radius more common.
PRESENTATION
The typical history of a patient with a scaphoid fracture is a fall onto an outstretched hand with the wrist dorsiflexed and radially deviated. Most patients with scaphoid fractures present shortly after a fall, but in some cases, the initial pain improves, causing a delayed presentation.
Physical examination may reveal a swollen wrist. Tenderness is usually located dorsally around the distal radius. Patients may have painful wrist extension and loss of grip strength if they present a few days after the injury.
There are no reliable clinical tests to rule out a scaphoid fracture. Swelling of the anatomic snuff box ( Figure 2 5 ) increases the likelihood of a scaphoid facture. The combination of snuff box swelling, scaphoid tubercle tenderness, and pain with axial pressure on the first metacarpal bone has a sensitivity of approximately 100 percent. 6 However, the specificity of each test is 9, 30, and 48 percent, respectively. 6 Diminished grip strength compared with the contralateral side increases the positive predictive value for a scaphoid fracture. 7 The differential diagnosis of a suspected scaphoid fracture is listed in Table 3 .
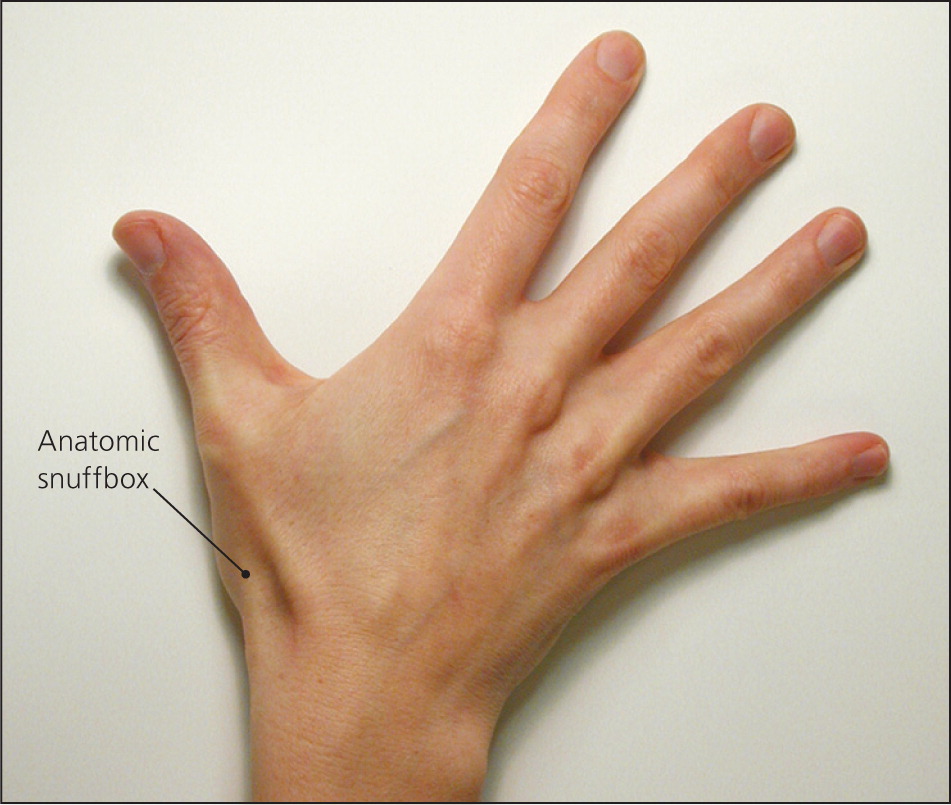
| Carpometacarpal dislocation | Radiographic finding of joint space loss(1 to 2 mm) in carpometacarpal joints |
| Distal radial fracture | Radiographic findings of fracture, tenderness to distal radius |
| Lunate fracture | Radiographic findings of fracture, tenderness to lunate |
| Scapholunate tear | Radiographic finding of scapholunate widening (greater than 3 mm) |
DIAGNOSTIC TESTS
Conventional radiography (anteroposterior, lateral, and oblique views) alone can miss up to 30 percent of scaphoid fractures. 8 Based on retrospective studies, sensitivity improves if additional views are added (i.e., posteroanterior in ulnar deviation, pronated oblique, and supinated oblique). 8 In many cases, repeat radiography is needed in 10 to 14 days to observe sclerosis, which indicates a healing fracture.
If the diagnosis cannot be confirmed with plain radiography, a bone scan or MRI can be performed. Bone scan has a sensitivity near 100 percent but produces false-positive results up to 25 percent of the time. 9 MRI within one day after trauma has a sensitivity of 80 percent, 10 but late examination (more than 10 days after injury) has a sensitivity and specificity comparable to bone scan. 11
DIAGNOSTIC STRATEGY
If a scaphoid fracture is suspected based on history and physical examination, plain radiography should be performed, including specialized views such as a posteroanterior in ulnar deviation and a pronated oblique. If radiography is negative for fracture but clinical suspicion is high, the wrist should be protected in a thumb spica cast with the option of repeat plain radiography in 10 to 14 days or a bone scan one to two days after injury. 4 , 5 If repeat plain radiography is negative but wrist pain persists, MRI should be performed to clarify the diagnosis.
Case 2. Ulnar Neuropathy
A 39-year-old right-handed woman presents with a four-week history of wrist pain and numbness and tingling in her right hand. There is no history of trauma or injury to the neck, elbow, or wrist. She works mostly at a desk job but has not had any changes in her work schedule. Physical examination of the wrist reveals no soft tissue swelling, muscle atrophy, or skin changes. She has painful wrist extension, as well as reproduction of the tingling in her fifth finger with tapping over the pisiform. Grip strength is normal and no other bony tenderness is appreciated.
The ulnar nerve originates from the C8 and T1 nerve roots ( Figure 3 12 ) , and extends from the medial cord of the brachial plexus through the axilla, innervating the muscles of the forearm and the hand. Proximal to the wrist, dorsal and palmar cutaneous branches split off, whereas the rest of the nerve courses through the Guyon canal ( Figure 4 ) to the palmar surface of the hand. This triangular canal is bordered medially by the pisiform, laterally by the hamate, anteriorly by the tendon of the flexor carpi ulnaris, and posteriorly by the transverse carpal ligament. In the canal, the ulnar nerve splits to a superficial sensory branch, which supplies sensation to the hypothenar eminence, and to a deep motor branch that innervates the hypothenar muscles, adductor pollicis, and flexor pollicis brevis. The ulnar nerve may be compressed anywhere in the Guyon canal, causing motor, sensory, or mixed deficits. Compression is usually caused by ganglion cysts or repetitive trauma.
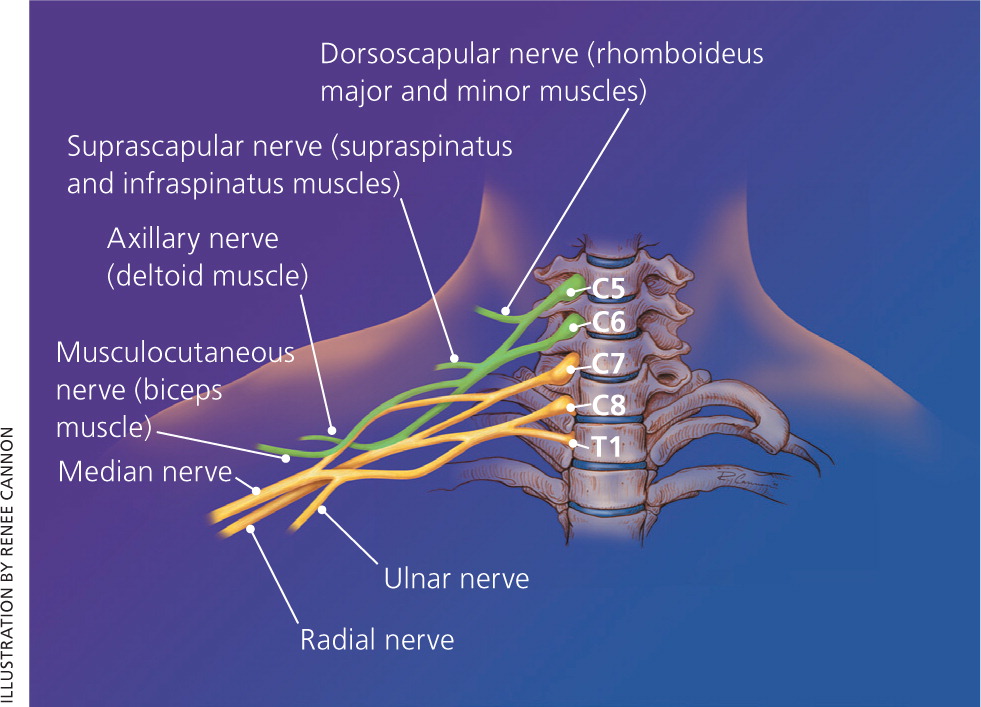
Ulnar nerve entrapment is the second most common neuropathy of the upper extremity, surpassed only by median nerve entrapment (i.e., carpal tunnel syndrome). 13 Although the true incidence of ulnar neuropathy at the wrist is not well documented, it is accepted to be the second most common site after compression at the elbow. Ulnar neuropathies are slightly more common in men than in women. Peak incidence is in men older than 35 years. 14
The typical presentation in ulnar neuropathy is wrist discomfort with sensory changes in the fourth and fifth digits. Grip weakness may be present in chronic cases. History usually reveals no specific injury. Activities that involve repetitive or prolonged wrist extension, such as cycling, karate, and baseball (specifically catchers) may increase the risk of ulnar neuropathy. 15
Physical examination of a patient presenting with these neurologic symptoms should include cervical spine, shoulder, and elbow examinations to rule out a proximal lesion. Reproduction of pain on neck movement could indicate cervical disk disease; pain with shoulder motion could indicate a brachial plexus problem; and reproduction of symptoms with compression of the nerve at the ulnar groove could indicate compression at the elbow. Compression of the ulnar nerve at the Guyon canal should cause weakness of the hypothenar muscles innervated by the deep motor branch and sensory disturbances of the fifth digit innervated by the superficial sensory branch.
Clinical tests include a positive Tinel sign on percussion of the ulnar nerve over the Guyon canal, as well as a positive Phalen sign (maximum passive flexion of the wrist for more than one minute) with paresthesias in the fourth and fifth fingers. Unlike in carpal tunnel syndrome, sensitivity and specificity of these tests for ulnar neuropathy at the wrist are not known. The differential diagnosis of suspected ulnar neuropathy at the wrist is listed in Table 4 .
| Brachial plexopathy | History of shoulder/arm pain, motor weakness of upper extremity |
| Cervical radiculopathy | History of neck pain, forearm symptoms (e.g., pain, numbness, tingling) |
| Ulnar neuropathy at the elbow | Elbow pain |
| Wrist fracture | Traumatic injury, positive radiographic findings |
Plain radiography evaluates wrist anatomy well, and can identify fractures, dislocations, or soft tissue masses that may have led to nerve compression.
Ultrasonography of peripheral nerves is helpful in identifying compressive etiologies of nerve injury and in visualizing structural nerve changes. It is noninvasive, relatively inexpensive, and well tolerated by patients.
Electromyography and nerve conduction studies can be helpful in identifying the area of entrapment and documenting the extent of the pathology. Motor and sensory conduction velocities are more useful in acute entrapments, whereas electromyography is a better choice for chronic neuropathies because it shows axonal degeneration more clearly. The sensitivity and specificity of these electrodiagnostic tests in the primary care setting are unknown because existing studies are limited to a small number of patients with known neuropathy.
MRI can detect abnormalities of the ulnar nerve, flexor tendons, vascular structures, and the transverse carpal ligament around the Guyon canal. Neurogenic edema can be seen as early as 24 to 48 hours after denervation compared with electromyography, in which changes after denervation are not seen for one to three weeks. 16 Imaging criteria for neuropathy on MRI are not well defined, and several studies have found MRI abnormalities in healthy, asymptomatic patients. 17
If ulnar neuropathy is suspected, plain radiography should be ordered first. If no obvious mass or lesion is found, electrodiagnostic tests should be ordered to localize the lesion, measure its severity, and aid in the prognosis. In the setting of inconclusive or nonlocalizing electrodiagnostic test results, ultrasonography or MRI may be useful.
Case 3. De Quervain Tenosynovitis
A 31-year-old woman presents with several months of worsening radial left wrist pain that started insidiously. She denies any specific trauma. She has no numbness or tingling in the wrist, hand, or fingers. Her pain worsens with gripping and grasping, and with picking up her nine-month-old daughter. Physical examination reveals no discoloration and minimal soft tissue swelling along the radial styloid and anatomic snuff box. There is soft tissue tenderness about the anatomic snuff box and radial styloid. She has limited motion of the thumb, with pain mostly in extension and abduction. Her sensory and vascular examinations are unremarkable.
Two major dorsal tendons of the thumb are involved: the extensor pollicis brevis and the abductor pollicis longus ( Figure 5 ) . [ corrected ] These tendons comprise the lateral border of the anatomic snuffbox, with the extensor pollicis longus medially and the scaphoid bone at the bottom. The two tendons have similar function in bringing the thumb into radial abduction. These tendons run in a synovial sheath in the first extensor compartment of the hand. Inflammatory changes in the sheath and tendons result in a tenosynovitis. Recurrent or persistent inflammation may result in stenosing tenosynovitis.
The typical presentation includes subacute radial wrist pain at the thumb base and into the distal radius. In retrospect, patients may identify a new or repetitive hand-based activity as the cause, but the etiology often is idiopathic. De Quervain tenosynovitis is more common in women, particularly those 30 to 50 years of age. 18 New mothers are especially noted to have this problem from picking up a child. 19
Physical examination may reveal a minimally swollen wrist. Tenderness is usually located over the radial tubercle and sometimes around the soft tissues of the anatomic snuff box. Thumb motion is invariably painful. Neurovascular examination should be unremarkable. The Finkelstein test is confirmatory because it has good sensitivity and specificity. 18 , 20 It is performed by making a fist over the thumb and then moving the hand into ulnar deviation, which passively stretches the thumb tendons over the radial styloid. 20 , 21 A grind test of the thumb, which is performed by axial compression and slight rotation of the metacarpophalangeal joint, should be negative in those with de Quervain tenosynovitis but positive in those with first carpometacarpal osteoarthritis. The differential diagnosis of suspected de Quervain tenosynovitis is listed in Table 5 .
| Ganglion cyst | Visual appearance of cyst-like structure |
| Osteoarthritis of the first extensor compartment | Radiographic findings of osteoarthritis |
| Radial nerve entrapment of the forearm | Electromyographic findings |
| Wrist extensor tendinopathy | Clinical examination findings |
The diagnosis is clinical based on history and examination. In cases where osteoarthritis of the carpometacarpal joint is considered, pain relief with diagnostic lidocaine (Xylocaine) injection of the first extensor compartment excludes arthritic cause. Radiography, electromyography/nerve conduction studies, blood tests, and MRI or ultrasonography may be used to evaluate for alternative diagnoses.
If the history and examination are consistent, no further diagnostic testing is needed. For suspicion of fracture or arthritis, radiography is an appropriate first step. If suspected, radial nerve abnormalities may be ruled out with electromyography or nerve conduction studies. If there is concern for infectious tenosynovitis, a complete blood count and measurement of inflammatory markers, such as erythrocyte sedimentation rate and C-reactive protein levels, are appropriate. If the patient does not respond to treatment or if the diagnosis is in question, an MRI or musculoskeletal ultrasonography may be ordered to further evaluate the first extensor compartment. 19 , 22
Data Sources: A PubMed search was completed in Clinical Queries using the key terms scaphoid fracture, ulnar neuropathy, and de Quervain's. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were Essential Evidence Plus, the Cochrane database, the National Guideline Clearinghouse, and UpToDate. Search date: August 2011.
Jordan K, Clarke AM, Symmons DP, et al. Measuring disease prevalence: a comparison of musculoskeletal disease using four general practice consultation databases. Br J Gen Pract. 2007;57(534):7-14.
Daniels JM, Zook EG, Lynch JM. Hand and wrist injuries: part I. Non-emergent evaluation. Am Fam Physician. 2004;69(8):1941-1948.
Dobyns JH, Beckenbaugh RD, Bryan RS, et al. Fractures of the hand and wrist. In: Flynn JE, ed. Hand Surgery . 3rd ed. Baltimore, Md.: Williams & Wilkins; 1982.
Ingari JV. The adult wrist. In: DeLee JC, Drez D, Miller MD, eds. DeLee & Drez's Orthopaedic Sports Medicine. 3rd ed. Philadelphia, Pa.: Saunders; 2009.
Phillips TG, Reibach AM, Slomiany WP. Diagnosis and management of scaphoid fractures. Am Fam Physician. 2004;70(5):879-884.
Freeland P. Scaphoid tubercle tenderness: a better indicator of scaphoid fractures?. Arch Emerg Med. 1989;6(1):46-50.
Grover R. Clinical assessment of scaphoid injuries and the detection of fractures. J Hand Surg Br. 1996;21(3):341-343.
Cheung GC, Lever CJ, Morris AD. X-ray diagnosis of acute scaphoid fractures. J Hand Surg Br. 2006;31(1):104-109.
Tiel-van Buul MM, van Beek EJ, Borm JJ, Gubler FM, Broekhuizen AH, van Royen EA. The value of radiographs and bone scintigraphy in suspected scaphoid fracture. A statistical analysis. J Hand Surg Br. 1993;18(3):403-406.
Beeres FJ, Rhemrev SJ, den Hollander P, et al. Early magnetic resonance imaging compared with bone scintigraphy in suspected scaphoid fractures. J Bone Joint Surg Br. 2008;90(9):1205-1209.
Fowler C, Sullivan B, Williams LA, McCarthy G, Savage R, Palmer A. A comparison of bone scintigraphy and MRI in the early diagnosis of the occult scaphoid waist fracture. Skeletal Radiol. 1998;27(12):683-687.
Miller JD, Pruitt S, McDonald TJ. Acute brachial plexus neuritis: an uncommon cause of shoulder pain. Am Fam Physician. 2000;62(9):2067-2072.
Elhassan B, Steinmann SP. Entrapment neuropathy of the ulnar nerve. J Am Acad Orthop Surg. 2007;15(11):672-681.
Gay JR, Love JG. Diagnosis and treatment of tardy paralysis of the ulnar nerve; based on a study of 100 cases. J Bone Joint Surg Am. 1947;29(4):1087-1097.
Brukner P, Bahr R, Blair S, et al., eds. Brukner & Khan's Clinical Sports Medicine . 4th ed. New York, NY: McGraw-Hill; 2012.
Vucic S, Cordato DJ, Yiannikas C, Schwartz RS, Shnier RC. Utility of magnetic resonance imaging in diagnosing ulnar neuropathy at the elbow. Clin Neurophysiol. 2006;117(3):590-595.
Husarik DB, Saupe N, Pfirrmann CW, Jost B, Hodler J, Zanetti M. Elbow nerves: MR findings in 60 asymptomatic subjects—normal anatomy, variants, and pitfalls. Radiology. 2009;252(1):148-156.
Wolf JM, Sturdivant RX, Owens BD. Incidence of de Quervain's tenosynovitis in a young, active population. J Hand Surg Am. 2009;34(1):112-115.
Anderson SE, Steinbach LS, De Monaco D, Bonel HM, Hurtienne Y, Voegelin E. “Baby wrist”: MRI of an overuse syndrome in mothers. AJR Am J Roentgenol. 2004;182(3):719-724.
Dawson C, Mudgal CS. Staged description of the Finkelstein test. J Hand Surg Am. 2010;35(9):1513-1515.
Crop JA, Bunt CW. “Doctor, my thumb hurts.”. J Fam Pract. 2011;60(6):329-332.
Diop AN, Ba-Diop S, Sane JC, et al. Role of US in the management of de Quervain's tenosynovitis: review of 22 cases. J Radiol. 2008;89(9 pt 1):1081-1084.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2013 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Musculoskeletal Key
Fastest musculoskeletal insight engine.
- MANUAL THERAPIST
- MUSCULOSKELETAL MEDICINE
- PHYSICAL MEDICINE & REHABILITATION
- RHEUMATOLOGY
- SPORT MEDICINE
- Gold Membership
Case studies in a musculoskeletal out-patients setting
CHAPTER EIGHT Case studies in a musculoskeletal out-patients setting Adrian Schoo, Nick Taylor, Ken Niere, with a contribution from James Selfe Case study 1: Jaw Pain 217 Case study 2: Headache 218 Case study 3: Neck Pain – Case One 221 Case study 4: Neck Pain – Case Two 224 Case study 5: Thoracic Pain 226 Case study 6: Low Back Pain – Case One 228 Case study 7: Low Back Pain – Case Two 231 Case study 8: Shoulder Pain 234 Case study 9: Elbow Pain 237 Case study 10: Hand Weakness and Pain 239 Case study 11: Groin Pain 241 Case study 12: Hip and Thigh Pain 244 Case study 13: Medial Knee Pain 247 Case study 14: Anterior Knee Pain 249 Case study 15: Calf Pain 252 Case study 16: Achilles Pain 254 Case study 17: Ankle Sprain 256 Case study 18: Fibromyalgia 258 Introduction Musculoskeletal problems are very common, and can be encountered in hospital emergency departments, orthopaedics, and out-patient physiotherapy ( Carter & Rizzo 2007 ). It is not uncommon for in-patients who are admitted for another problem to be referred and treated in the ward or in the out-patient department for a musculoskeletal problem. The prevalence of specific conditions can vary between the different groups in the community. For example, sporting injuries are more likely to occur in the younger groups, whereas degenerative conditions such as osteoarthritis are more likely to occur as people progress in years. Musculoskeletal problems can result in pain and functional limitations (disability), and represent a major burden to the society due to associated health care costs and loss of productivity ( National Health Priority Action Council 2004 ). Musculoskeletal conditions, including arthritis, cause more disability than any other medical condition and affect one-third of all people with disability. Since part of the chronic disease burden is attributed to risk factors such as physical inactivity ( Bauman 2004 ) people with musculoskeletal conditions are often referred to physiotherapy out-patients for management of their conditions. As in other areas of physiotherapy practice, musculoskeletal assessment and treatment requires a systematic clinical reasoning approach ( Edwards et al 2004 ). The clinical reasoning approach used in this chapter considers: (i) differential diagnoses based on assessment and clinical presentation; (ii) intervention based on the best evidence available; (iii) constant evaluation of therapy outcomes; (iv) adjustment of intervention programme in line with diagnosis and stage of progress; and (v) referring to or working together with other disciplines to exclude and or address confounding problems. In assessing and treating common musculoskeletal conditions and measuring progress it is important to use outcome measures that are valid and reliable, and that consideration must be given to impairments of body structure and function as well as activity limitation and participation restriction, such as ability to return to work. The World Health Organization’s International Classification of Functioning, Disability and Health (ICF) provides a useful framework for physiotherapists in out-patients to assess patient functioning ( Jette 2006 ). Referral to or working with other disciplines may involve tests such as X-rays or dynamic ultrasound scans, or