Purdue Online Writing Lab Purdue OWL® College of Liberal Arts

Writing a Literature Review

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays). When we say “literature review” or refer to “the literature,” we are talking about the research ( scholarship ) in a given field. You will often see the terms “the research,” “the scholarship,” and “the literature” used mostly interchangeably.
Where, when, and why would I write a lit review?
There are a number of different situations where you might write a literature review, each with slightly different expectations; different disciplines, too, have field-specific expectations for what a literature review is and does. For instance, in the humanities, authors might include more overt argumentation and interpretation of source material in their literature reviews, whereas in the sciences, authors are more likely to report study designs and results in their literature reviews; these differences reflect these disciplines’ purposes and conventions in scholarship. You should always look at examples from your own discipline and talk to professors or mentors in your field to be sure you understand your discipline’s conventions, for literature reviews as well as for any other genre.
A literature review can be a part of a research paper or scholarly article, usually falling after the introduction and before the research methods sections. In these cases, the lit review just needs to cover scholarship that is important to the issue you are writing about; sometimes it will also cover key sources that informed your research methodology.
Lit reviews can also be standalone pieces, either as assignments in a class or as publications. In a class, a lit review may be assigned to help students familiarize themselves with a topic and with scholarship in their field, get an idea of the other researchers working on the topic they’re interested in, find gaps in existing research in order to propose new projects, and/or develop a theoretical framework and methodology for later research. As a publication, a lit review usually is meant to help make other scholars’ lives easier by collecting and summarizing, synthesizing, and analyzing existing research on a topic. This can be especially helpful for students or scholars getting into a new research area, or for directing an entire community of scholars toward questions that have not yet been answered.
What are the parts of a lit review?
Most lit reviews use a basic introduction-body-conclusion structure; if your lit review is part of a larger paper, the introduction and conclusion pieces may be just a few sentences while you focus most of your attention on the body. If your lit review is a standalone piece, the introduction and conclusion take up more space and give you a place to discuss your goals, research methods, and conclusions separately from where you discuss the literature itself.
Introduction:
- An introductory paragraph that explains what your working topic and thesis is
- A forecast of key topics or texts that will appear in the review
- Potentially, a description of how you found sources and how you analyzed them for inclusion and discussion in the review (more often found in published, standalone literature reviews than in lit review sections in an article or research paper)
- Summarize and synthesize: Give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: Don’t just paraphrase other researchers – add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically Evaluate: Mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: Use transition words and topic sentence to draw connections, comparisons, and contrasts.
Conclusion:
- Summarize the key findings you have taken from the literature and emphasize their significance
- Connect it back to your primary research question
How should I organize my lit review?
Lit reviews can take many different organizational patterns depending on what you are trying to accomplish with the review. Here are some examples:
- Chronological : The simplest approach is to trace the development of the topic over time, which helps familiarize the audience with the topic (for instance if you are introducing something that is not commonly known in your field). If you choose this strategy, be careful to avoid simply listing and summarizing sources in order. Try to analyze the patterns, turning points, and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred (as mentioned previously, this may not be appropriate in your discipline — check with a teacher or mentor if you’re unsure).
- Thematic : If you have found some recurring central themes that you will continue working with throughout your piece, you can organize your literature review into subsections that address different aspects of the topic. For example, if you are reviewing literature about women and religion, key themes can include the role of women in churches and the religious attitude towards women.
- Qualitative versus quantitative research
- Empirical versus theoretical scholarship
- Divide the research by sociological, historical, or cultural sources
- Theoretical : In many humanities articles, the literature review is the foundation for the theoretical framework. You can use it to discuss various theories, models, and definitions of key concepts. You can argue for the relevance of a specific theoretical approach or combine various theorical concepts to create a framework for your research.
What are some strategies or tips I can use while writing my lit review?
Any lit review is only as good as the research it discusses; make sure your sources are well-chosen and your research is thorough. Don’t be afraid to do more research if you discover a new thread as you’re writing. More info on the research process is available in our "Conducting Research" resources .
As you’re doing your research, create an annotated bibliography ( see our page on the this type of document ). Much of the information used in an annotated bibliography can be used also in a literature review, so you’ll be not only partially drafting your lit review as you research, but also developing your sense of the larger conversation going on among scholars, professionals, and any other stakeholders in your topic.
Usually you will need to synthesize research rather than just summarizing it. This means drawing connections between sources to create a picture of the scholarly conversation on a topic over time. Many student writers struggle to synthesize because they feel they don’t have anything to add to the scholars they are citing; here are some strategies to help you:
- It often helps to remember that the point of these kinds of syntheses is to show your readers how you understand your research, to help them read the rest of your paper.
- Writing teachers often say synthesis is like hosting a dinner party: imagine all your sources are together in a room, discussing your topic. What are they saying to each other?
- Look at the in-text citations in each paragraph. Are you citing just one source for each paragraph? This usually indicates summary only. When you have multiple sources cited in a paragraph, you are more likely to be synthesizing them (not always, but often
- Read more about synthesis here.