the provision of orthotics to improve biomechanics. In addition to specific techniques, treatment may require education, ergonomic advice and the instruction of a home exercise programme to improve outcomes on function and pain. There is an emerging and increasing body of research on the effectiveness of physiotherapy that provides the clinician in out-patients with an evidence base for their practice ( Herbert et al 2001 ). For example, there is high level evidence that therapeutic exercise can benefit clients across broad areas of physiotherapy practice ( Morris & Schoo 2004 , Taylor et al 2007 ). In prescribing exercises it can be important to know whether the exercise programme is performed correctly and adhered to by the client. Conditions such as back problems or tendinopathies may be negatively affected by incorrect activity performance. Additional problems that can affect health outcomes are incorrect belief systems and mental health problems. For instance, people with osteoarthritis may think that movement harms the joint, but by not moving they put themselves at risk of developing problems associated with physical inactivity (e.g. increased morbidity and mortality due to cardiovascular problems or falls) ( Philbin et al 1996 ). Also, people with chronic pain may be depressed and are, therefore, less likely to be interested in performing exercises, and may benefit from counselling (e.g. motivational interviewing). Screening patients for problems such as fear-avoidance behaviour and anxiety ( Andrews & Slade 2001 ), asking about past and current exercise performance, motivating them if needed (Friedrich et al 1998) and demonstrating the prescribed exercises can assist in determining the likelihood of correct and consistent programme performance (Friedrich et al 1996b, Schneiders et al 1998 ). We have selected common musculoskeletal conditions that are likely to be encountered in hospital out-patient departments. The different cases relate to younger and older people, females as well as males. A multitude of physical tests and outcome measures have been included together with clinical reasoning and evidence-based treatment options. CASE STUDY 1 Jaw pain Subjective examination Subject 34-year-old female office worker HPC Left sided headaches off and on for 3/12 Increasing pain of the left temporomandibular joint (TMJ) last 2/12 Pain at night, at rest, and when opening the mouth or chewing PMH Appendectomy Stress at work Aggravating factors Biting a big apple Chewing hard or tough food Easing factors Rest is better than chewing, although remains painful Drinking fluid Ice Night Wakes up because of pain Grinds teeth when asleep (according to partner) Daily pattern Constant pain that worsens during and directly after opening the mouth or chewing General health Using prescribed sedatives due stress at work. No other problems reported Attitude/expectations Given the symptoms she expects that it may take some time for them to settle Pain and dysfunction scores VAS current pain at rest = 3 VAS usual level of pain during chewing in the last week = 7 VAS worst level of pain during opening the mouth in the last week = 9 Objective examination Palpation Skin temperature (T sk ) normal Left TMJ painful on palpation TMJ movement and clicking can be felt when placing the index finger in the auditory canal and opening the mouth No signs of TMJ dislocation when comparing left with right Muscle length External pterygoid muscle feels tight and painful on opening of the mouth (palpation through the mouth) Functional testing, including ROM and strength Opening of the mouth is limited. It can accommodate two fingers only. Normally, the span is large enough to accommodate three fingers ( Hoppenfield 1986 ) Asymmetrical mandibular motion with severe swinging to the left when opening the mouth Questions 1. What is your provisional diagnosis? 2. What signs and symptoms lead you to this diagnosis? 3. How will you address these in your treatment plan? 4. What kind of common and less common problems need to be excluded? 5. How likely is it that the patient’s stress and teeth grinding contribute to the current complaint? 6. How will the expectations of the patient influence your treatment? 7. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 2 Headache Subjective examination Subject 29-year-old male working on Help Desk in Information and Computer Technology HPC Gradual onset of headaches and cervical pain about 3/52 ago Cannot recall precipitating incident Headaches becoming more frequent (now daily) and lasting longer (up to 3 hours) Has deep ache (non-throbbing) radiating from the back of the occiput to the right frontal region. Also complaining of stiffness like pain in the right side of the cervical spine. Neck pain and headache seem related (see Figure 8.1 ) FIGURE 8.1 Body chart – Case Study 2 . PMH Car accident 10 years ago which led to cervical pain for about 3/52. No problems since apart from an occasional stiff neck Aggravating factors Prolonged work at the computer (if more than 2 hours brings on headache) Reversing the car reproduces slight cervical stiffness Easing factors Analgesia dulls the headache Night Sleep undisturbed Daily pattern Seems to depend on how long he has spent at the computer General health In good health, no weight loss No complaints of dizziness, no nausea or vomiting Assessed as being depressed, has been taking antidepressants over the last 3/12 Investigations No X-rays or other investigations at this stage Attitude/expectations At the moment headache is not affecting him a lot but wanted to get it checked out in case it is something serious Keen not to miss any work Intends to continue normal recreation of sail boarding this weekend Pain and dysfunction scores Neck Disability Index: 14% Disability VAS level of pain when headache is most severe (after working at the computer for 2 hours) = 6 Physical examination Observation Forward head posture with a slouched sitting posture Palpation Hypo-mobility of upper cervical joints on the right, with reproduction of local cervical pain Increased muscle tone in right upper trapezius and right levator scapulae Movements Active movements Right cervical rotation equals 60° with slight stiffness in neck Left cervical rotation equals 75–80° Limited cervical retraction, feels stiff Muscle function Decreased strength and endurance of the deep cervical neck flexors as determined by the cranio-cervical flexion test ( Jull et al 1999 ) Neurodynamic testing Upper limb neurodynamic/tension test (base test): In 90° shoulder abduction and full external rotation, right elbow extension lacks 40° while left lacks 30°. Reproducing local neck pain, which is eased with cervical lateral flexion towards the right Neurological tests (tests of nerve conduction) Not assessed Questions 1. What is your provisional diagnosis? 2. What signs and symptoms led to your provisional diagnosis? 3. How will you address these in your treatment plan? 4. What kind of common and less common problems need to be excluded? 5. How relevant are work details for this patient? 6. How will the expectations of the patient influence your treatment? 7. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 3 Neck pain – case one Subjective examination Subject 32-year-old male accountant HPC Prolonged sitting (all day) at a conference 3/52 previously Noticed onset of left lower cervical and interscapular pain at the end of the day On waking the next morning pain had spread to the posterior aspect of the arm and forearm as far as the middle three fingers (see Figure 8.2 ) FIGURE 8.2 Body chart – Case Study 3 . Seen by doctor 1/52 ago. Doctor ordered plain X-rays including oblique views that did not show any abnormality Has not improved at all since onset of symptoms Medical history High cholesterol, overweight, sedentary lifestyle Minor neck complaints that usually settled within 2 or 3 days Aggravating factors Sitting for more than 10 minutes increases neck pain. More than 30 minutes increases arm pain Looking up or to the left increases neck and arm pain Lifting briefcase with left hand aggravates neck and interscapular pain Easing factors Neck pain relieved by lying supine Arm pain relieved by lying supine with left arm above head Night Can sleep 2–3 hours at a time before being woken by increased neck and interscapular pain Changing position helps to decrease the pain Daily pattern Increased symptoms with increased amounts of sitting, particularly if using computer Medication Was prescribed non-steroidal anti-inflammatory medication (Meloxicam) which helps take the edge off the neck pain Attitude/expectations Wants to know what the problem is, particularly as the X-rays did not show any abnormality Feels that something might be ‘out’ in his neck. If it could be ‘put back in’ the symptoms should resolve Physical examination Observation Sits with forward head posture Cervical active movements in sitting Extension reproduces pain in the neck and left arm at 30°. Movement occurs mainly in the upper and mid-cervical regions. Very little movement in the lower cervical or upper thoracic areas Right rotation produces a stretching in the left cervical region at 75° Left rotation reproduces left neck and interscapular pain at 40° Palpation Increased tone and tenderness noted in the left paraspinal muscles (cervical and upper thoracic) and left scalene muscles Local pain and left arm pain reproduced by postero-anterior (PA) pressures over the spinous processes of C6 and C7 and over the C6 and C7 articular pillars on the left Generalized stiffness noted with PA pressures in the mid and upper thoracic regions Segmental neurological examination Absent left triceps jerk Weakness in left triceps (25% of right side) Decreased sensation to light touch over the tip of the left middle finger Questions 1. What is the most likely source of the patient’s arm pain? 2. What is the most likely source of the patient’s neck and interscapular pain? 3. What are other possible symptoms sources? 4. Are there reasons to be cautious in administering physiotherapy treatment? 5. What would an appropriate initial physiotherapy treatment involve? 6. What would a longer-term management programme include? 7. What is the likely prognosis? 8. Is referral to other health professionals warranted? CASE STUDY 4 Neck pain – case two Subjective examination Subject 23-year-old female personal assistant HPC Rear end motor car accident 2/7 ago Immediate onset of cervical pain and stiffness (left and right). Both pain and stiffness have been increasing. Pain is now constant Vague headache started today (see Figure 8.3 ) FIGURE 8.3 Body chart – Case Study 4 . Seen by doctor yesterday who organised an X-ray (no abnormality detected) and referred patient to physiotherapy PMH Left knee reconstruction 3 years ago with good return of function since No past history of neck complaints Aggravating factors Turning head to either side, especially if movement is quick Travelling in car – took 20 minutes to settle after 30-minute car trip Easing factors Supine with head supported on one pillow Felt a bit easier under hot shower Night Wakes often due to discomfort Sleeps on 3 pillows Difficulty turning in bed due to pain Daily pattern Constant pain that gradually worsens during the day General health Taking non-prescription analgesics every 4 hours on advice of doctor. No other medications Not seeing the doctor for any other health problems Attitude/expectations Anxious about prognosis Worried about how much work she will have to miss as she only started in her current position 3/12 ago Pain and dysfunction scores VAS current pain at rest = 5 VAS level of pain after 30 minute car trip = 8.5 Physical examination Observation Walking slowly and all movements are guarded Removes jacket slowly and with great care Neck in slight protracted posture Palpation Generalized tenderness to light palpation of cervical spine (central, left and right) Increased muscle spasm left and right paraspinal muscles Further detailed palpation not possible because therapist wary of exacerbating symptoms Active movements Left rotation equals 30° before pain started increasing Right rotation equals 35° before pain started increasing Attempt to retract cervical spine caused increased pain No other movements tested today Questions 1. What is your provisional diagnosis? 2. Which of the signs and symptoms will you place on your priority list? 3. How will you address these in your treatment plan? 4. What kind of common and less common problems need to be excluded? 5. How relevant are work details for this patient? 6. How will the expectations of the patient influence your treatment? 7. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 5 Thoracic pain Subjective examination Subject 60-year-old male lawyer Presents with bilateral lower thoracic pain with radiation of symptoms anteriorly to the lower sternal area (see Figure 8.4 ) FIGURE 8.4 Body chart – Case Study 5 . Had a similar problem 5 years previously that settled with physiotherapy which resolved after three sessions of passive mobilisation directed to the thoracic spine HPC Noticed onset of symptoms 4/52 previously after lifting pots while gardening. Pain initially felt in sternal area, then onset of thoracic pain over the course of the day Pain initially intermittent, now constant at a level of VAS 2/10 at best and VAS 7/10 at worst Medical history Noticed 5 kg of weight loss in previous 4/52 that could not be explained by other factors Had noticed intermittent, generalised, mild (VAS 1–2/10), aches and pains in trunk, arms and legs over the previous 3/12 that had worsened slightly over the previous 4/52 Aggravating factors Prolonged sitting for greater than 20 minutes at work would increase posterior and anterior chest pains to VAS 6/10 Easing factors Standing and walking for 10 minutes decreases all symptoms to VAS 2/10 Night Wakes 3–4 times each night with increased symptoms in thoracic and sternal areas. Has to get out of bed and walk around to ease pain. Tends to notice generalised aches and pains associated with increased sweating at night Daily pattern Dependent on amount of sitting during the day. More thoracic and sternal pain at end of day when sitting a lot Medication Nil Attitude/expectations Expects that physiotherapy will ease symptoms as they did for a past episode of similar pain Physical examination Observation Increased thoracic kyphosis noted while sitting. Able to actively correct sitting posture, although this increases thoracic pain slightly Thoracic active movements in sitting Extension is restricted by about 50% and reproduces posterior thoracic pain with overpressures localised to the mid/lower thoracic spine Thoracic rotation feels stiff but no pain reproduced Flexion is normal in range and reproduces a stretching feeling in the mid thoracic area Palpation Generalised stiffness noted on midline and unilateral postero-anterior (PA) pressures from T2–T10 Posterior thoracic and anterior pain reproduced with midline PA pressures over T7–T8. These pains settled quickly once the pressure was released Palpation of the ribs, inferior part of the sternum and upper part of rectus abdominis did not reveal any increased tenderness Questions 1. What are your hypotheses regarding the likely source of the thoracic and sternal pains? 2. What would an appropriate initial physiotherapy treatment involve? 3. Are there examination findings that would make you suspect a non-musculoskeletal source of the symptoms? 4. What are red flags? 5. Is referral to other health professionals warranted? CASE STUDY 6 Low back pain – case one Subjective examination Subject 44-year-old male bank manager HPC 4/7 ago bent to reach into boot of car and felt slight backache. Thought it would settle so played golf anyway. Next morning severe low back pain with aching pain radiating down the back of the right leg to just below the knee. Has no pins and needles or numbness (see Figure 8.5 ) FIGURE 8.5 Body chart – Case Study 6 . PMH Has had four or five episodes of low back pain over the last 8 years, usually settles quickly in 2 or 3 days Has not required treatment with previous episodes Aggravating factors Finds it difficult to put shoes and socks on in the morning After driving to work (about 40 minutes) found leg pain had worsened Can only sit for about 15 to 20 minutes at a time at work Has noticed that sneezing increased back and leg pain Easing factors Lying on back eventually relieves the leg pain Standing and walking seem to help a little Night Pain gradually eases after initial discomfort Is waking at night but finds can get back to sleep quite quickly when changes position Daily pattern Back stiff and aches getting out of bed first thing in the morning but eases after shower Back pain is worse by the end of the day, and leg pain is more constant by the end of the day General health Taking non-steroidal anti-inflammatories (NSAIDs) with slight improvement At recent annual review doctor advised to increase physical activity to reduce weight (BMI 26.4) and adjust diet (cholesterol 6.4). Otherwise fit and well Attitude/expectations Very keen not to miss club Stableford golf competition this weekend (in 3/7) Intending to cope with work as best he can. Very busy at work so reluctant to take time off Pain and dysfunction scores Oswestry Disability Score: 36% Disability VAS level of pain after 40 minute car trip: back = 8, leg = 6 Physical examination Observation Slight left-sided contralateral list (when observed from behind in standing shoulders are to the left relative to the hips) Changes position regularly when in sitting position Palpation Increased tone, right erector spinae in the lumbar region Central postero-anterior pressures over the lumbar spine reproduced back pain (but not leg pain) at L4 and L5 Unilateral pressures were painful on the right at L4 and L5 Movements Active movements Lumbar flexion in standing limited (2 cm below the knee) Lumbar extension in standing markedly limited Left and right rotation (assessed in sitting) both more than 60° Attempt to correct contralateral list led to increased back pain Repeated active movements Flexion in standing repeated 10 times led to increased back pain and increase of leg pain Extension in standing repeated 15 times abolished leg pain, and increased range – back pain remained Repeated correction of contralateral list (side gliding to the right) led to reduced central back pain and slightly increased range Neurodynamic tests Straight leg raise: right = 70° left = 70° Slump test not evaluated Neurological tests (tests of nerve conduction) Muscle strength in myotomes L3 to S1, left = right Sensation in dermatomes L2 to S1, left = right Reflexes (patella tendon and Achilles), brisk left = right Questions 1. What is your provisional diagnosis? 2. What is the likely source of the right leg pain? 3. Which of the signs and symptoms will you place on your priority list? 4. How will you address these in your treatment plan? 5. What kind of common and less common problems need to be excluded? 6. How relevant are work details for this patient? 7. How will the expectations of the patient influence your treatment? 8. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 7 Low back pain – case two Subjective examination Subject 49-year-female assembly worker at automotive manufacturer HPC Complaining of increasing back pain over the last 14/12. Back pain is in the central low back region and radiates into both gluteal regions – no leg pain (see Figure 8.6 ). Has been off work for the last 6/12 with no improvement in pain FIGURE 8.6 Body chart – Case Study 7 . Injured back when installing car upholstery 14/12 ago. Initially had 3/7 off work and experienced some slow improvement over the first 3/12 Has had manipulative physiotherapy involving manipulation, mobilisation and traction with no benefit. Also tried chiropractic without benefit PMH 15-year history of intermittent low back pain usually no more than a few days off work Cholecystectomy 6 years ago Aggravating factors Prolonged walking or standing (more than 15 minutes) increases ache Prolonged sitting (more than 15 minutes) increases ache Unable to do weekly shopping or housework as these activities aggravate the ache Easing factors Lying down but only for about 30 minutes, as gets stiff when lying in one position for too long Night Finds it difficult to get comfortable, wakes when turning Not getting good-quality sleep any more Daily pattern Gradually worse by the end of the day General health Has gained weight over the last 14/12 (about 6 kg) Assessed as being depressed, has been taking antidepressants over the last 3/12 Investigations X-ray shows mild bilateral degeneration of the L4–5 facets CT scan shows a minor disc bulge at L4–5 and L5–S1 with no nerve root involvement Attitude/expectations Has reduced activity level to avoid aggravating back Believes that if she can find the right practitioner then they will fix her Very concerned with the CT scan report and the diagnosis of disc pathology Has been more short-tempered with family and friends since her back problem began Her spouse has been very supportive and has willingly taken over tasks such as housework and shopping Pain and dysfunction scores Oswestry Disability Score: 72% Disability VAS level of pain after 15 minutes of standing or sitting = 7.5 Physical examination Observation Exhibits pain behaviours including grimacing, and placing hand on back Changes position regularly when sitting and standing Walking pattern is slow and guarded Palpation Central palpation of the lumbar spine at L1, L2, L3, L4 and L5 painful Unilateral pressures are painful left and right at L1, L2, L3, L4 and L5 Movements Active movements Lumbar flexion in standing limited (2 cm above the knee) Lumbar extension in standing moderately limited (estimated half of expected range) Left and right rotation (assessed in sitting) both about 40° Neural mobility tests Straight leg raise on right = 50° left = 50° Able to fully extend knee in upright sitting Slump test not evaluated Neurological tests (tests of nerve conduction) • Normal no abnormality detected Questions 1. What is your provisional diagnosis? 2. How do you interpret the X-ray and CT scan reports? 3. Which of the signs and symptoms will you place on your priority list? 4. How will you address these in your treatment plan? 5. What kind of common and less common problems need to be excluded? 6. How relevant are work details for this patient? 7. What are yellow flags and how are they relevant for this patient? 8. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 8 Shoulder pain Subjective examination Subject 47-year-old female factory worker Right arm dominant HPC Right shoulder pain which started 1/52 ago when dragging a heavy item onto the conveyor belt. Routinely she has to pull, lift, and reach overhead PMH Low back pain episodes since work-related lifting injury Asthma and frequent coughing Aggravating factors At work: Overhead work, lifting and carrying boxes In transit: Driving car, riding a bike with wide handlebars. At home: Preparing meals, working at the computer, knitting Easing factors Rest Avoiding overhead work or holding elbows out when lifting or carrying items Night Wakes frequently because of pain, particularly when sleeping on the painful shoulder Daily pattern Constant nagging pain that worsens during activities as mentioned above (see aggravating factors ) General health Asthma attacks. Smokes. Using bronchodilatators as needed Attitude/expectations Is afraid that she may need to look for another job due to experiencing increasing shoulder problems at work Wants better duties within the factory as some of her colleagues have managed to do Pain and dysfunction scores VAS current pain at rest = 3 VAS usual level of pain during aggravating activity in the last week = 7 VAS worst level of pain in the last week = 9 Shoulder Pain and Disability Index (SPADI): Pain score = 60%, Disability score = 45%, Total score = 50.8% ( Roach et al 1991 ) Objective examination Standing with arms relaxed Shoulders protracted and depressed (right > left) Right shoulder abducted and elbow flexed Hyper kyphosis Shortness of breath with upper chest breathing Palpation Skin temperature (T sk ) normal Tenderness of subscapularis, supraspinatus and serratus posterior superior with palpable trigger points Painful insertion of subscapularis and supraspinatus on the humerus Palpable click on shoulder abduction Muscle length and strength Tightness of the subscapularis, pectoralis minor Weakness of rhomboids, supraspinatus Functional and other testing, including ROM Painful arc when abducting arm (90–115° abduction) with audible click (VAS rises to 6 during this impingement) Hawkins and Kennedy impingement test (compressing the subacromial tissues by internal rotation in 90° shoulder flexion) was positive ( Ginn 2003 ) and VAS rises to 8 Apprehension test for shoulder stability and SLAP lesion tests were negative, indicating integrity of joint capsule, labrum and ligaments ( Brukner et al 2001e , Ginn 2003 , Hoppenfield 1986 ) Shoulder elevation reduced by 10° with early scapular movement when comparing with left shoulder (VAS rises to 5) Pain on resistance against external rotation and abduction (VAS rises to 8) Reduced internal rotation and adduction strength when pushing palm of the hand on the table when sitting at the table (VAS rises to 7) Difficulty placing right hand behind back. Positive Gerbers’ test (resisting against hand when patient is pushing hand away from the spine (VAS rises to 8) Questions 1. What is your provisional diagnosis? 2. What signs and symptoms lead you to this diagnosis? 3. Describe the mechanism that can leads to this condition. 4. How will you address these signs and symptoms in your treatment plan? 5. What kind of common and less common problems need to be excluded? 6. Can patient’s asthma and hyper kyphosis contribute to the shoulder complaint? 7. How will the expectation of the patient influence your treatment? 8. Is it possible that outcome measures do not reflect the severity of pain and disability experienced by the patient? 9. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 9 Elbow pain Subjective examination Subject 39-year-old male carpenter Right hand dominant HPC Right lateral elbow pain off and on for at least 5/12. Insidious onset Worsened 4/52 ago when his nail gun broke down and he was forced to use a hammer all day Severe pain and reduced strength, particularly when using his arm during activities such as gripping, holding and lifting. Pain radiates into forearm No history of locking PMH Fractured ribs 3 years ago due to fall at work. Landed on his right side, and elbow was pushed into the ribs. No elbow symptoms until 5/12 ago Never experienced any symptoms of the cervical or thoracic spine Minor injuries such as an ankle sprain, mainly due to sport Aggravating factors Firm gripping (e.g. pliers) Hammering Screw driving Using a jackhammer Driving (car has no power steering) Closing a tap Knocking the elbow Easing factors Rest Ice Night Constant ache. Lying on elbow or pulling up the blanket makes it worse Daily pattern Constant pain that worsens during and directly after activity General health No other health problems reported. Not using any medication or receiving any other medical care Attitude/expectations Is disappointed that his elbow problem hasn’t improved over time as his other injuries did Experiencing increasing problems at work. Is afraid that he will lose his job One of his colleagues experienced major improvement after physiotherapy treatment and he hopes that it will help him too Expects that it may take some time since he wants to stay at work Pain and dysfunction scores VAS current pain at rest = 4 VAS usual level of pain during activity in the last week = 8 VAS worst level of pain in the last week = 9–10 Upper Extremity Functional Index (UEFI) 35/80 ( Stanford et al 2001 ) Objective examination Arm at rest while standing Elbow flexed (right > left) Wrist flexed (right > left) Forearm supinated (right > left) Palpation Skin temperature (T sk ) normal Lateral epicondyle extremely painful with some palpable swelling Tenderness extensor carpi radialis brevis and longus Thickening in extensor carpi radialis brevis (ECRB) Difficult to palpate for tenderness of capitellum radii due to surrounding tissue swelling and pain Muscle length ECRB – tight (flexion and ulnar deviation of the wrist, pronation of the forearm, and slight extension of elbow) Extensor carpi radialis longus – tight (flexion and ulnar deviation of the wrist, pronation of the forearm, and complete extension of elbow) Functional testing, including ROM and strength Elbow extension showed pain in at end of ROM (VAS rises to 6) Forearm pronation/supination showed full ROM (VAS rises to 5) Reduced grip strength (VAS rises from 4 to 9 during firm gripping) Difficulty opening pushing door handle and opening door (VAS rises to 7) Difficulty lifting an object with palm of hand facing down (VAS rises to 8) Resistance against dorsiflexion in a dorsiflexed position of the wrist, with fist closed, caused severe pain on the lateral side of the elbow Questions 1. What is your provisional diagnosis? 2. What signs and symptoms lead you to this diagnosis? 3. Describe the mechanism that can lead to the condition 4. What will you include in your treatment plan? 5. What kind of common and less common problems need to be excluded? 6. How likely does the patient’s previous fall contribute to the current complaint? 7. How will the expectations of the patient influence your treatment? 8. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 10 Hand weakness and pain Subjective examination Subject 56-year-old woman who works part-time as a kindergarten assistant Right hand dominant HPC Pain, numbness and tingling noticed in right hand (particularly in the thumb, index and middle fingers) over the last 6/52, especially at night. Insidious onset Has started to have difficulty using right hand for gripping and it is starting to affect work as a kindergarten assistant and tennis Feels it is getting worse, because pain is now extending up the forearm. Is now waking her during the night PMH Diagnosed with non-insulin-dependent diabetes 5 years ago, currently well controlled with diet and exercise (walks for 45 minutes three times a week and plays social tennis twice a week) Knee arthroscopy with partial left medial menisectomy 12 years ago after tennis injury, recovered well Aggravating factors Gripping (tennis racquet after 1 set, a feeling of weakness) Opening jars Packing up play equipment at kindergarten Sleeping Easing factors Gets a little relief from changing position and shaking out wrist Aspirin (started aspirin 2/52 ago on advice of GP), may have helped a little Night Now waking every night (once only) with right wrist pain and numbness Daily pattern Symptoms are dependent on activity. Finds it is painful at end of shift at the kindergarten and after tennis. Otherwise not troubling too much during the day Attitude/expectations Enjoys her regular exercise (especially tennis) so is keen to get the problem fixed She has friends who had surgery for something that sounded similar so is not sure why she was referred to physiotherapy or how it might help Pain and dysfunction scores VAS current pain at rest = 1.5 VAS worst level of pain in the last week = 7 Levine symptom severity scale = 1.9/5.0 Levine functional status scale = 1.4/5.0 Physical examination Observation No abnormality detected No wasting of right thenar eminence Palpation Slight reduction to light touch on the palmar surface of the right thumb and 1st and 2nd finger Movement (right side) Wrist flexion = 60°, no pain Wrist extension = 55°, no pain Wrist supination = 90° from mid-prone, no pain Wrist pronation = 90° from mid-prone, no pain Finger IP flexion OK, no pain Finger MCP flexion OK, no pain Thumb flexion, abduction and opposition OK, no pain Functional testing, including ROM and strength Grip strength assessed on Jamar dynamometer (right = 27 kg with VAS = 3, left = 35 kg) Phalen’s test (sustained bilateral wrist flexion) reproduced numbness on palmar surface of index and middle after 45 seconds Upper limb tension test with a median nerve bias: reproduced right hand symptoms which eased on release of shoulder depression ( Butler 2000 ) Questions 1. What is your provisional diagnosis? 2. What are the anatomical relationships that explain your provisional diagnosis and the patient’s symptoms and signs? 3. Explain the significance of the night symptoms and the positive Phalen’s sign. 4. Are there other assessment techniques that could be used to confirm the provisional diagnosis? 5. Find out what items the Levine symptom severity and functional status scales assesses ( Levine et al 1993 ) and then discuss how this patient rates. 6. Which of the symptoms and signs will you place on your priority list? 7. How will you address these in your physiotherapy treatment plan? 8. Are there other problems that could be contributing to the symptoms? 9. The patient has some friends who had surgery for something similar. What is the role of surgery for this condition? CASE STUDY 11 Groin pain Subjective examination Subject 17-year-old male student Playing in high-level senior soccer team with training three times a week in addition to a match on the weekend Plays as midfielder Right foot dominant HPC About 4/12 ago noticed slight stiffness in groin the morning after a strenuous match. Insidious onset Gradually got worse until about 2/12 ago could not train or play without right-sided groin pain. Performance was also waning with a loss of power and acceleration On advice of team trainer rested from all training and playing for 6/52, but on resumption of training 2/52 ago groin pain returned immediately. Seen by GP who ordered X-rays and a bone scan, and referred him to physiotherapy PMH Well-controlled asthma. Uses one puff of a preventer daily (Flixitide). Rarely needs to use reliever (Ventolin) Episode of Osgood–Schlatters syndrome when 14 years old after joining soccer development squad. Resolved after 1 year through modification of activity Otherwise well and not seeing the doctor for any other condition Aggravating factors Running, especially when sprinting and when cutting (changing direction) Kicking, especially when taking a corner No pain on sneezing or coughing Easing factors Avoidance of aggravating activities Night Sleep unaffected Daily pattern Symptoms are dependent on activity. Now affecting whenever tries to run or kick a ball Notices in morning, takes 10 to 15 minutes to ease Attitude/expectations Concerned that the problem appears to be getting worse. Had thought it would just go away Receives payment for playing in soccer team which he had planned to continue to help support his studies at university Pain and dysfunction scores VAS current pain at rest = 0 VAS worst level of pain in the last week = 9 (kicking across from a corner) VAS worst level of pain in the last week = 8 (when attempting to sprint) Physical examination Observation In standing, no obvious wasting or pelvic asymmetry With walking, observed excessive pelvic tilting (obliquity) in the frontal plane Palpation Tender to palpation at tendon attaching to right medial inferior pubic ramus Trigger point tenderness to muscle belly distal to medial inferior pubic ramus Tender at right side of pubic symphysis Movement Right hip flexion = 130°, no pain = left Right hip extension = 25°, no pain = left Right hip abduction = 45°, pain (VAS = 3), left = 55° Right hip internal/external rotation = left Functional testing Squeeze test (patient supine with hip flexed 45°, examiner places fist between patient knees, and asks patient to bilaterally adduct) reproduced right groin pain (VAS = 4) Resisted straight-leg right hip adduction reproduced right groin pain (VAS = 4) Right hip quadrant (passive hip flexion, adduction and internal rotation) only very slight pain, similar to discomfort when tested on the left side Thomas test (slight restriction on right compared to left with only slight reproduction of pain (VAS = 0.5) when hip flexion resisted) Abdominal muscle testing: 1. global muscles, only slight pain (VAS = 1) on resisted abdominal flexion 2. stabilising muscles, assessed in supine with a pressure cuff biofeedback unit placed in the small of the back. He could increase the pressure in the cuff from 40 to 43 mmHg for 3 seconds 4 times before unwanted activity from global muscles was observed Standing on one leg (Trendelenburg test), only slight drop of pelvis observed, within normal limits (<10°) Investigations (completed 1/52 ago) X-ray: no abnormality detected Bone scan: indicated some increased uptake in the right inferior pubic region Questions 1. What is your provisional diagnosis? 2. What are the key findings from your examination that led to your provisional diagnosis? 3. What other common causes of groin pain did you consider in making your diagnosis? 4. What are some less common causes of groin pain that you need to consider when examining this patient? Briefly explain why these are considered unlikely at this stage. 5. What is Osgood–Schlatter’s disease and what is its relevance to the current condition? 6. What are the significance of the bone scan findings and the assessment of the abdominal stabilising muscles, and do these findings tie in with the other assessment findings? 7. Which of the symptoms and signs will you place on your priority list? 8. How will you address these in your physiotherapy treatment plan? CASE STUDY 12 Hip and thigh pain Subjective examination Subject 38-year-old female Right leg dominant HPC Right lateral hip and thigh pain that can radiate to knee Started approximately 1/12 ago Woke up with pain after a long shopping day PMH Overweight (BMI ≥27) Neck pain and headaches Aggravating factors Walking Sleeping on right side Sleeping on a hard mattress Easing factors Rest and ice Night Wakes up frequently, particularly when lying on right side, or on left side with right hip in adduction and knee resting on the mattress Daily pattern Pain during and after prolonged standing and walking General health Overweight. No other problems reported. Not using any medication Attitude/expectations Is not sure whether treatment will provide immediate relief, but hopes that at least she will be able to sleep better. Between pain experienced at night and her youngest child waking up and demanding attention she does not get much sleep and feels fatigued Pain and dysfunction scores VAS current pain at rest before activity = 2 VAS usual level of pain when waking up at night = 8 VAS usual level of pain during and after activity in the last week = 7 VAS worst level of pain in the last week = 9 Lower Extremity Functional Scale 48/80 ( Binkley et al 1999 ) Objective examination Standing Visibly overweight Wide hips, but knees are touching each other Valgus position of knees and ankles Pronated feet with reasonable longitudinal arches Palpation Although skin temperature (T sk ) around hip and along the thigh appeared normal, that of the posterior aspect of the trochanter may have been a little elevated Tenderness of the iliotibial tract and the bony posterior aspect of the greater trochanter, with a boggy feeling around the location of the bursa ( Hoppenfield 1986 )
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:

Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

Pharmacy guide to joint pain: case studies

Science Photo Library
This is the third and final article in this series, designed to help pharmacy teams support patients who are experiencing joint pain or patients who have been diagnosed with osteoarthritis (OA) and may benefit from recommendations for appropriate management strategies, including the wide range of products available in pharmacies.
Read more about our joint pain partnership and find related content on our Pharmacy Learning Centre.
By using available opportunities, such as when patients collect prescribed medicines or when patients purchase an over-the-counter (OTC) product, pharmacy teams can provide patients with additional advice and guidance, including signposting them to resources, charities and organisations that can provide additional support.
In the ‘ Pharmacy guide to joint pain: diagnosis and assessment ‘ and ‘ Pharmacy guide to joint pain: management ‘, best practice for pharmacy teams was outlined for patients who present in community pharmacy with new onset joint pain . In this article, case studies provide further context for the appropriate diagnosis and management of patients.
Case study 1: Assessing a patient with ‘red flag’ symptoms
- Prior reading: ‘ Pharmacy guide to joint pain: diagnosis and assessment ‘
An overweight man in his 50s, who is not a regular customer at the pharmacy, approaches the counter and speaks to a member of the pharmacy team.
Pharmacy technician: Hello, is there anything I can help you with today? Patient: Hi there, my wrist has been sore, and I was wondering if you could recommend something for pain relief? Pharmacy technician: I’m sorry to hear that. Would you like to come into the consultation room so that we can discuss this further? Patient: OK. Pharmacy technician: Have you had any recent falls or injuries that may have caused the pain? Patient: No, not at all. It just seems to have developed. It seems to be bothering me as I try to pick up and grip objects. Pharmacy technician: Does your wrist feel stiff in the mornings? Patient: Yes, it does. The stiffness seems to last about 15–20 minutes and then seems to ease up a bit. It can feel a bit stiff too if I’ve not used it for too long. This has been ongoing for a few months now so thought I should come and speak to someone about it. Pharmacy technician: Have you experienced any other symptoms, such as hot swollen joints, fever or weight loss? Patient: (Patient shows you their wrist and it looks a little red and is hot to the touch) . I haven’t really noticed any other symptoms, just the pain and stiffness , but it is a little red now. Pharmacy technician: Do you have any other health problems or are you taking any other medication? Patient: Yes, I have had a previous cancer diagnosis but I am currently in remission. Pharmacy technician: As you have told me that you have had a previous condition and that today your wrist appears a little red and swollen, I think it would be worth a visit to the nearest NHS walk-in centre to get this looked at. Here is a list of the nearest centres to us. Patient: Thank you. I shall go there now.
Case study 2: Symptoms of mechanical joint pain
A woman aged 48 years, a regular customer in the pharmacy, approaches the counter and speaks to the pharmacy technician.
Pharmacy technician: Hello Ms Spence, is there anything I can help you with today? Patient: Hello, I wanted to ask your advice. I’ve noticed my knee is a bit sore, especially when walking up the stairs or when I’m doing chores around the house. Pharmacy technician: I’m sorry to hear that, have you ever had any trouble with your knee before? Patient: Actually, yes, now you mention it. When I was younger, I tore a ligament in the same knee and had an operation, but it’s been fine for years. Pharmacy technician: What is the pain like? Patient: It’s a grating pain and I’ve noticed it’s definitely worse when I’m moving around a lot more. Pharmacy technician: Does your knee ever feel stiff? Patient: Well yes, in the morning it’s a bit stiff when I get out of bed, but that usually eases off really quickly once I start moving around. Pharmacy technician: It sounds to me like you may have some symptoms that are indicative of osteoarthritis (OA). This may seem concerning, but it can be managed through the pharmacy, let me explain further. Your knee and other joints are sites of continual growth, degeneration and repair. In most cases, the body is able to repair the damage itself and no symptoms are experienced. OA arises as a result of the failure of normal replacement and regrowth in the joints. Do you want to come into the consultation room so I can ask you a few more questions? Then we can get to the bottom of this and look into possible management options?
Case study 3: Providing advice for the management of mechanical joint pain symptoms
- Prior reading: ‘ Pharmacy guide to joint pain: management ‘
A woman aged 64 years comes into the pharmacy to pick up her husband’s medication. When trying to open her bag, she tells the pharmacy technician she has been having some trouble with her hands.
Patient: My hands have been getting very uncomfortable over the past few months, mainly this thumb and the ends of these fingers, carrying the shopping and this lot is so difficult. Could you recommend anything? After asking about red flag symptoms, you decide the woman is likely to have typical hand osteoarthritis (OA), with no red flag symptoms. Pharmacy technician: It sounds to me as if you may have some symptoms that are indicative of OA. This may sound concerning but it can be managed, let me explain further. Your knee and other joints are sites of continual growth, degeneration and repair. In most cases, the body is able to repair the damage itself and no symptoms are experienced. OA arises as a result of the failure of normal replacement and regrowth in the joints. I can recommend some exercises for you that may help ease the pain and improve your symptoms. Patient: That sounds good, are they difficult? How will I remember them? Is there anything you can give me for the pain too? Pharmacy technician: Don’t worry, they are very simple, and should only take 5–10 minutes each day. I can give you a leaflet called ‘Keep moving’ , which has all the exercises outlined in case you forget. Do you have any other health problems or are you taking any other medication? Have you tried anything to relieve the pain? Patient: No, I don’t take anything at the minute and haven’t tried anything for the pain. I’ve tried using an ice pack but it’s useless. Pharmacy technician: OK, well in that case I would recommend that you try a topical gel for pain relief. If you use this in combination with the exercises I have shown you, you should hopefully see some improvements. You could also try using a heat pack when your hands are feeling sore if you haven’t had any luck with the ice pack.
Case study 4: Providing advice on the application of topical creams
Mr Wilson approaches the medicine counter in the pharmacy and tells you that his wife had been advised to use ibuprofen gel on her knee as she had symptoms indicative of osteoarthritis (OA).
Mr Wilson: Hello, I just wanted to get some advice on this gel that my wife has been recommended. She used this a few years ago when she was diagnosed with OA. She is having a bit of a flare up of symptoms at the minute and this gel worked well before. She hasn’t used it in a few years and I just wanted to check she is using it properly as she has used it for two days but hasn’t had any pain relief yet. Pharmacy technician: Hi Mr Wilson, if your wife has previously been diagnosed with OA and has used this gel before and it’s been effective, it’s definitely the best thing to try first. These gels can take up to two weeks before they give their maximum effect. The gel should be applied regularly as explained in the leaflet. If she doesn’t notice any effect after two weeks she could then try an alternative treatment. Mr Wilson: Oh right OK, I didn’t realise that. Oh yes, it said to apply a small amount of the gel up to four times daily, so I’ll make sure she does that too. Pharmacy technician: Has your wife been given any advice on exercises she could do with her knee as well as using the gel? If she was given any before I would definitely recommend she starts doing these again and this should also help ease the pain and improve movement. I can also give you some leaflets for her with some simple exercises she could start doing at home. Using an ice or heat pack can also help with pain relief. Mr Wilson: Yes, now you mention it she did have some exercises given to her before, so I’ll hunt these out when I get home, I’m sure I put them in the drawer. If you had a leaflet too that would be great, and I’ll mention to her about the ice or heat pack too, thank you.
*All case studies are fictional.
Please leave a comment Cancel reply
You must be logged in to post a comment.
You might also be interested in…

NICE recommends exercise over analgesics for patients with osteoarthritis

Help us fight joint pain in community pharmacy — become a ‘PJ joint pain champion’

Opioid prescribing for patients waiting for hip and knee surgery increased by 40% during pandemic
Error: User registration is currently not allowed.
Username or Email Address
Google Authenticator code
Remember Me
Lost your password?
← Go to BMJ
Lablogatory
A blog for medical laboratory professionals