The most interesting literature reviews are often written as arguments (again, as mentioned at the beginning of the page, this is discipline-specific and doesn’t work for all situations). Often, the literature review is where you can establish your research as filling a particular gap or as relevant in a particular way. You have some chance to do this in your introduction in an article, but the literature review section gives a more extended opportunity to establish the conversation in the way you would like your readers to see it. You can choose the intellectual lineage you would like to be part of and whose definitions matter most to your thinking (mostly humanities-specific, but this goes for sciences as well). In addressing these points, you argue for your place in the conversation, which tends to make the lit review more compelling than a simple reporting of other sources.
- UConn Library
- Literature Review: The What, Why and How-to Guide
- Introduction
Literature Review: The What, Why and How-to Guide — Introduction
- Getting Started
- How to Pick a Topic
- Strategies to Find Sources
- Evaluating Sources & Lit. Reviews
- Tips for Writing Literature Reviews
- Writing Literature Review: Useful Sites
- Citation Resources
- Other Academic Writings
What are Literature Reviews?
So, what is a literature review? "A literature review is an account of what has been published on a topic by accredited scholars and researchers. In writing the literature review, your purpose is to convey to your reader what knowledge and ideas have been established on a topic, and what their strengths and weaknesses are. As a piece of writing, the literature review must be defined by a guiding concept (e.g., your research objective, the problem or issue you are discussing, or your argumentative thesis). It is not just a descriptive list of the material available, or a set of summaries." Taylor, D. The literature review: A few tips on conducting it . University of Toronto Health Sciences Writing Centre.
Goals of Literature Reviews
What are the goals of creating a Literature Review? A literature could be written to accomplish different aims:
- To develop a theory or evaluate an existing theory
- To summarize the historical or existing state of a research topic
- Identify a problem in a field of research
Baumeister, R. F., & Leary, M. R. (1997). Writing narrative literature reviews . Review of General Psychology , 1 (3), 311-320.
What kinds of sources require a Literature Review?
- A research paper assigned in a course
- A thesis or dissertation
- A grant proposal
- An article intended for publication in a journal
All these instances require you to collect what has been written about your research topic so that you can demonstrate how your own research sheds new light on the topic.
Types of Literature Reviews
What kinds of literature reviews are written?
Narrative review: The purpose of this type of review is to describe the current state of the research on a specific topic/research and to offer a critical analysis of the literature reviewed. Studies are grouped by research/theoretical categories, and themes and trends, strengths and weakness, and gaps are identified. The review ends with a conclusion section which summarizes the findings regarding the state of the research of the specific study, the gaps identify and if applicable, explains how the author's research will address gaps identify in the review and expand the knowledge on the topic reviewed.
- Example : Predictors and Outcomes of U.S. Quality Maternity Leave: A Review and Conceptual Framework: 10.1177/08948453211037398
Systematic review : "The authors of a systematic review use a specific procedure to search the research literature, select the studies to include in their review, and critically evaluate the studies they find." (p. 139). Nelson, L. K. (2013). Research in Communication Sciences and Disorders . Plural Publishing.
- Example : The effect of leave policies on increasing fertility: a systematic review: 10.1057/s41599-022-01270-w
Meta-analysis : "Meta-analysis is a method of reviewing research findings in a quantitative fashion by transforming the data from individual studies into what is called an effect size and then pooling and analyzing this information. The basic goal in meta-analysis is to explain why different outcomes have occurred in different studies." (p. 197). Roberts, M. C., & Ilardi, S. S. (2003). Handbook of Research Methods in Clinical Psychology . Blackwell Publishing.
- Example : Employment Instability and Fertility in Europe: A Meta-Analysis: 10.1215/00703370-9164737
Meta-synthesis : "Qualitative meta-synthesis is a type of qualitative study that uses as data the findings from other qualitative studies linked by the same or related topic." (p.312). Zimmer, L. (2006). Qualitative meta-synthesis: A question of dialoguing with texts . Journal of Advanced Nursing , 53 (3), 311-318.
- Example : Women’s perspectives on career successes and barriers: A qualitative meta-synthesis: 10.1177/05390184221113735
Literature Reviews in the Health Sciences
- UConn Health subject guide on systematic reviews Explanation of the different review types used in health sciences literature as well as tools to help you find the right review type
- << Previous: Getting Started
- Next: How to Pick a Topic >>
- Last Updated: Sep 21, 2022 2:16 PM
- URL: https://guides.lib.uconn.edu/literaturereview
Reference management. Clean and simple.
What is a literature review? [with examples]
What is a literature review?
The purpose of a literature review, how to write a literature review, the format of a literature review, general formatting rules, the length of a literature review, literature review examples, frequently asked questions about literature reviews, related articles.
A literature review is an assessment of the sources in a chosen topic of research.
In a literature review, you’re expected to report on the existing scholarly conversation, without adding new contributions.
If you are currently writing one, you've come to the right place. In the following paragraphs, we will explain:
- the objective of a literature review
- how to write a literature review
- the basic format of a literature review
Tip: It’s not always mandatory to add a literature review in a paper. Theses and dissertations often include them, whereas research papers may not. Make sure to consult with your instructor for exact requirements.
The four main objectives of a literature review are:
- Studying the references of your research area
- Summarizing the main arguments
- Identifying current gaps, stances, and issues
- Presenting all of the above in a text
Ultimately, the main goal of a literature review is to provide the researcher with sufficient knowledge about the topic in question so that they can eventually make an intervention.