Microbiology Case Study: A 27 Year Old with Disseminated Joint Pain
Case History
A 27 year old male presented to the Emergency Department (ED) with complaints of right knee pain and swelling for one week. Two weeks prior, he tripped while walking to work and began to feel pain in his right calf. Upon physical examination, swelling was noted in his ankles, knee, shoulders, and fingers. The knee and shoulder were tender to palpation. In the ED, he was afebrile and vitals were normal. He denied any sort of injury, chills, or rash and no history of tobacco, alcohol, or illicit substance abuse. CT scan of the lower extremity showed no acute fracture but moderate to large knee joint effusion was observed. He and his fiancé (male partner) has been in a monogamous relationship for almost a decade, however the patient did have a history of gonorrhea nine years ago but was treated. Knee arthrocentesis was performed. The fluid was yellow and cloudy and contained 27,000 WBCs. The Gram stain of the synovial fluid showed many intracellular gram negative diplococci and the joint fluid culture grew out Neisseria gonorrhoeae . PCR of the rectal swab also detected N. gonorrhoeae .
N. gonorrhoeae is the causative agent of gonorrhea, a sexually transmitted disease. In the United States, it is the second most commonly reported communicable disease. 1 While infections can be asymptomatic, in men, gonorrhea commonly causes acute urethritis with dysuria, urethral discharge, and rarely, epididymitis. 2,3,4 In women, gonorrhea can cause cervicitis and lead to pelvic inflammatory disease (PID), infertility, ectopic pregnancy, and chronic pelvic pain. 5,6 Those with gonococcal endocervicitis can be co-infected with Chlamydia trachomatis and/or Trichomonas vaginalis , other causative agents of sexually transmitted diseases. N. gonorrhoeae can cause extragenital infections in the pharynx and rectum, which are most commonly seen among men who have sex with men (MSM). Disseminated gonococcal infection is rare (0.5-3% of infected individuals) and can be characterized by low grade fever, hemorrhagic skin lesions, tenosynovitis, polyarthralgia and septic arthritis. Complications of disseminated infections may include permanent joint damage, endocarditis, and meningitis. Gonococcal conjunctivitis mainly affects newborns from untreated mothers. 7
Gonorrhea can be diagnosed clinically by a history and physical examination and also, by microbiological methods. Home collection kits are available to increase convenience. On a Gram stain, N. gonorrhoeae , a gram negative coccus, frequently appears within or closely associated polymorphonuclear leukocytes (PMNs) typically as diplococci pairs. Direct smears can be prepared from urethral, endocervical sites, and normally sterile or minimally contaminated sites such as joint fluid. Swab specimens (e.g. urogenital, pharyngeal, vaginal or rectal) should be collected with a Dacron or Rayon swab as calcium alginate and cotton swabs may be toxic or inhibitory for the bacteria. 8 Specimens must be transported to the microbiology immediately. 9 Blood and joint fluid are also acceptable specimen types for culture for detection of disseminated gonococcal infection.
Enriched selective media for culture of N. gonorrhoeae includes MTM medium, ML medium, GC-Lect and the New York City medium. Plates should be incubated in a CO 2 incubator (between 3-7%) at 35C to 37C for optimal growth. 9 Gram negative diplococci recovered from urogenital sites that grow on the selective media and are oxidase-positive can be presumptively identified as N. gonorrhoeae . Another quick biochemical test that can be done is superoxol; N. gonorrhoeae produce immediate bubbling whereas N. meningitidis and N. lactamica produce weak, delayed bubbling. Confirmation using other testing methods such as carbohydrate utilization tests (e.g. N. gonorrhoeae produces acid from glucose only), immunological methods, enzymatic procedures, or DNA probe are also available. 10
Compared to standard culture methods, Nucleic Acid Amplification Tests (NAAT) offer more rapid results and increased sensitivity. Additionally, NAATs may also include additional targets such as C. trachomatis , a frequent co-pathogen, as part of the assay. NAATs should be used according manufacturer’s protocols and on validated specimen types. For example, the Cepheid Xpert CT/NG test (as used by our patient here) can be used to test asymptomatic and symptomatic individuals and the acceptable specimen types are urine, pharyngeal, and rectal swabs, patient-collected vaginal swabs, and clinician-collected endocervical swabs. 11 Given the legal implications of a N. gonorrhoeae diagnosis in a child, the CDC recommends that NAATs can be used to test for N. gonorrhoeae from vaginal and urine specimens from females and urine for males. 12 For extragenital specimens, only validated FDA-cleared NAATs assays using pediatric specimens should be used.
The CDC recommends that uncomplicated gonorrhea be treated with ceftriaxone and azithromycin. However, between 2000-2010s, elevated MICs to both ceftriaxone and cefixime were seen and emerging azithromycin resistance is still a concern. The CLSI M100 currently recommends agar dilution or disk diffusion for antimicrobial susceptibility testing for N. gonorrhoeae . Susceptible and resistant interpretative breakpoints are available for penicillin, most cephems, tetracycline, ciprofloxacin, and spectinomycin. Of note, for azithromycin, only the susceptible category has a breakpoint. 13

- CDC. Sexually Transmitted Disease Surveillance, 2020. Atlanta, GA: Department of Health and Human Services; April 2022.
- John J, Donald WH. Asymptomatic urethral gonorrhoea in men. Br J Vener Dis 1978; 54:322.
- Handsfield HH, Lipman TO, Harnisch JP, et al. Asymptomatic gonorrhea in men. Diagnosis, natural course, prevalence and significance. N Engl J Med 1974; 290:117.
- Sherrard J, Barlow D. Gonorrhoea in men: clinical and diagnostic aspects. Genitourin Med 1996; 72:422.
- McCormack WM, Johnson K, Stumacher RJ, Donner A, Rychwalski R. Clinical spectrum of gonococcal infection in women. Lancet , 1(8023), 1182–1185 (1977).
- Curran J, Rendtorff R, Chandler R, Wiser W, Robinson H. Female gonorrhea: its relation to abnormal uterine bleeding, urinary tract symptoms, and cervicitis. Obstet Gynecol , 45(2), 195–198 (1975).
- O’Brien JP, Goldenberg DL, Rice PA. Disseminated gonococcal infection: a prospective analysis of 49 patients and a review of pathophysiology and immune mechanisms. Medicine (Baltimore) 1983; 62:395.
- Laurer BA, Masters HB. Toxic effect of calcium alginate swabs on Neiserria gonorrhoeae. J Clin Microbiol 1988: 26:54-56
- Leber, A. 3.9 Genital Cultures. Clinical Microbiology Procedures Handbook, 4th Edition. ASM Press, Washington, DC. 2016. p.3.9.3.1-3.9.3.15.
- Knapp JS. Historical perspectives and identification of Neisseria and related species. Clin Microbiol Rev 1988;1:415-431.
- Cepheid GeneXpert. Xpert CT/NG (English). 2019. 301-0234 Rev.K
- CDC. Gonococcal Infections Among Infants and Children. Sexually Transmitted Infection Treatment Guidelines, Atlanta, GA: Department of Health and Human Services; 2021.
- CLSI. Performance Standards for Antimicrobial Susceptibility Test. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2022, Edition 32

-Maikel Benitez Barzaga, MD is a Pathology Resident (PGY-1) at The George Washington University Hospital. His academic interest include hematology, microbiology, molecular and surgical pathology.

-Rebecca Yee, PhD, D(ABMM), M(ASCP) CM is the Chief of Microbiology, Director of Clinical Microbiology and Molecular Microbiology Laboratory at the George Washington University Hospital. Her interests include bacteriology, antimicrobial resistance, and development of infectious disease diagnostics.
Share this:
Leave a comment cancel reply.
This site uses Akismet to reduce spam. Learn how your comment data is processed .

- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu
- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Intramuscular botulinum toxin as an adjunct to arthrocentesis with viscosupplementation in temporomandibular disorders: a proof-of-concept case–control investigation.