The format of a literature review is fairly standard. It includes an:
- introduction that briefly introduces the main topic
- body that includes the main discussion of the key arguments
- conclusion that highlights the gaps and issues of the literature
➡️ Take a look at our guide on how to write a literature review to learn more about how to structure a literature review.
First of all, a literature review should have its own labeled section. You should indicate clearly in the table of contents where the literature can be found, and you should label this section as “Literature Review.”
➡️ For more information on writing a thesis, visit our guide on how to structure a thesis .
There is no set amount of words for a literature review, so the length depends on the research. If you are working with a large amount of sources, it will be long. If your paper does not depend entirely on references, it will be short.
Take a look at these three theses featuring great literature reviews:
- School-Based Speech-Language Pathologist's Perceptions of Sensory Food Aversions in Children [ PDF , see page 20]
- Who's Writing What We Read: Authorship in Criminological Research [ PDF , see page 4]
- A Phenomenological Study of the Lived Experience of Online Instructors of Theological Reflection at Christian Institutions Accredited by the Association of Theological Schools [ PDF , see page 56]
Literature reviews are most commonly found in theses and dissertations. However, you find them in research papers as well.
There is no set amount of words for a literature review, so the length depends on the research. If you are working with a large amount of sources, then it will be long. If your paper does not depend entirely on references, then it will be short.
No. A literature review should have its own independent section. You should indicate clearly in the table of contents where the literature review can be found, and label this section as “Literature Review.”
The main goal of a literature review is to provide the researcher with sufficient knowledge about the topic in question so that they can eventually make an intervention.

Literature Review - what is a Literature Review, why it is important and how it is done
What are literature reviews, goals of literature reviews, types of literature reviews, about this guide/licence.
- Strategies to Find Sources
- Evaluating Literature Reviews and Sources
- Tips for Writing Literature Reviews
- Writing Literature Review: Useful Sites
- Citation Resources
- Other Academic Writings
- Useful Resources
Help is Just a Click Away
Search our FAQ Knowledge base, ask a question, chat, send comments...
Go to LibAnswers
What is a literature review? "A literature review is an account of what has been published on a topic by accredited scholars and researchers. In writing the literature review, your purpose is to convey to your reader what knowledge and ideas have been established on a topic, and what their strengths and weaknesses are. As a piece of writing, the literature review must be defined by a guiding concept (e.g., your research objective, the problem or issue you are discussing, or your argumentative thesis). It is not just a descriptive list of the material available, or a set of summaries. " - Quote from Taylor, D. (n.d) "The literature review: A few tips on conducting it"
Source NC State University Libraries. This video is published under a Creative Commons 3.0 BY-NC-SA US license.
What are the goals of creating a Literature Review?
- To develop a theory or evaluate an existing theory
- To summarize the historical or existing state of a research topic
- Identify a problem in a field of research
- Baumeister, R.F. & Leary, M.R. (1997). "Writing narrative literature reviews," Review of General Psychology , 1(3), 311-320.
When do you need to write a Literature Review?
- When writing a prospectus or a thesis/dissertation
- When writing a research paper
- When writing a grant proposal
In all these cases you need to dedicate a chapter in these works to showcase what have been written about your research topic and to point out how your own research will shed a new light into these body of scholarship.
Literature reviews are also written as standalone articles as a way to survey a particular research topic in-depth. This type of literature reviews look at a topic from a historical perspective to see how the understanding of the topic have change through time.
What kinds of literature reviews are written?
- Narrative Review: The purpose of this type of review is to describe the current state of the research on a specific topic/research and to offer a critical analysis of the literature reviewed. Studies are grouped by research/theoretical categories, and themes and trends, strengths and weakness, and gaps are identified. The review ends with a conclusion section which summarizes the findings regarding the state of the research of the specific study, the gaps identify and if applicable, explains how the author's research will address gaps identify in the review and expand the knowledge on the topic reviewed.
- Book review essays/ Historiographical review essays : This is a type of review that focus on a small set of research books on a particular topic " to locate these books within current scholarship, critical methodologies, and approaches" in the field. - LARR
- Systematic review : "The authors of a systematic review use a specific procedure to search the research literature, select the studies to include in their review, and critically evaluate the studies they find." (p. 139). Nelson, L.K. (2013). Research in Communication Sciences and Disorders . San Diego, CA: Plural Publishing.
- Meta-analysis : "Meta-analysis is a method of reviewing research findings in a quantitative fashion by transforming the data from individual studies into what is called an effect size and then pooling and analyzing this information. The basic goal in meta-analysis is to explain why different outcomes have occurred in different studies." (p. 197). Roberts, M.C. & Ilardi, S.S. (2003). Handbook of Research Methods in Clinical Psychology . Malden, MA: Blackwell Pub.
- Meta-synthesis : "Qualitative meta-synthesis is a type of qualitative study that uses as data the findings from other qualitative studies linked by the same or related topic." (p.312). Zimmer, L. (2006). "Qualitative meta-synthesis: A question of dialoguing with texts," Journal of Advanced Nursing , 53(3), 311-318.