1. Introduction
2.1. pain at rest, 2.2. pain at chewing, 2.3. masticatory efficacy, 2.4. functional limitation, 2.5. subjective efficacy, 2.6. maximum non-assisted and assisted mouth opening, 2.7. side effects, 3. materials and methods, 3.1. ethics, 3.2. study design/sample, 3.3. participants, 3.4. variables, 4. discussion, 5. conclusions, 6. future perspective, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021 , 25 , 441–453. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nazzal, H.; Baccar, M.; Ziad, T.; Al-Musfir, T.; Al Emadi, B.; Matoug-Elwerfelli, M.; Narasimhan, S.; Khan, Y.; Reagu, S. Prevalence of anxiety, sleep bruxism and temporomandibular disorders during COVID-19 in Qatari children and adolescents: A cross-sectional study. Eur. Arch. Paediatr. Dent. 2023 , 24 , 787–795. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Colonna, A.; Guarda-Nardini, L.; Ferrari, M.; Manfredini, D. COVID-19 pandemic and the psyche, bruxism, temporomandibular disorders triangle. Cranio J. Craniomandib. Pract. 2021 , 42 , 429–434. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- De la Torre Canales, G.; Bonjardim, L.R.; Poluha, R.L.; Carvalho Soares, F.F.; Guarda-Nardini, L.; Conti, P.R.; Manfredini, D. Correlation Between Physical and Psychosocial Findings in a Population of Temporomandibular Disorder Patients. Int. J. Prosthodont. 2020 , 33 , 155–159. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zani, A.; Lobbezoo, F.; Bracci, A.; Djukic, G.; Guarda-Nardini, L.; Favero, R.; Ferrari, M.; Aarab, G.; Manfredini, D. Smartphone-based evaluation of awake bruxism behaviours in a sample of healthy young adults: Findings from two University centres. J. Oral Rehabil. 2021 , 48 , 989–995. [ Google Scholar ] [ CrossRef ]
- De la Torre Canales, G.; Manfredini, D.; Grillo, C.M.; Guarda-Nardini, L.; Machado Gonçalves, L.; Rizzatti Barbosa, C.M. Therapeutic effectiveness of a combined counseling plus stabilization appliance treatment for myofascial pain of the jaw muscles: A pilot study. Cranio J. Craniomandib. Pract. 2017 , 35 , 180–186. [ Google Scholar ] [ CrossRef ]
- Haskin, C.L.; Milam, S.B.; Cameron, I.L. Pathogenesis of degenerative joint disease in the human temporomandibular joint. Crit. Rev. Oral Biol. Med. 1995 , 6 , 248–277. [ Google Scholar ] [ CrossRef ]
- Sorrenti, N.G.; Manfredini, D.; Sornig, F.; Ferrari, M.; Colonna, A.; Val, M. Correlation between bilateral TMJ MRI findings: A systematic review of the literature. Dent. Med. Probl. 2024 , 61 , 401–406. [ Google Scholar ] [ CrossRef ]
- Val, M.; Sidoti Pinto, G.A.; Manini, L.; Gandolfo, S.; Pentenero, M. Variations of salivary concentration of cytokines and chemokines in presence of oral squamous cell carcinoma. A case-crossover longitudinal prospective study. Cytokine 2019 , 120 , 62–65. [ Google Scholar ] [ CrossRef ]
- Reda, B.; Contardo, L.; Vidoni, G.; El-Outa, A. Prevalence of Temporomandibular Disorders (TMD) in Dental Patients at a Specialized Regional Medical Center in Italy. Cureus 2024 , 16 , e60819. [ Google Scholar ] [ CrossRef ]
- Grochala, J.; Kajor, M.; Pihut, M.; Loster, J.E. A proposal for a database of sounds generated by temporomandibular joints and a tool for automateddiagnosisbasedonanRDC/TMDquestionnaire. Folia Med. Cracov. 2023 , 63 , 91–102. [ Google Scholar ] [ CrossRef ]
- Li, J.; Chen, H. Intra-articular injection of platelet-rich plasma vs hyaluronic acid as an adjunct to TMJ arthrocentesis: A systematic review and meta-analysis. J. Stomatol. Oral Maxillofac. Surg. 2023 , 125 , 101676. [ Google Scholar ] [ CrossRef ]
- Guarda-Nardini, L.; De Almeida, A.M.; Manfredini, D. Arthrocentesis of the Temporomandibular Joint: Systematic Review and Clinical Implications of Research Findings. J. Oral Facial Pain Headache 2021 , 35 , 17–29. [ Google Scholar ] [ CrossRef ]
- Turosz, N.; Chęcińska, K.; Chęciński, M.; Lubecka, K.; Bliźniak, F.; Chlubek, D.; Olszowski, T.; Sikora, M. Temporomandibular Joint Injections and Lavage: An Overview of Reviews. J. Clin. Med. 2024 , 13 , 2855. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rosati, R.; Val, M.; Manfredini, D.; Carmagnola, D.; Fortunati, C.; Guarda-Nardini, L.; Dellavia, C. Baseline masticatory muscles’ performance may predict pain relief in temporomandibular disorders. Oral Dis. 2024 . [ Google Scholar ] [ CrossRef ]
- Nitzan, D.W. The process of lubrication impairment and its involvement in temporomandibular joint disc displacement: A theoretical concept. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2001 , 59 , 36–45. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nitzan, D.W. ‘Friction and adhesive forces’–possible underlying causes for temporomandibular joint internal derangement. Cells Tissues Organs 2003 , 174 , 6–16. [ Google Scholar ] [ CrossRef ]
- Guarda-Nardini, L.; Masiero, S.; Marioni, G. Conservative treatment of temporomandibular joint osteoarthrosis: Intra-articular injection of sodium hyaluronate. J. Oral Rehabil. 2005 , 32 , 729–734. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Guarda-Nardini, L.; Tito, R.; Staffieri, A.; Beltrame, A. Treatment of patients with arthrosis of the temporomandibular joint by infiltration of sodium hyaluronate: A preliminary study. Eur. Arch. Otorhinolaryngol. 2002 , 259 , 279–284. [ Google Scholar ] [ CrossRef ]
- Guarda-Nardini, L.; Manfredini, D.; Salamone, M.; Salmaso, L.; Tonello, S.; Ferronato, G. Efficacy of botulinum toxin in treating myofascial pain in bruxers: A controlled placebo pilot study. Cranio J. Craniomandib. Pract. 2008 , 26 , 126–135. [ Google Scholar ] [ CrossRef ]
- Chen, Y.W.; Chiu, Y.W.; Chen, C.Y.; Chuang, S.K. Botulinum toxin therapy for temporomandibular joint disorders: A systematic review of randomized controlled trials. Int. J. Oral Maxillofac. Surg. 2015 , 44 , 1018–1026. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ramos-Herrada, R.M.; Arriola-Guillén, L.E.; Atoche-Socola, K.J.; Bellini-Pereira, S.A.; Castillo, A.A. Effects of botulinum toxin in patients with myofascial pain related to temporomandibular joint disorders: A systematic review. Dent. Med. Probl. 2022 , 59 , 271–280. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Delcanho, R.; Val, M.; Nardini, L.G.; Manfredini, D. Botulinum Toxin for Treating Temporomandibular Disorders: What is the Evidence? J. Oral Facial Pain Headache 2022 , 36 , 6–20. [ Google Scholar ] [ CrossRef ]
- Val, M.; Delcanho, R.; Ferrari, M.; Guarda Nardini, L.; Manfredini, D. Is Botulinum Toxin Effective in Treating Orofacial Neuropathic Pain Disorders? A Systematic Review. Toxins 2023 , 15 , 541. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Smuts, J.A.; Schultz, D.; Barnard, A. Mechanism of action of botulinum toxin type A in migraine prevention: A pilot study. Headache 2004 , 44 , 801–805. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Aoki, K.R. Review of a proposed mechanism for the antinociceptive action of botulinum toxin type A. Neurotoxicology 2005 , 26 , 785–793. [ Google Scholar ] [ CrossRef ]
- Durham, P.L.; Cady, R.; Cady, R. Regulation of calcitonin gene-related peptide secretion from trigeminal nerve cells by botulinum toxin type A: Implications for migraine therapy. Headache 2004 , 44 , 35–42, discussion 42–33. [ Google Scholar ] [ CrossRef ]
- Guarda Nardini, L.; Meneghini, M.; Guido, M.; Baciorri, F.; Manfredini, D. Histopathology of the temporomandibular joint disc: Findings in 30 samples from joints with degenerative disease. J. Oral Rehabil. 2021 , 48 , 1025–1034. [ Google Scholar ] [ CrossRef ]
- Val, M.; Ragazzo, M.; Bendini, M.; Manfredini, D.; Trojan, D.; Guarda Nardini, L. Computer-assisted surgery with custom prostheses and human amniotic membrane in a patient with bilateral class IV TMJ reankylosis: A case report. Cell Tissue Bank. 2022 , 23 , 395–400. [ Google Scholar ] [ CrossRef ]
- Câmara-Souza, M.B.; Bracci, A.; Colonna, A.; Ferrari, M.; Rodrigues Garcia, R.C.M.; Manfredini, D. Ecological Momentary Assessment of Awake Bruxism Frequency in Patients with Different Temporomandibular Disorders. J. Clin. Med. 2023 , 12 , 501. [ Google Scholar ] [ CrossRef ]
- Corrêa-Silva, M.; de Carvalho, T.M.I.; Zambon, C.E.; Peres, M.; Machado, G.G. Is there a superiority between arthrocentesis and stabilizing occlusal splint for the treatment of anterior disc displacement with reduction and intermittent block and anterior disc displacement without reduction in TMJ? Randomized clinical trial. Oral. Surg. Oral Med. Oral Pathol. Oral. Radiol. 2024 , 138 , P244–P254. [ Google Scholar ] [ CrossRef ]
- Guarda-Nardini, L.; Manfredini, D.; Ferronato, G. Arthrocentesis of the temporomandibular joint: A proposal for a single-needle technique. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008 , 106 , 483–486. [ Google Scholar ] [ CrossRef ]
- Rauso, R.; Lo Giudice, G.; Tartaro, G.; Zerbinati, N.; Nicoletti, G.F.; Fragola, R. Botulinum toxin type A injections for masticatory muscles hypertrophy: A systematic review. J. Craniomaxillofac. Surg. 2022 , 50 , 7–18. [ Google Scholar ] [ CrossRef ]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J. Oral Facial Pain Headache 2014 , 28 , 6–27. [ Google Scholar ] [ CrossRef ]
- Nitzan, D.W.; Dolwick, M.F.; Martinez, G.A. Temporomandibular joint arthrocentesis: A simplified treatment for severe, limited mouth opening. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 1991 , 49 , 1163–1167, discussion 1168–1170. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Manfredini, D.; Favero, L.; Cocilovo, F.; Monici, M.; Guarda-Nardini, L. A comparison trial between three treatment modalities for the management of myofascial pain of jaw muscles: A preliminary study. Cranio J. Craniomandib. Pract. 2018 , 36 , 327–331. [ Google Scholar ] [ CrossRef ]
- Pentenero, M.; Val, M.; Rosso, S.; Gandolfo, S. Microbiopsy a first-level diagnostic test to rule out oral dysplasia or carcinoma in general dental practice. Oral Dis. 2018 , 24 , 109–111. [ Google Scholar ] [ CrossRef ]
- Alpaslan, G.H.; Alpaslan, C. Efficacy of temporomandibular joint arthrocentesis with and without injection of sodium hyaluronate in treatment of internal derangements. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2001 , 59 , 613–618, discussion 618–619. [ Google Scholar ] [ CrossRef ]
- Grossmann, E.; Poluha, R.L. Comparative study of arthrocentesis with concentric-needle cannula with classic concentric needle: A randomized single-blind controlled clinical trial. J. Craniomaxillofac. Surg. 2024 , 52 , 850–854. [ Google Scholar ] [ CrossRef ]
- Mao, T.; Wang, W. Comparison of outcomes with intra-articular hyaluronic acid vs corticosteroids after TMJ arthrocentesis: A systematic review and meta-analysis. Quintessence Int. 2024 . [ Google Scholar ] [ CrossRef ]
- Delcanho, R.E.; Kim, Y.J.; Clark, G.T. Haemodynamic changes induced by submaximal isometric contraction in painful and non-painful human masseter using near-infra-red spectroscopy. Arch. Oral Biol. 1996 , 41 , 585–596. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kim, Y.J.; Kuboki, T.; Tsukiyama, Y.; Koyano, K.; Clark, G.T. Haemodynamic changes in human masseter and temporalis muscles induced by different levels of isometric contraction. Arch. Oral Biol. 1999 , 44 , 641–650. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- De la Torre Canales, G.; Alvarez-Pinzon, N.; Muñoz-Lora, V.R.M.; Vieira Peroni, L.; Farias Gomes, A.; Sánchez-Ayala, A.; Haiter-Neto, F.; Manfredini, D.; Rizzatti-Barbosa, C.M. Efficacy and Safety of Botulinum Toxin Type A on Persistent Myofascial Pain: A Randomized Clinical Trial. Toxins 2020 , 12 , 395. [ Google Scholar ] [ CrossRef ]
- De la Torre Canales, G.; Câmara-Souza, M.B.; Ernberg, M.; Al-Moraissi, E.A.; Grigoriadis, A.; Poluha, R.L.; Christidis, M.; Jasim, H.; Lövgren, A.; Christidis, N. Botulinum Toxin-A for the Treatment of Myogenous Temporomandibular Disorders: An Umbrella Review of Systematic Reviews. Drugs 2024 , 84 , 779–809. [ Google Scholar ] [ CrossRef ]
- Setler, P. The biochemistry of botulinum toxin type B. Neurology 2000 , 55 , S22–S28. [ Google Scholar ]
- Kharatmal, S.B.; Singh, J.N.; Sharma, S.S. Voltage-Gated Sodium Channels as Therapeutic Targets for Treatment of Painful Diabetic Neuropathy. Mini Rev. Med. Chem. 2015 , 15 , 1134–1147. [ Google Scholar ] [ CrossRef ]
- De la Torre Canales, G.; Poluha, R.L.; Bonjardim, L.R.; Ernberg, M.; Conti, P.C.R. Botulinum toxin-A effects on pain, somatosensory and psychosocial features of patients with refractory masticatory myofascial pain: A randomized double-blind clinical trial. Sci. Rep. 2024 , 14 , 4201. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Li, K.; Tan, K.; Yacovelli, A.; Bi, W.G. Effect of botulinum toxin type A on muscular temporomandibular disorder: A systematic review and meta-analysis of randomized controlled trials. J. Oral Rehabil. 2024 , 51 , 886–897. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nixdorf, D.R.; Heo, G.; Major, P.W. Randomized controlled trial of botulinum toxin A for chronic myogenous orofacial pain. Pain 2002 , 99 , 465–473. [ Google Scholar ] [ CrossRef ]
- Guarda-Nardini, L.; Stecco, A.; Stecco, C.; Masiero, S.; Manfredini, D. Myofascial pain of the jaw muscles: Comparison of short-term effectiveness of botulinum toxin injections and fascial manipulation technique. Cranio J. Craniomandib. Pract. 2012 , 30 , 95–102. [ Google Scholar ] [ CrossRef ]
- Kütük, S.G.; Özkan, Y.; Kütük, M.; Özdaş, T. Comparison of the Efficacies of Dry Needling and Botox Methods in the Treatment of Myofascial Pain Syndrome Affecting the Temporomandibular Joint. J. Craniofacial Surg. 2019 , 30 , 1556–1559. [ Google Scholar ] [ CrossRef ]
- Nykänen, L.; Manfredini, D.; Lobbezoo, F.; Kämppi, A.; Bracci, A.; Ahlberg, J. Assessment of awake bruxism by a novel bruxism screener and ecological momentary assessment among patients with masticatory muscle myalgia and healthy controls. J. Oral Rehabil. 2024 , 51 , 162–169. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Groups | Patient n° | Sex | Age | TMJ |
|---|---|---|---|---|
| Group A | 1 | F | 67 | 0 |
| Group A | 2 | M | 71 | 0 |
| Group A | 3 | M | 54 | 1 |
| Group A | 4 | F | 62 | 0 |
| Group A | 5 | F | 37 | 1 |
| Group B | 6 | F | 78 | 1 |
| Group B | 7 | F | 67 | 1 |
| Group B | 8 | M | 28 | 1 |
| Group B | 9 | F | 44 | 0 |
| Group B | 10 | F | 69 | 0 |
| Groups | Patient n° | Functional Limitation (T0) | Functional Limitation (T1) | Functional Limitation (T2) | Functional Limitation (T3) | Functional Limitation (T4) | Functional Limitation (T5) |
|---|---|---|---|---|---|---|---|
| GROUP A | Average | 3.2 | 2.8 | 2.2 | 2.2 | 0.8 | 0.2 |
| Standard Deviation | 0.45 | 0.45 | 0.45 | 0.45 | 0.45 | 0.45 | |
| GROUP B | Average | 3.6 | 3.8 | 3 | 2.8 | 1.6 | 0.4 |
| Standard Deviation | 0.55 | 0.45 | 0.71 | 0.45 | 0.55 | 0.55 |
| Groups | Patient n° | Maximum Non-Assisted Mouth Opening (T0) | Maximum Non-Assisted Mouth Opening (T5) | Maximum Assisted Mouth Opening (T0) | Maximum Assisted Mouth Opening (T5) |
|---|---|---|---|---|---|
| Group A | 1 | 26 | 43 | 28 | 46 |
| Group A | 2 | 34 | 45 | 38 | 49 |
| Group A | 3 | 24 | 38 | 24 | 41 |
| Group A | 4 | 18 | 42 | 25 | 47 |
| Group A | 5 | 38 | 45 | 41 | 46 |
| Group B | 6 | 21 | 27 | 23 | 32 |
| Group B | 7 | 41 | 44 | 42 | 47 |
| Group B | 8 | 20 | 36 | 27 | 38 |
| Group B | 9 | 31 | 34 | 36 | 38 |
| Group B | 10 | 15 | 30 | 20 | 34 |
| GROUP A | Average | 28 | 42.6 | 31.2 | 45.8 |
| Standard Deviation | 8 | 2.88 | 7.79 | 2.95 | |
| GROUP B | Average | 25.6 | 34.2 | 29.6 | 37.8 |
| Standard Deviation | 10.38 | 6.5 | 9.18 | 5.76 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Guarda Nardini, L.; Manfredini, D.; Colonna, A.; Ferrari Cagidiaco, E.; Ferrari, M.; Val, M. Intramuscular Botulinum Toxin as an Adjunct to Arthrocentesis with Viscosupplementation in Temporomandibular Disorders: A Proof-of-Concept Case–Control Investigation. Toxins 2024 , 16 , 364. https://doi.org/10.3390/toxins16080364
Guarda Nardini L, Manfredini D, Colonna A, Ferrari Cagidiaco E, Ferrari M, Val M. Intramuscular Botulinum Toxin as an Adjunct to Arthrocentesis with Viscosupplementation in Temporomandibular Disorders: A Proof-of-Concept Case–Control Investigation. Toxins . 2024; 16(8):364. https://doi.org/10.3390/toxins16080364
Guarda Nardini, Luca, Daniele Manfredini, Anna Colonna, Edoardo Ferrari Cagidiaco, Marco Ferrari, and Matteo Val. 2024. "Intramuscular Botulinum Toxin as an Adjunct to Arthrocentesis with Viscosupplementation in Temporomandibular Disorders: A Proof-of-Concept Case–Control Investigation" Toxins 16, no. 8: 364. https://doi.org/10.3390/toxins16080364
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Acad Pathol
- v.9(1); 2022
Educational case: Osteoarthritis
Jonathan light.
a School of Medicine, Eastern Virginia Medical School, Norfolk, VA, USA
Harrison Klause
b Department of Radiology, Eastern Virginia Medical School, USA
Richard M. Conran
c Department of Pathology & Anatomy, Eastern Virginia Medical School, Norfolk, VA, USA
The following fictional case is intended as a learning tool within the Pathology Competencies for Medical Education (PCME), a set of national standards for teaching pathology. These are divided into three basic competencies: Disease Mechanisms and Processes, Organ System Pathology, and Diagnostic Medicine and Therapeutic Pathology. For additional information, and a full list of learning objectives for all three competencies, see https://www.journals.elsevier.com/academic-pathology/news/pathology-competencies-for-medical-education-pcme . 1
Primary objective
Objective MS2.7: Arthritis. Compare and contrast rheumatoid and osteoarthritis including the etiology, pathogenesis, and morphology of each.
Competency 2: Organ System Pathology; Topic: MS: Musculoskeletal System; Learning Goal 2: Nonneoplastic Disorders of the Musculoskeletal System.
Patient presentation
The patient is a pleasant 60-year-old previously healthy woman who presents to the clinic with intermittent back pain, a painful right knee, and painful hands. She states that her right knee and hands are stiff for 30 min in the morning and resolve with activity. Her knee and hand pain are exacerbated by movement throughout the day but are relieved incompletely with rest. She states that bearing weight on her right knee has been more painful recently (mornings and evenings, 7 days per week) with the pain reaching a maximum of 7/10 compared with 4/10 previously, but the pain has slowly progressed for the past 24 months. In addition, she states she has had the pain in her hands and wrists for 2 or more years. She does not report a history of crystal-induced arthritis, such as gout or pseudogout, or Lyme disease. Surgical history includes bilateral endoscopic carpal tunnel release (ECTR) 1 year ago with persistent pain and tingling in her hands and wrists, cholecystectomy 10 years ago and an appendectomy as a child, but no joint surgeries or trauma. Her last menstrual period was 10 years ago. She has self-treated her musculoskeletal pain intermittently with ibuprofen for temporary relief and manages hypertension with lisinopril. Family history includes her mother has seropositive rheumatoid arthritis (RA), and her father has hypertension. Social history is negative for alcohol, tobacco, or recreational drug use. She was an equestrian until 5 years ago. She reports no recent sexual activity or history of a sexually transmitted infection. The patient has not changed her diet in the past 5 years, and her weight has been stable. On review of systems, she does not report night sweats, recent fevers, cough, headache, skin changes, or redness of her face or extremities, or other problems except for back, hand, and knee pain.
Diagnostic findings, Part 1
The patient's height is 67 inches, and she weighs 155 pounds. Body mass index is 24.3 kg/m 2 . Her vital signs are blood pressure 132/78 mmHg, heart rate 100 beats per minute, respiratory rate 12 breaths per minute, and temperature 98.2 °F. On physical examination (PE), her skin shows hypertrophic scarring of the ventral wrists at the ECTR surgical sites; there is no visible malar rash or target lesion. Head, ears, eyes, neck, and throat examination is unremarkable. The mucous membranes are moist, and she has a healthy dentition. The thyroid gland is normal in size and consistency, and cervical lymph nodes are regular. Cardiac examination demonstrates a regular rate and rhythm, with no gallops, rubs, or murmurs, and the lungs are clear to auscultation, with no wheezing, egophony, or crackles. Her abdominal examination is benign as there is no organomegaly or palpable masses; visible well-healed scars are evident from her previous appendectomy and cholecystectomy. Her musculoskeletal examination shows a medial bony irregularity and mild tenderness to palpation of the right patellofemoral joint and mild tenderness of the contralateral knee joint medially. The first carpometacarpal joint of both hands is tender to palpation. The hands and wrists demonstrate no erythema or warmth; however, some tenderness to palpation of the patient's ECTR scars is demonstrated. Tinel test (tapping over the affected median nerve elicits paresthesia of the palmar and distal first three-and-half digits) is positive bilaterally. Heberden's (distal interphalangeal [DIP] joint swelling) and Bouchard's (proximal interphalangeal [PIP] joint swelling) nodes are evident on the first, second, and third digits. The patient has mild tenderness to palpation over the lumbar back, with no obvious deformities; flexion and extension are limited due to pain, and there is no scoliosis or kyphosis. The right knee joint has varus deformity and exhibits crepitus with a limited range of motion (ROM); strength of 5/5. The right knee has no erythema or warmth but a mild effusion. The right hip strength is 5/5 and elicits no pain on palpation or movement. The straight leg raise test is normal bilaterally.
Questions/discussion points, Part 1
What is the differential diagnosis for polyarticular joint pain.
In general, different causes of polyarticular joint pain include infectious arthritis, osteoarthritis (OA), RA, crystal-induced arthritis, Lyme disease, hemochromatosis, and systemic lupus erythematosus (SLE). The absence of malar rash argues against SLE (sensitivity 57%, specificity 96%). 2 While the classic bull's eye lesion (circular target-like rash) supports a Lyme disease diagnosis, the rash may not always be present. Furthermore, five joints or fewer are affected simultaneously in a patient with Lyme disease, and the usual joints involved are knees, shoulder, elbow, wrist, or ankle. 3 Cancer metastasis could affect several joints but would typically be associated with unexplained weight loss, night sweats, or history of infections. A patient with hemochromatosis may have joint pain but may also have cirrhosis, heart failure, and bronzing of the skin.
What is the next step in the management of the patient in the clinical vignette?
The clinician should order conventional radiographs of the lumbar spine, bilateral hands, wrists, and right knee. OA and RA have distinct findings on conventional radiographs. 4 While OA is possible based on a history of chronic joint pain without relapsing episodes and the PE findings, bilateral wrist pain is not characteristic of OA. 5 , 6 PIP and DIP joint involvement, however, is common in OA. Typically, DIP joint sparing occurs in RA. 6 The American College of Rheumatologists (ACR) recommends imaging studies when the patient has decreased joint function, such as limited ROM. 7 If OA is high on the differential diagnosis, a conventional radiograph would yield any necessary information to make the diagnosis. Ultrasound is considered first for the patient due to being a portable, nonradiation study, with potential to identify specific joint pathologies. However, patients with severe joint disease may not be able to flex the knee enough to allow optimal visualization using ultrasound. The patient has a limited ROM, so conventional radiographs are necessary even if ultrasound identifies joint pathology.
Ultrasound is a cost-effective, noninvasive, specialized imaging technique used in cases of gout, OA, and RA. 8 In gout, the presence of the “snowstorm” sign appears due to uric acid crystal foci (hyperechoic) within the synovial fluid (hypoechoic). The clinician writing the ultrasound report should be specific when noting snowstorm sign of the affected joint in gout since snowstorm sign is also used in the ultrasonography of molar pregnancy. Ultrasound in OA is useful for detecting joint space narrowing and has a high sensitivity for demonstrating subchondral cysts or tendon or ligament damage surrounding the affected knee. 4 In RA, ultrasound may demonstrate acute synovial inflammation and tenosynovial effusion, sometimes in the setting of a subclinical presentation. 9 Therefore, ultrasound may be used to identify joint pathology and predict disease progression, also help with treatment. For patients with RA, ultrasound may improve early diagnosis and management during the ‘window of opportunity’ (before disease progression establishes significant damage to bone, cartilage, and tendon). 9 Furthermore, ultrasound has utility of being able to identify normal nerve and vessel architecture within the wrist. Therefore, ultrasound images of the patient's wrists are obtained to identify possible postoperative hypertrophic scar tissue causing traction or compression of her median nerve as a cause of her bilateral wrist pain based on a positive Tinel test on PE.
Diagnostic findings, Part 2
Imaging of the hand and knee were obtained ( Fig. 1 , Fig. 2 , Fig. 3 , Fig. 4 , Fig. 5 ).