Guide adapted from "Literature Review" , a guide developed by Marisol Ramos used under CC BY 4.0 /modified from original.
- Next: Strategies to Find Sources >>
- Last Updated: Jul 3, 2024 10:56 AM
- URL: https://lit.libguides.com/Literature-Review
The Library, Technological University of the Shannon: Midwest
How to write a literature review introduction (+ examples)
The introduction to a literature review serves as your reader’s guide through your academic work and thought process. Explore the significance of literature review introductions in review papers, academic papers, essays, theses, and dissertations. We delve into the purpose and necessity of these introductions, explore the essential components of literature review introductions, and provide step-by-step guidance on how to craft your own, along with examples.
Why you need an introduction for a literature review
In academic writing , the introduction for a literature review is an indispensable component. Effective academic writing requires proper paragraph structuring to guide your reader through your argumentation. This includes providing an introduction to your literature review.
It is imperative to remember that you should never start sharing your findings abruptly. Even if there isn’t a dedicated introduction section .
When you need an introduction for a literature review
There are three main scenarios in which you need an introduction for a literature review:
What to include in a literature review introduction
It is crucial to customize the content and depth of your literature review introduction according to the specific format of your academic work.
Academic literature review paper
The introduction of an academic literature review paper, which does not rely on empirical data, often necessitates a more extensive introduction than the brief literature review introductions typically found in empirical papers. It should encompass:
Regular literature review section in an academic article or essay
In a standard 8000-word journal article, the literature review section typically spans between 750 and 1250 words. The first few sentences or the first paragraph within this section often serve as an introduction. It should encompass:
Introduction to a literature review chapter in thesis or dissertation
Some students choose to incorporate a brief introductory section at the beginning of each chapter, including the literature review chapter. Alternatively, others opt to seamlessly integrate the introduction into the initial sentences of the literature review itself. Both approaches are acceptable, provided that you incorporate the following elements:
Examples of literature review introductions
Example 1: an effective introduction for an academic literature review paper.
To begin, let’s delve into the introduction of an academic literature review paper. We will examine the paper “How does culture influence innovation? A systematic literature review”, which was published in 2018 in the journal Management Decision.
Example 2: An effective introduction to a literature review section in an academic paper
The second example represents a typical academic paper, encompassing not only a literature review section but also empirical data, a case study, and other elements. We will closely examine the introduction to the literature review section in the paper “The environmentalism of the subalterns: a case study of environmental activism in Eastern Kurdistan/Rojhelat”, which was published in 2021 in the journal Local Environment.
Thus, the author successfully introduces the literature review, from which point onward it dives into the main concept (‘subalternity’) of the research, and reviews the literature on socio-economic justice and environmental degradation.
Examples 3-5: Effective introductions to literature review chapters
Numerous universities offer online repositories where you can access theses and dissertations from previous years, serving as valuable sources of reference. Many of these repositories, however, may require you to log in through your university account. Nevertheless, a few open-access repositories are accessible to anyone, such as the one by the University of Manchester . It’s important to note though that copyright restrictions apply to these resources, just as they would with published papers.
Master’s thesis literature review introduction
Phd thesis literature review chapter introduction, phd thesis literature review introduction.
The last example is the doctoral thesis Metacognitive strategies and beliefs: Child correlates and early experiences Chan, K. Y. M. (Author). 31 Dec 2020 . The author clearly conducted a systematic literature review, commencing the review section with a discussion of the methodology and approach employed in locating and analyzing the selected records.
Steps to write your own literature review introduction
Master academia, get new content delivered directly to your inbox, the best answers to "what are your plans for the future", 10 tips for engaging your audience in academic writing, related articles, minor revisions: sample peer review comments and examples, sample emails to your thesis supervisor, co-authorship guidelines to successfully co-author a scientific paper, how to select a journal for publication as a phd student.
Harvey Cushing/John Hay Whitney Medical Library
- Collections
- Research Help
YSN Doctoral Programs: Steps in Conducting a Literature Review
- Biomedical Databases
- Global (Public Health) Databases
- Soc. Sci., History, and Law Databases
- Grey Literature
- Trials Registers
- Data and Statistics
- Public Policy
- Google Tips
- Recommended Books
- Steps in Conducting a Literature Review
What is a literature review?
A literature review is an integrated analysis -- not just a summary-- of scholarly writings and other relevant evidence related directly to your research question. That is, it represents a synthesis of the evidence that provides background information on your topic and shows a association between the evidence and your research question.
A literature review may be a stand alone work or the introduction to a larger research paper, depending on the assignment. Rely heavily on the guidelines your instructor has given you.
Why is it important?
A literature review is important because it:
- Explains the background of research on a topic.
- Demonstrates why a topic is significant to a subject area.
- Discovers relationships between research studies/ideas.
- Identifies major themes, concepts, and researchers on a topic.
- Identifies critical gaps and points of disagreement.
- Discusses further research questions that logically come out of the previous studies.
APA7 Style resources
APA Style Blog - for those harder to find answers
1. Choose a topic. Define your research question.
Your literature review should be guided by your central research question. The literature represents background and research developments related to a specific research question, interpreted and analyzed by you in a synthesized way.
- Make sure your research question is not too broad or too narrow. Is it manageable?
- Begin writing down terms that are related to your question. These will be useful for searches later.
- If you have the opportunity, discuss your topic with your professor and your class mates.
2. Decide on the scope of your review
How many studies do you need to look at? How comprehensive should it be? How many years should it cover?
- This may depend on your assignment. How many sources does the assignment require?
3. Select the databases you will use to conduct your searches.
Make a list of the databases you will search.
Where to find databases:
- use the tabs on this guide
- Find other databases in the Nursing Information Resources web page
- More on the Medical Library web page
- ... and more on the Yale University Library web page
4. Conduct your searches to find the evidence. Keep track of your searches.
- Use the key words in your question, as well as synonyms for those words, as terms in your search. Use the database tutorials for help.
- Save the searches in the databases. This saves time when you want to redo, or modify, the searches. It is also helpful to use as a guide is the searches are not finding any useful results.
- Review the abstracts of research studies carefully. This will save you time.
- Use the bibliographies and references of research studies you find to locate others.
- Check with your professor, or a subject expert in the field, if you are missing any key works in the field.
- Ask your librarian for help at any time.
- Use a citation manager, such as EndNote as the repository for your citations. See the EndNote tutorials for help.
Review the literature
Some questions to help you analyze the research:
- What was the research question of the study you are reviewing? What were the authors trying to discover?
- Was the research funded by a source that could influence the findings?
- What were the research methodologies? Analyze its literature review, the samples and variables used, the results, and the conclusions.
- Does the research seem to be complete? Could it have been conducted more soundly? What further questions does it raise?
- If there are conflicting studies, why do you think that is?
- How are the authors viewed in the field? Has this study been cited? If so, how has it been analyzed?
Tips:
- Review the abstracts carefully.
- Keep careful notes so that you may track your thought processes during the research process.
- Create a matrix of the studies for easy analysis, and synthesis, across all of the studies.
- << Previous: Recommended Books
- Last Updated: Jun 20, 2024 9:08 AM
- URL: https://guides.library.yale.edu/YSNDoctoral
- Library Homepage
Literature Review: The What, Why and How-to Guide: Literature Reviews?
- Literature Reviews?
- Strategies to Finding Sources
- Keeping up with Research!
- Evaluating Sources & Literature Reviews
- Organizing for Writing
- Writing Literature Review
- Other Academic Writings
What is a Literature Review?
So, what is a literature review .
"A literature review is an account of what has been published on a topic by accredited scholars and researchers. In writing the literature review, your purpose is to convey to your reader what knowledge and ideas have been established on a topic, and what their strengths and weaknesses are. As a piece of writing, the literature review must be defined by a guiding concept (e.g., your research objective, the problem or issue you are discussing, or your argumentative thesis). It is not just a descriptive list of the material available or a set of summaries." - Quote from Taylor, D. (n.d)."The Literature Review: A Few Tips on Conducting it".
- Citation: "The Literature Review: A Few Tips on Conducting it"
What kinds of literature reviews are written?
Each field has a particular way to do reviews for academic research literature. In the social sciences and humanities the most common are:
- Narrative Reviews: The purpose of this type of review is to describe the current state of the research on a specific research topic and to offer a critical analysis of the literature reviewed. Studies are grouped by research/theoretical categories, and themes and trends, strengths and weaknesses, and gaps are identified. The review ends with a conclusion section that summarizes the findings regarding the state of the research of the specific study, the gaps identify and if applicable, explains how the author's research will address gaps identify in the review and expand the knowledge on the topic reviewed.
- Book review essays/ Historiographical review essays : A type of literature review typical in History and related fields, e.g., Latin American studies. For example, the Latin American Research Review explains that the purpose of this type of review is to “(1) to familiarize readers with the subject, approach, arguments, and conclusions found in a group of books whose common focus is a historical period; a country or region within Latin America; or a practice, development, or issue of interest to specialists and others; (2) to locate these books within current scholarship, critical methodologies, and approaches; and (3) to probe the relation of these new books to previous work on the subject, especially canonical texts. Unlike individual book reviews, the cluster reviews found in LARR seek to address the state of the field or discipline and not solely the works at issue.” - LARR
What are the Goals of Creating a Literature Review?
- To develop a theory or evaluate an existing theory
- To summarize the historical or existing state of a research topic
- Identify a problem in a field of research
- Baumeister, R.F. & Leary, M.R. (1997). "Writing narrative literature reviews," Review of General Psychology , 1(3), 311-320.
When do you need to write a Literature Review?
- When writing a prospectus or a thesis/dissertation
- When writing a research paper
- When writing a grant proposal
In all these cases you need to dedicate a chapter in these works to showcase what has been written about your research topic and to point out how your own research will shed new light into a body of scholarship.
Where I can find examples of Literature Reviews?
Note: In the humanities, even if they don't use the term "literature review", they may have a dedicated chapter that reviewed the "critical bibliography" or they incorporated that review in the introduction or first chapter of the dissertation, book, or article.
- UCSB electronic theses and dissertations In partnership with the Graduate Division, the UC Santa Barbara Library is making available theses and dissertations produced by UCSB students. Currently included in ADRL are theses and dissertations that were originally filed electronically, starting in 2011. In future phases of ADRL, all theses and dissertations created by UCSB students may be digitized and made available.