Ultrasound of the knee. A. The scan shows joint margin destruction (arrow) suggestive of osteoarthritic change. The patient's knee is in the flexed position and the probe in the transverse approach. B. The scan is from a different patient that demonstrates the normal femoral cartilage (anechoic-dark) contour with uniform thickness for comparison. The patient's knee is in the flexed position and the probe in the transverse approach.

Right hand rheumatoid arthritis: Conventional anteroposterior (AP) radiograph of the right hand demonstrates advanced findings of rheumatoid arthritis characterized in this case by ankylosis of the carpal bones, juxta-articular osteoporosis, marked erosions, and subchondral cysts (arrow) along the radiocarpal, ulnocarpal, first carpometacarpal, metacarpophalangeal, and proximal interphalangeal joints with relative sparing of the distal interphalangeal joints.

Right hand osteoarthritis: Oblique radiograph of the right hand demonstrates degenerative osteoarthritis characterized by marginal osteophyte formation, joint space narrowing, and subchondral sclerosis in a distribution involving the first carpometacarpal joint, proximal, and distal interphalangeal joints, most conspicuous at the first interphalangeal, second (arrow), and third distal phalangeal joints.

Right knee osteoarthritis: Oblique (A) and lateral (B) radiographs of the right knee demonstrate advanced tricompartmental osteoarthritis, characterized by marked joint space narrowing and osteophyte formation, most conspicuous in the medial and patellofemoral compartments (arrow).

Lateral radiograph of the lumbar spine demonstrates multilevel degenerative changes of the thoracolumbar spine, characterized by disc space narrowing and end-plate osteophyte formation, most conspicuously evident at T12-L1 (arrow), as well as facet arthropathy at the lower lumbar spine (arrow) with associated retrolisthesis.
Questions/discussion points, Part 2
What is seen in the ultrasound scan of the knee.
Fig. 1 A is an ultrasound scan of a knee from a patient with a similar clinical presentation of knee pain, demonstrating joint margin destruction, suggesting osteoarthritic change. The patient's knee is in the flexed position, and the probe is in the transverse approach. Artifact versus osteoarthritic change was considered due to sound passing through two adjacent surfaces with different echogenicities but repeat images from different approaches combined with the clinical presentation were consistent with joint pathology. Documentation of ultrasound findings should include a written description of the findings and images added to the patient's chart. Fig. 1 B is an ultrasound scan of the knee from a patient that demonstrates the normal femoral cartilage (anechoic-dark) contour and uniform thickness for comparison. The patient's knee is in the flexed position, and the probe is in the transverse approach. The patient's ultrasound examination is clinically insufficient for diagnosis due to the limited ROM of her right knee, so conventional radiographs are obtained.
Additionally, ultrasonography of the patient's bilateral wrists demonstrates preservation of normal nerve architecture; however, no transverse carpal ligaments are identified, which is expected after CTR. The median nerve is observed bilaterally with some surrounding inflammation and compression by overlying tissue (presumably scar tissue). Snowstorm sign is not evident on any of the patient's joint ultrasounds; therefore, gout is less likely.
What is seen in the radiographs of the hand and knee?
Fig. 2 is a conventional anteroposterior (AP) radiograph of the right hand demonstrating advanced findings of RA characterized in this image by ankylosis of the carpal bones, juxta-articular osteoporosis, marked erosions and subchondral cysts along the radiocarpal, ulnocarpal, first carpometacarpal, metacarpophalangeal, and PIP joints with relative sparing of the DIP joints. Fig. 3 is a conventional oblique radiograph of the right hand, which demonstrates degenerative OA characterized by marginal osteophyte formation, joint space narrowing, and subchondral sclerosis in a distribution involving the first carpometacarpal joint, proximal and DIP joints, most conspicuous at the first interphalangeal, second and third distal phalangeal joints. Fig. 4 A–B are conventional oblique and lateral radiographs of the right knee, which demonstrate advanced tricompartmental OA, characterized by marked joint space narrowing and osteophyte formation, most conspicuous in the medial and patellofemoral compartments. Fig. 5 is a lateral radiograph of the lumbar spine that demonstrates multilevel degenerative changes of the thoracolumbar spine, characterized by disc space narrowing and end-plate osteophyte formation, most conspicuously evident at T12-L1, as well as facet arthropathy at the lower lumbar spine with associated retrolisthesis (a posterior slippage of the vertebra; the opposite of spondylolisthesis).
Which figure, Fig. 2 or Fig. 3 , best matches the clinical findings for the patient in the clinical vignette and why?
Fig. 2 demonstrates carpal bone ankylosis, potentially consistent with wrist pain, whereas Fig. 3 shows no carpal bone involvement. Fig. 3 demonstrates PIP and DIP joint involvement and involvement of the first carpometacarpal joint of both hands, which align with the PE findings. Fig. 3 is consistent with the patient's clinical presentation.
Discuss a possible cause of the Patient's wrist pain based on her past medical history
The patient's past medical history reveals ECTR. Carpal tunnel release may be surgically performed endoscopically or by the open technique (OCTR). ECTR is considered minimally invasive surgery. With ECTR, there is a 1.45% rate of transient neuropraxias compared to just 0.25% with the OCTR technique. 10 Neuropraxia may be due to iatrogenic injury and is a cause of postoperative symptoms such as paresthesia or motor weakness secondary to CTR; however, these symptoms are usually transient rather than persistent. Furthermore, ECTR has a significantly better outcome in terms of reducing trauma to nerves, arteries, or tendons compared to OCTR, 0.49% compared to 0.19%, respectively. 10 The outcomes of both ECTR and OCTR are generally good with a relatively low risk of injury. 10 Other studies have shown that ECTR and OCTR have comparable outcomes with lower incidences of scar associated postoperative complications in ECTR. 11 Sensitivity caused by scar tissue formation postoperatively is a significant consideration for the patient's wrist pain based on her ultrasound examination results and past medical history.
Which laboratory tests are needed to support osteoarthritis versus rheumatoid arthritis?
The most likely diagnoses based on history, clinical presentation, and imaging are OA and RA. Additionally, the patient's family history is seropositive for RA supporting the possibility of RA.
When there is a concern for RA, screening rheumatoid factor (RF) antibody, anti-citrullinated protein antibody (ACPA), and routine lab work is indicated, including complete blood cell counts (CBC), comprehensive metabolic panel (CMP), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). 5 The ACR advises against ordering routine lab arthritis panels for patients with joint pain. The diagnosis of OA is primarily clinical, based on history (joint stiffness for 30 min or less in the morning) and PE (joint crepitus and tenderness). 12 The ACR and European Alliance of Associations for Rheumatology (EULAR) have essential diagnostic criteria for knee OA, 12 which should be utilized by the clinician as there are no laboratory tests to diagnose OA.
The role of CBC in the patient's assessment is to screen for infection or malignancy. In the setting of infection as the cause of the patient's joint pain, leukocytosis would be evident (white blood cell count greater than 11,000 per mm 3 ). 13 Low white blood cell count (<4500/mm 3 ) 14 could indicate an autoimmune condition such as RA. CBC has less diagnostic utility in OA since OA is neither infectious nor autoimmune. ESR is a measure of inflammation, which is represented by an increased mass of clumped proteins and erythrocytes in the bottom of the laboratory centrifuge tube. ESR may be elevated in the setting of RA. CRP is a routinely used serum marker ordered by the clinician when there is concern for RA based on the clinical presentation and patient history. In patients with RA, there is a significant relationship between CRP levels and tissue inflammation scores from patient's knee synovium samples. 15 CRP levels may remain elevated chronically in patients with RA. 15 However, CRP levels are sometimes found to be significantly elevated in patients with OA. 16
As many as 50–80% of patients with RA have autoantibodies. 17 RA autoantibodies target the Fc portion of other IgG antibodies and are termed rheumatoid factor (RF). 18 ACPAs target proteins that contain citrulline and are prevalent in patients with RA. 18 However, RF or ACPAs may be measured in healthy individuals including those with OA. 18 RF and ACPAs have a sensitivity of 69% and 67% for patients with RA, while the specificity for RA is 85% and 95%, respectively. 18 The ACR/EULAR criteria for patients with RA heavily weigh RF and ACPAs for meeting diagnostic criteria. If the patient is negative for both RF and ACPA, zero criteria points are met, but if the patient is low or high positive for RF or ACPAs, two or three criteria points are assigned, respectively. 19 Therefore, patients who are ACPA seronegative require 10 or more joints to be affected to meet the criteria and those seropositive for ACPA still fulfill the criteria with only a single joint affected. Abnormal ESR or CRP meets one criteria point only, which supports the importance of the laboratory results (RF or ACPA seropositivity) in RA. 19
Diagnostic findings, Part 3
A CBC, CMP, ESR, CRP, and RF were obtained. The laboratory test results were within the normal range. The RF was seronegative.
Questions/discussion points, Part 3
What is the most likely diagnosis based on the clinical, imaging, and lab findings.
The patient has conventional radiographs that are consistent with OA, not RA. DIP joints are spared in RA. Additionally, there is limited ROM of the right knee and back on clinical examination, joint space narrowing and osteophytes on imaging (right knee and lumbar back), and a seronegative RF lab result. The presence of Bouchard's nodes and Heberden's nodes further supports OA as the diagnosis.
What are the diagnostic criteria for OA of the knee?
The EULAR recommendations require the following symptoms: knee pain, no early morning stiffness (EMS) or EMS ≤30 min, and functional limitation. The required clinical signs include crepitus, restricted ROM, bone enlargement, joint margin tenderness, and no palpable warmth. The ACR diagnostic criteria are that the individual must have knee pain and any three or more of the following: no EMS or EMS ≤30 min, crepitus, bone enlargement, joint margin tenderness, and no palpable warmth. The patient in the clinical vignette per the EULAR and ACR criteria meets the diagnostic requirements for knee OA.
Discuss the epidemiology of OA and RA
OA is the leading cause of joint disease worldwide. 20 Some estimates are that OA affects 10% of men and 18% of women over the age of 60. 20 The leading risk factor for OA is age 20 ; the prevalence increases exponentially after the age of 50. 6 Several nonhereditary possible contributions increase the risk of OA development, including systemic, biomechanics, and past injury. Genetics also plays a crucial role with at least 11 loci known. 20 As many as 14 million people in the United States have OA of the knee, roughly half are under 65. 21 Additionally, concomitant hand and knee OA more often affect women than men. 6 , 22 OA of the knee is clinically more common than the hip and hand. 12 OA accounts for an increased number of hospitalizations compared to RA. 22
RA is a chronic autoimmune disorder, which principally affects the joints. The incidence of RA is 0.5%–1.0%, 19 with an evident increase in the northern hemisphere from the south to north and rural to urban areas. 23 RA affects twice as many women as men, and the peak age is 50 years. 19 Positive family history for RA is significant clinically as there is a three to five times increased likelihood of developing RA when the family history is positive. 23 There is a 40%–65% hereditability seen for seropositive RA. 23 In seropositive RA, there are autoantibodies, including RF, ACPA, anti-carbamylated (anti-CarP) antibodies, and anti-acetylated protein antibodies. 19
What is the pathogenesis of OA and RA?
OA is a degenerative joint disease primarily affecting the articular cartilage of weight-bearing joints such as the hips, knees, spine, and fingers. 6 , 24 The pathogenesis of OA involves the entire joint: cartilage, subchondral bone, and soft tissues, including the synovium. 12 In OA, cartilage integrity is lost predominantly by biomechanical stress; however, genetic influences may result in early chondrocyte injury and disordered matrix repair. 6 There is an uneven balance in the repair mechanism. Proliferating chondrocytes synthesize matrix proteoglycans, but the degradation rate exceeds production in OA. 6 Diminishment of proteoglycans permits more water to interact with the collagen, causing swelling of the cartilage. 24 Additionally, chondrocytes secrete matrix metalloproteinases (MMPs), which break down the extracellular matrix type II collagen. 6 Chondrocytes and the adjacent synovium release soluble factors and pro-inflammatory cytokines, including transforming growth factor-beta (TGF-β), which stimulates the production of MMPs. 6 Other important modulators are tumor necrosis factor-alpha (TNF-α), prostaglandins (PGE 2 ), and nitric oxide, which all contribute to disease. 24 Eventually, chondrocyte depletion and irreversible matrix degradation occur in advanced OA. 6 Additional changes to the surrounding structures include meniscal degeneration, sclerosis of the underlying bone, osteophyte expansion at the joint margin, weakness of the surrounding joint muscles, ligamentous injury, and synovitis. 5 Genetics contribute to the development of OA via mutations in the COL2A1 gene, responsible for producing type II collagen, the main component of articular cartilage. 24
RA is a chronic autoimmune disorder primarily affecting the joints. T-helper CD4 + cells are principally responsible for the pathogenesis of RA. 6 The central cytokines involved in RA are interferon-gamma (IFN-γ), interleukin-17 (IL-17), IL-1, tumor necrosis factor (TNF), and receptor activator of nuclear factor kappa-B ligand (RANKL); TNF is the most important cytokine involved in RA pathogenesis. 6 These cytokines potentiate the inflammatory response. Antibodies directed against self-antigens lead to the pathologic changes seen in RA. 6 Some autoantibodies are directed against self-citrullinated peptides (ACPAs) in up to 70% of RA patients 6 and can include IgM, IgA, or IgG antibody classes. 23 In citrullination, arginine within a peptide is post-translationally modified to citrulline. Complement activation via the classic and alternative pathways by ACPAs leads to reduced complement levels and increased complement cleavage products within the synovial fluid of individuals with RA. 17 Many proteins within the joints are affected by citrullination, including within the hyaline cartilage, fibrinogen, type II collagen, the intermediate filament protein vimentin, and α-enolase, the glycolytic enzyme. 6 Additional autoantibodies present in up to 80% of RA patients are pentameric anti-IgM and dimeric anti-IgA, which target the Fc heavy chains of IgG; these two autoantibodies against Fcγ are called RF. 6 Genetics and environmental influences also contribute to RA development. 6 The HLA-DR4 allele is detected in roughly 50% of individuals with ACPA-positive RA. 6 Environmental factors including smoking and periodontal disease are implicated in RA pathogenesis due to increasing citrullination of self-peptides. 6
Compare and contrast the clinical findings in OA and RA
Joint involvement differs between OA and RA. While “joint mice” occur in OA, pannus (inflammatory synovium which migrates to the surface of the articular cartilage) formation and ankylosis (fibrous fusion of the joint) occur in RA. 24 Pannus formation in joints of individuals with RA occurs due to proliferation of synovial cells, inflammation (often with lymphoid aggregates, which are not observed in OA), angiogenesis, fibrin-laden exudate on articular joint surfaces, and subchondral bone resorption ( Fig. 6 , Fig. 7 ). 6 Joint loss in RA is characteristically juxta-articular, occurring on both sides of the joint. 24 Fissuring, eburnation, marginal joint osteophytes, and subchondral cysts are common findings in OA. Furthermore, extraskeletal manifestations of RA are rheumatoid nodules, which have a core of fibrinoid necrosis with palisading macrophages, surrounded by plasma cells and lymphocytes. 24 Rheumatoid nodules are characteristic of RA and present in the skin of the elbow and leg, areas that experience high pressure and these lesions are firm, mobile, rubbery, and sometimes tender. 24 However, the patient in the clinical vignette has a normal skin exam. Table 1 4 , 5 , 6 , 8 , 9 , 15 , 25 , 26 , 27 summarizes findings in OA and RA.