Where to Find Standalone Literature Reviews
Literature reviews are also written as standalone articles as a way to survey a particular research topic in-depth. This type of literature review looks at a topic from a historical perspective to see how the understanding of the topic has changed over time.
- Find e-Journals for Standalone Literature Reviews The best way to get familiar with and to learn how to write literature reviews is by reading them. You can use our Journal Search option to find journals that specialize in publishing literature reviews from major disciplines like anthropology, sociology, etc. Usually these titles are called, "Annual Review of [discipline name] OR [Discipline name] Review. This option works best if you know the title of the publication you are looking for. Below are some examples of these journals! more... less... Journal Search can be found by hovering over the link for Research on the library website.
Social Sciences
- Annual Review of Anthropology
- Annual Review of Political Science
- Annual Review of Sociology
- Ethnic Studies Review
Hard science and health sciences:
- Annual Review of Biomedical Data Science
- Annual Review of Materials Science
- Systematic Review From journal site: "The journal Systematic Reviews encompasses all aspects of the design, conduct, and reporting of systematic reviews" in the health sciences.
- << Previous: Overview
- Next: Strategies to Finding Sources >>
- Last Updated: Mar 5, 2024 11:44 AM
- URL: https://guides.library.ucsb.edu/litreview
- University of Texas Libraries
Literature Reviews
- What is a literature review?
- Steps in the Literature Review Process
- Define your research question
- Determine inclusion and exclusion criteria
- Choose databases and search
- Review Results
- Synthesize Results
- Analyze Results
- Librarian Support
- Artificial Intelligence (AI) Tools
What is a Literature Review?
A literature or narrative review is a comprehensive review and analysis of the published literature on a specific topic or research question. The literature that is reviewed contains: books, articles, academic articles, conference proceedings, association papers, and dissertations. It contains the most pertinent studies and points to important past and current research and practices. It provides background and context, and shows how your research will contribute to the field.
A literature review should:
- Provide a comprehensive and updated review of the literature;
- Explain why this review has taken place;
- Articulate a position or hypothesis;
- Acknowledge and account for conflicting and corroborating points of view
From S age Research Methods
Purpose of a Literature Review
A literature review can be written as an introduction to a study to:
- Demonstrate how a study fills a gap in research
- Compare a study with other research that's been done
Or it can be a separate work (a research article on its own) which:
- Organizes or describes a topic
- Describes variables within a particular issue/problem
Limitations of a Literature Review
Some of the limitations of a literature review are:
- It's a snapshot in time. Unlike other reviews, this one has beginning, a middle and an end. There may be future developments that could make your work less relevant.
- It may be too focused. Some niche studies may miss the bigger picture.
- It can be difficult to be comprehensive. There is no way to make sure all the literature on a topic was considered.
- It is easy to be biased if you stick to top tier journals. There may be other places where people are publishing exemplary research. Look to open access publications and conferences to reflect a more inclusive collection. Also, make sure to include opposing views (and not just supporting evidence).
Source: Grant, Maria J., and Andrew Booth. “A Typology of Reviews: An Analysis of 14 Review Types and Associated Methodologies.” Health Information & Libraries Journal, vol. 26, no. 2, June 2009, pp. 91–108. Wiley Online Library, doi:10.1111/j.1471-1842.2009.00848.x.
Meryl Brodsky : Communication and Information Studies
Hannah Chapman Tripp : Biology, Neuroscience
Carolyn Cunningham : Human Development & Family Sciences, Psychology, Sociology
Larayne Dallas : Engineering
Janelle Hedstrom : Special Education, Curriculum & Instruction, Ed Leadership & Policy
Susan Macicak : Linguistics
Imelda Vetter : Dell Medical School
For help in other subject areas, please see the guide to library specialists by subject .
Periodically, UT Libraries runs a workshop covering the basics and library support for literature reviews. While we try to offer these once per academic year, we find providing the recording to be helpful to community members who have missed the session. Following is the most recent recording of the workshop, Conducting a Literature Review. To view the recording, a UT login is required.
- October 26, 2022 recording
- Last Updated: Jul 30, 2024 9:33 AM
- URL: https://guides.lib.utexas.edu/literaturereviews

Frequently asked questions
What is the purpose of a literature review.
There are several reasons to conduct a literature review at the beginning of a research project:
- To familiarize yourself with the current state of knowledge on your topic
- To ensure that you’re not just repeating what others have already done
- To identify gaps in knowledge and unresolved problems that your research can address
- To develop your theoretical framework and methodology
- To provide an overview of the key findings and debates on the topic
Writing the literature review shows your reader how your work relates to existing research and what new insights it will contribute.
Frequently asked questions: Academic writing
A rhetorical tautology is the repetition of an idea of concept using different words.
Rhetorical tautologies occur when additional words are used to convey a meaning that has already been expressed or implied. For example, the phrase “armed gunman” is a tautology because a “gunman” is by definition “armed.”
A logical tautology is a statement that is always true because it includes all logical possibilities.
Logical tautologies often take the form of “either/or” statements (e.g., “It will rain, or it will not rain”) or employ circular reasoning (e.g., “she is untrustworthy because she can’t be trusted”).
You may have seen both “appendices” or “appendixes” as pluralizations of “ appendix .” Either spelling can be used, but “appendices” is more common (including in APA Style ). Consistency is key here: make sure you use the same spelling throughout your paper.
The purpose of a lab report is to demonstrate your understanding of the scientific method with a hands-on lab experiment. Course instructors will often provide you with an experimental design and procedure. Your task is to write up how you actually performed the experiment and evaluate the outcome.
In contrast, a research paper requires you to independently develop an original argument. It involves more in-depth research and interpretation of sources and data.
A lab report is usually shorter than a research paper.
The sections of a lab report can vary between scientific fields and course requirements, but it usually contains the following:
- Title: expresses the topic of your study
- Abstract: summarizes your research aims, methods, results, and conclusions
- Introduction: establishes the context needed to understand the topic
- Method: describes the materials and procedures used in the experiment
- Results: reports all descriptive and inferential statistical analyses
- Discussion: interprets and evaluates results and identifies limitations
- Conclusion: sums up the main findings of your experiment
- References: list of all sources cited using a specific style (e.g. APA)
- Appendices: contains lengthy materials, procedures, tables or figures
A lab report conveys the aim, methods, results, and conclusions of a scientific experiment . Lab reports are commonly assigned in science, technology, engineering, and mathematics (STEM) fields.
The abstract is the very last thing you write. You should only write it after your research is complete, so that you can accurately summarize the entirety of your thesis , dissertation or research paper .
If you’ve gone over the word limit set for your assignment, shorten your sentences and cut repetition and redundancy during the editing process. If you use a lot of long quotes , consider shortening them to just the essentials.
If you need to remove a lot of words, you may have to cut certain passages. Remember that everything in the text should be there to support your argument; look for any information that’s not essential to your point and remove it.
To make this process easier and faster, you can use a paraphrasing tool . With this tool, you can rewrite your text to make it simpler and shorter. If that’s not enough, you can copy-paste your paraphrased text into the summarizer . This tool will distill your text to its core message.
Revising, proofreading, and editing are different stages of the writing process .
- Revising is making structural and logical changes to your text—reformulating arguments and reordering information.
- Editing refers to making more local changes to things like sentence structure and phrasing to make sure your meaning is conveyed clearly and concisely.
- Proofreading involves looking at the text closely, line by line, to spot any typos and issues with consistency and correct them.
The literature review usually comes near the beginning of your thesis or dissertation . After the introduction , it grounds your research in a scholarly field and leads directly to your theoretical framework or methodology .
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a thesis, dissertation , or research paper , in order to situate your work in relation to existing knowledge.
Avoid citing sources in your abstract . There are two reasons for this:
- The abstract should focus on your original research, not on the work of others.
- The abstract should be self-contained and fully understandable without reference to other sources.
There are some circumstances where you might need to mention other sources in an abstract: for example, if your research responds directly to another study or focuses on the work of a single theorist. In general, though, don’t include citations unless absolutely necessary.
An abstract is a concise summary of an academic text (such as a journal article or dissertation ). It serves two main purposes:
- To help potential readers determine the relevance of your paper for their own research.
- To communicate your key findings to those who don’t have time to read the whole paper.
Abstracts are often indexed along with keywords on academic databases, so they make your work more easily findable. Since the abstract is the first thing any reader sees, it’s important that it clearly and accurately summarizes the contents of your paper.
In a scientific paper, the methodology always comes after the introduction and before the results , discussion and conclusion . The same basic structure also applies to a thesis, dissertation , or research proposal .
Depending on the length and type of document, you might also include a literature review or theoretical framework before the methodology.
Whether you’re publishing a blog, submitting a research paper , or even just writing an important email, there are a few techniques you can use to make sure it’s error-free:
- Take a break : Set your work aside for at least a few hours so that you can look at it with fresh eyes.
- Proofread a printout : Staring at a screen for too long can cause fatigue – sit down with a pen and paper to check the final version.
- Use digital shortcuts : Take note of any recurring mistakes (for example, misspelling a particular word, switching between US and UK English , or inconsistently capitalizing a term), and use Find and Replace to fix it throughout the document.
If you want to be confident that an important text is error-free, it might be worth choosing a professional proofreading service instead.
Editing and proofreading are different steps in the process of revising a text.
Editing comes first, and can involve major changes to content, structure and language. The first stages of editing are often done by authors themselves, while a professional editor makes the final improvements to grammar and style (for example, by improving sentence structure and word choice ).
Proofreading is the final stage of checking a text before it is published or shared. It focuses on correcting minor errors and inconsistencies (for example, in punctuation and capitalization ). Proofreaders often also check for formatting issues, especially in print publishing.
The cost of proofreading depends on the type and length of text, the turnaround time, and the level of services required. Most proofreading companies charge per word or page, while freelancers sometimes charge an hourly rate.
For proofreading alone, which involves only basic corrections of typos and formatting mistakes, you might pay as little as $0.01 per word, but in many cases, your text will also require some level of editing , which costs slightly more.
It’s often possible to purchase combined proofreading and editing services and calculate the price in advance based on your requirements.