Rheumatoid arthritis. The hyperplastic synovium shows numerous finger-like villous projection that replaced the joint space.

Rheumatoid arthritis. The synovium shows hyperplasia with villous formation (arrows). Lymphoid aggregates are seen in the villi (arrowheads) (H&E, low magnification).
Table 1
Osteoarthritis (OA) versus rheumatoid arthritis (RA).
| OA | RA | |
|---|---|---|
| Demographics | ||
| Clinical signs | ||
| Laboratory value findings | ||
| Ultrasound signs | ||
| Radiographic signs | ||
| Morphology | ||
| Pharmacotherapy |
Diagnostic findings, Part 4
Fig. 8 is a section of lumbosacral spine obtained at autopsy from a patient with OA. Fig. 9 is an image of a bisected femoral head submitted for pathological examination form a patient with OA.

Section of vertebral column from a patient with osteoarthritis. Notice the intervertebral disc in the center of the image (∗) shows severe degenerative changes (Masson, low magnification).

Osteoarthritis. The gross image of the femoral head demonstrates erosion of the articular surface (arrowhead) with subchondral cyst (red arrow).
Questions/discussion points, Part 4
Describe the findings in the lumbosacral spine and femoral head.
Fig. 8 , a resection of the lumbosacral spine from another patient with OA progression at autopsy, shows narrowing of the joint space between two vertebral bodies secondary to degeneration of the intervertebral (IV) disc; marginal osteophytes surrounding the IV discs is evident.
The bisected femoral head from a patient with a similar bone morbidity caused by OA as the patient demonstrates erosion of the articular surface with a subchondral cyst on gross examination ( Fig. 9 ). The femoral head shows fibrillation, surface cracks in the articular cartilage, a feature characteristic of OA on microscopic examination ( Fig. 10 ). Loose bodies, dislodged fragments of articular cartilage, flake off the fibrillated surface into the joint space (referred to as joint mice) with progression of the OA ( Fig. 11 ).

Fragmented articular surface in osteoarthritis. The articular surface of bone in this image shows fragmentation of the articular surface, referred to as “fibrillation."

Low-power photograph showing fragmentation of the articular cartilage. Small fragments of cartilage may become detached and form loose bodies (“joint mice”) within the joint space (arrowheads).
What are the gross and histomorphologic findings of OA?
The histomorphometry of early OA is the loss of surface proteoglycans from the hyaline cartilage, which results in a decreased metachromatic staining. 24 Clusters of proliferating chondrocytes surrounded by basophilic staining matrix (territorial matrix) further characterize early OA. 6 , 24 Some chondrocytes die, leaving empty lacunae within the cartilage. 24 Several years later, OA may progress to fibrillations or cracks in the articular cartilage, which parallel its long axis. 24 Disease advances and fibrillations become oriented more perpendicular to the articular cartilage's long axis, in line with the type II collagen fibers within the cartilage matrix. 24 These defects in the articular cartilage become filled with synovial fluid. 24 Additionally, subchondral cysts develop secondary to synovial fluid within subchondral irregularities or bone fractures. 6 Chondrocytes eventually drop out, and entire cartilage units become detached, forming loose bodies, 6 also called joint mice. 28 This leads to nonuniform articular cartilage with erosion points and enhanced thickness of subchondral bone. 29 Subchondral bone is exposed and burnished by articulation with the opposing bone, such as the tibia plateau and femoral condyle, causing eburnation. 6 Osteophytes (bone spurs) occur at the joint margin 29 capped by articular hyaline cartilage and fibrocartilage, which slowly ossify. 6
Osteophytes are palpable at the PIP joints (Bouchard's nodes) and DIP joints (Heberden's nodes) in the patient in the clinical vignette; sometimes osteophytes are palpable at the knee joint. The patient in the clinical vignette has a palpable deformity of the medial right knee. Based on the clinical presentation and imaging, the bone deformity seen in this patient's right knee is consistent with an osteophyte. Additionally, the patient has a varus knee, causing increased medial joint cartilage damage, seen on clinical examination, imaging, and histology.
What are the costs associated with OA?
OA's healthcare costs in high-income countries are substantial, accounting for 1–2.5% of their gross domestic product. 12 Total hip and total knee replacements account for a majority of these costs. 12 However, the cost for the individual with OA, such as loss of personal savings due to decreased work, combined with national costs, exceeds direct healthcare costs. 12 The personal medical expenditure costs for the individual with OA was $2117 (CI 95%, $1268–2966) more than the average person, totaling $139.8 billion nationally in 2013. 30 Ambulatory care followed by prescriptions and inpatient hospital stay accounts for the three most significant expenditures in order from greatest to least. 30 OA was the second most expensive condition treated in United States hospitals in 2017. 31
What are current treatment options for OA?
Treatment for OA initially is nonpharmacologic. The ACR/Arthritis Foundation Guideline recommends first trying the “physical, psychosocial, and mind-body approaches” to managing OA of the knee. 32 For example, yoga, balance training, cognitive behavioral therapy (CBT), Tai Chi, weight loss, self-efficacy programs, or exercise are recommended for treating knee OA (KOA). 32 The patient in the clinical vignette may be offered a cane and instructed to unload the weight on her right knee by utilizing the cane in her left hand although her back pain may increase fall risk. 26 The clinician may refer the patient to a physical therapist (PT). 33 Additionally, a randomized trial demonstrated that an over-the-counter neoprene sleeve provided patients with symptomatic pain relief, particularly those with varus deformity of the knee secondary to OA. 33 Topical analgesics such as capsaicin is a first-line pharmacologic approach to avoid gastrointestinal toxicities caused by oral nonsteroidal anti-inflammatory drugs (NSAIDs). 33 The patient in the clinical vignette is given a neoprene sleeve and referred for physical therapy. NSAID therapy is also recommended if the topical analgesic fails to provide pain relief. While controversial, viscosupplementation using intra-articular hyaluronans (HAs) offers another treatment option. HA is a principle component of synovial fluid that is diluted in OA. 34 Some studies have shown that intra-articular HA injection is equally or more effective than NSAIDs or intra-articular corticosteroids for pain relief and functional improvement. 34 Because viscosupplementations have different chemical properties, cross-linking mechanisms, and formulations, the results of these studies may only apply to a subset of patients with symptomatic OA. 26 , 34 The use of oral narcotics such as tramadol are not recommended for individuals with OA of the knee. 26
Teaching points
- • Osteoarthritis (OA) is the most common joint disease worldwide, affecting more women than men.
- • Clinical examination of the osteoarthritic joint demonstrates mild tenderness, limited range of motion, and joint enlargement without effusion.
- • OA is primarily caused by biomechanical stress injuring the articular cartilage.
- • OA is characterized by increased joint cartilage degeneration and an unequal repair mechanism.
- • Wrist pain is uncommon in OA but is common in RA.
- • Joint stiffness in the morning for 30 min or less and joint pain worse with activity and better with rest is typical of OA.
- • Distal interphalangeal (DIP) sparing occurs in rheumatoid arthritis (RA), whereas DIP, PIP, and first MCP hand joints are most affected in OA.
- • Joint mice are loose bodies, dislodged fragments of articular cartilage, that flake off the fibrillated surface into the joint space, seen in OA.
- • RA is a chronic autoimmune disease primarily affecting joints.
- • RF is comprised of anti-IgM and anti-IgA against Fcγ. RF and ACPA seropositivity facilitate the diagnosis in RA patients based on ACR and EULAR guidelines.
- • Pannus, ankylosis, and rheumatoid nodule are common in RA. Few inflammatory cells are demonstrated on histology in OA.
- • Pannus is characterized by an inflammatory synovium which migrates to the surface of the articular cartilage with subchondral bone involvement.
- • Rheumatoid nodules have a core of fibrinoid necrosis with palisading macrophages, surrounded by lymphocytes and plasma cells. Rheumatoid nodules are characteristic of RA and present in the skin of the elbow and leg, areas that experience high pressure and these lesions are firm, mobile, rubbery, and sometimes tender. Extraskeletal manifestations are common in RA but not OA.
- • The principal cell involved in RA pathogenesis is the T-helper cell. TNF is the most important mediator of RA pathogenesis.
- • First-line treatment for OA involving the knee is a topical analgesic as well as nonpharmacologic management. Oral NSAIDs if tolerated are recommended to treat OA of the knee. Oral narcotics (tramadol) are not recommended for osteoarthritis of the knee. Viscosupplementation may be used for a subset of patients with symptomatic osteoarthritis of the knee.
Author's note
Fig. 6 , Fig. 7 , Fig. 8 , Fig. 9 , Fig. 10 , Fig. 11 were obtained during the scope of US government employment for Dr. Conran.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of competing interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of the article.

IMAGES
COMMENTS
Presentation of Case. Dr. Christopher V. Radcliffe (Medicine): A 46-year-old man was evaluated in the rheumatology clinic of this hospital because of arthritis and rash. One week before the ...
Case Study #4. Maria is a 66-year-old woman presenting to you for evaluation of knee pain, worse on the right. She states that she has had knee pain on the right for a few years, but it has progressively gotten worse and in the last 6 months or so she has noticed similar pain on the left.
Even the most benign causes of joint pain can lead to serious disability. The evaluation of a patient with joint pain calls for a detailed history and physical exam (often focusing on extra-articular findings) and occasionally the analysis of joint fluid, serologies, and radiologic tests. + +
Osteoarthritis is a common condition that is typically associated with older adults. Other causes of osteoarthritis, such as those cases resulting from childhood Perthes disease, can affect younger people and frequently have a major impact on the lives of those affected. This case report describes the experiences of one patient with osteoarthritis, using examples of her poetry to illustrate ...
Regional pain of a single joint is a common presentation ... depending upon, among other things, study setting and case definition. It concluded that rates of misuse averaged between 8 and 12% . (3) ... TENS has been used anecdotally for use in low back pain, but studies show conflicting recommendations on the matter.
Presentation of Case. Dr. Chidiebere D. Akusobi (Medicine): A 44-year-old woman was evaluated in the rheumatology clinic of this hospital because of proximal muscle weakness and myalgia. The ...
by Komal Ejaz, MD, and Adam Brown, MD. We present the case of a man in his 40s who came to Cleveland Clinic for evaluation of inflammatory arthritis, rash, facial swelling, abdominal pain and weight loss. The patient was in his usual state of health until October 2022, when he developed inflammatory pain involving small joints of the hands and ...
A 14-year-old boy was admitted with fatigue, fever, joint pain, abdominal cramping, and diarrhea. He had been well until 2 weeks earlier, when fatigue and fever developed on his final day of summer...
Background Hip pain is a common presentation treated by physical therapists and is most often musculoskeletal in nature. However, mechanical and pathological hip pain may present with similar signs and symptoms, so an early and comprehensive diagnostic approach is mandatory for appropriate intervention and to avoid serious complications. Case Presentation A 28-year-old woman presented with a 1 ...
This joint move- ment has been described as the joint arthrokine- matics, or the intricate movement of the joint ... pain relieving modalities into the rehabilitation pro- gram of a stiff and painful shoulder. TREATMENT REGIME Phase 1 0-30 degrees external rotation; 0-45 degrees ... CASE STUDIES Case One A 3
In Alpayci et al. 4) study, knee joint traction treatment was found to significantly decrease pain, which was consistent with this study's result. Continuous traction results in muscle relaxation, stimulation of dynamic muscle contractions, and inhibition of protective muscle reflection all of which are instrumental in decreasing pain 5 ) .
This case study examines a 23-year-old Active Duty woman who is preparing to be involuntarily released from military duty for an easily correctable medical condition. She has complained of chronic low back pain that radiates into her hip and down her leg since experiencing a work-related injury. She has been seen by numerous providers for the ...
Background A coracoid process fracture combined with an acromioclavicular (AC) joint dislocation is an uncommon injury that typically causes significant pain and limits shoulder movement. Open reduction and internal fixation have been the traditional treatment approach. However, arthroscopic techniques are emerging as a promising alternative for managing these injuries. Case representation A ...
This manuscript presents the interesting case study with an aim to present the importance of biomechanical evaluation and treatment, emphasizing on the evaluation of the auxiliary nerve involvement. ... Pain at the shoulder joint before the exercise was 8, and the pain level reduced to 6 in 4 days and to 4 in 2 weeks at the maximum joint range ...
Purpose: The purpose of this case study is to describe the management of a female patient with chronic left low back pain and sacroiliac joint pain (LBP/SIJP) using unique unilateral exercises developed by the Postural Restoration Institute (PRI) to address pelvic asymmetry and left hip capsule restriction, which is consistent with a Right Handed and Left Anterior Interior Chain pattern of ...
A total of nine studies were included, comprising five cohort studies, three cross-sectional studies, and one case-control study. Moderate level of evidence suggested a positive association of the presence and change of BMLs with the severity and progress of hip pain, and evidence for the associations between other MRI features and hip pain ...
A 40-year-old man presents to his primary care doctor complaining of pain in his ankles, knees, feet, heels, lower back and buttocks. His eye also appears to be inflamed. And, he reports having a burning sensation when urinating, which has become much more frequent. He has been experiencing these symptoms for three months and at times, the ...
History and physical examination lead to the correct diagnosis in most cases. The location, nature, timing, and quality of the pain are important clues for narrowing the differential diagnosis. In ...
About 30% of lumbar pain is caused by sacroiliac joint disfunction (Alayat et al., 2017). The problem often becomes chronic lower back pain of about 10-23% of people around the world (Diaz ...
Case studies in a musculoskeletal out-patients setting. Case study 1: Jaw Pain 217. Case study 2: Headache 218. Case study 3: Neck Pain - Case One 221. Case study 4: Neck Pain - Case Two 224. Case study 5: Thoracic Pain 226. Case study 6: Low Back Pain - Case One 228. Case study 7: Low Back Pain - Case Two 231.
This paper presents a case of a 35-year-old female patient diagnosed with Complex Regional Pain Syndrome (CRPS) type I and treated over a two-month period with a novel low-frequency sound-transduced focal pulsed stimulus. The patient received 21 treatments consisting of focally applied sound sweeps in the 15-100 Hz range. Outcome measures included the Visual Analogue Scale for pain, five ...
Case study 3: Providing advice for the management of mechanical joint pain symptoms. Prior reading: 'Pharmacy guide to joint pain: management' A woman aged 64 years comes into the pharmacy to pick up her husband's medication. When trying to open her bag, she tells the pharmacy technician she has been having some trouble with her hands.
The purpose of this case study was to describe the application of a novel evaluation and management algorithm for the treatment of a patient with SIJ dysfunction. Case presentation A 25-year-old male, active duty U.S. Marine, presented with a three-year history of left-sided lower back pain and intermittent radiating pain down the left ...
Eight case-control studies of 3476 patients described pain symptoms in a higher proportion of patients with FND than controls with other neurological disorders. A random effects model of 30 cohorts found that an estimated 55% (95% CI 46% to 64%) of 4272 patients with FND reported pain. ... (36%)), muscle pain (30/107 (28%)), joint pain (29/ ...
A 27 year old male presented to the Emergency Department (ED) with complaints of right knee pain and swelling for one week. Two weeks prior, he tripped while walking to work and began to feel pain in his right calf. Upon physical examination, swelling was noted in his ankles, knee, shoulders, and fingers. The knee and shoulder were tender to ...
Developing stronger leg muscles could help slow or prevent knee osteoarthritis, a new study found. Performing strength training to build muscle mass is key.
Criteria for inclusion in the study were the presence of mainly arthrogenous TMD pain, with a combined diagnosis of degenerative joint disease with arthralgia lasting for more than 6 months according to the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) with concurrent mild myofascial pain. Magnetic resonance imaging was used to ...
The study found that bicycling, whether outdoors or in a spinning class can help prevent knee pain and arthritis. While the exact mechanism of how biking helps to reduce risks of knee pain and ...
The following fictional case is intended as a learning tool within the Pathology Competencies for Medical Education (PCME), a set of national standards for teaching pathology. These are divided into three basic competencies: Disease Mechanisms and Processes, Organ System Pathology, and Diagnostic Medicine and Therapeutic Pathology.
Early on Friday morning, a 31-year-old female trainee doctor retired to sleep in a seminar hall after a gruelling day at one of India's oldest hospitals. It was the last time she was seen alive ...