There are many different routes to becoming a professional proofreader or editor. The necessary qualifications depend on the field – to be an academic or scientific proofreader, for example, you will need at least a university degree in a relevant subject.
For most proofreading jobs, experience and demonstrated skills are more important than specific qualifications. Often your skills will be tested as part of the application process.
To learn practical proofreading skills, you can choose to take a course with a professional organization such as the Society for Editors and Proofreaders . Alternatively, you can apply to companies that offer specialized on-the-job training programmes, such as the Scribbr Academy .
Ask our team
Want to contact us directly? No problem. We are always here for you.
- Email [email protected]
- Start live chat
- Call +1 (510) 822-8066
- WhatsApp +31 20 261 6040

Our team helps students graduate by offering:
- A world-class citation generator
- Plagiarism Checker software powered by Turnitin
- Innovative Citation Checker software
- Professional proofreading services
- Over 300 helpful articles about academic writing, citing sources, plagiarism, and more
Scribbr specializes in editing study-related documents . We proofread:
- PhD dissertations
- Research proposals
- Personal statements
- Admission essays
- Motivation letters
- Reflection papers
- Journal articles
- Capstone projects
Scribbr’s Plagiarism Checker is powered by elements of Turnitin’s Similarity Checker , namely the plagiarism detection software and the Internet Archive and Premium Scholarly Publications content databases .
The add-on AI detector is powered by Scribbr’s proprietary software.
The Scribbr Citation Generator is developed using the open-source Citation Style Language (CSL) project and Frank Bennett’s citeproc-js . It’s the same technology used by dozens of other popular citation tools, including Mendeley and Zotero.
You can find all the citation styles and locales used in the Scribbr Citation Generator in our publicly accessible repository on Github .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Grad Med Educ
- v.8(3); 2016 Jul
The Literature Review: A Foundation for High-Quality Medical Education Research
a These are subscription resources. Researchers should check with their librarian to determine their access rights.
Despite a surge in published scholarship in medical education 1 and rapid growth in journals that publish educational research, manuscript acceptance rates continue to fall. 2 Failure to conduct a thorough, accurate, and up-to-date literature review identifying an important problem and placing the study in context is consistently identified as one of the top reasons for rejection. 3 , 4 The purpose of this editorial is to provide a road map and practical recommendations for planning a literature review. By understanding the goals of a literature review and following a few basic processes, authors can enhance both the quality of their educational research and the likelihood of publication in the Journal of Graduate Medical Education ( JGME ) and in other journals.
The Literature Review Defined
In medical education, no organization has articulated a formal definition of a literature review for a research paper; thus, a literature review can take a number of forms. Depending on the type of article, target journal, and specific topic, these forms will vary in methodology, rigor, and depth. Several organizations have published guidelines for conducting an intensive literature search intended for formal systematic reviews, both broadly (eg, PRISMA) 5 and within medical education, 6 and there are excellent commentaries to guide authors of systematic reviews. 7 , 8
- A literature review forms the basis for high-quality medical education research and helps maximize relevance, originality, generalizability, and impact.
- A literature review provides context, informs methodology, maximizes innovation, avoids duplicative research, and ensures that professional standards are met.
- Literature reviews take time, are iterative, and should continue throughout the research process.
- Researchers should maximize the use of human resources (librarians, colleagues), search tools (databases/search engines), and existing literature (related articles).
- Keeping organized is critical.
Such work is outside the scope of this article, which focuses on literature reviews to inform reports of original medical education research. We define such a literature review as a synthetic review and summary of what is known and unknown regarding the topic of a scholarly body of work, including the current work's place within the existing knowledge . While this type of literature review may not require the intensive search processes mandated by systematic reviews, it merits a thoughtful and rigorous approach.
Purpose and Importance of the Literature Review
An understanding of the current literature is critical for all phases of a research study. Lingard 9 recently invoked the “journal-as-conversation” metaphor as a way of understanding how one's research fits into the larger medical education conversation. As she described it: “Imagine yourself joining a conversation at a social event. After you hang about eavesdropping to get the drift of what's being said (the conversational equivalent of the literature review), you join the conversation with a contribution that signals your shared interest in the topic, your knowledge of what's already been said, and your intention.” 9
The literature review helps any researcher “join the conversation” by providing context, informing methodology, identifying innovation, minimizing duplicative research, and ensuring that professional standards are met. Understanding the current literature also promotes scholarship, as proposed by Boyer, 10 by contributing to 5 of the 6 standards by which scholarly work should be evaluated. 11 Specifically, the review helps the researcher (1) articulate clear goals, (2) show evidence of adequate preparation, (3) select appropriate methods, (4) communicate relevant results, and (5) engage in reflective critique.
Failure to conduct a high-quality literature review is associated with several problems identified in the medical education literature, including studies that are repetitive, not grounded in theory, methodologically weak, and fail to expand knowledge beyond a single setting. 12 Indeed, medical education scholars complain that many studies repeat work already published and contribute little new knowledge—a likely cause of which is failure to conduct a proper literature review. 3 , 4
Likewise, studies that lack theoretical grounding or a conceptual framework make study design and interpretation difficult. 13 When theory is used in medical education studies, it is often invoked at a superficial level. As Norman 14 noted, when theory is used appropriately, it helps articulate variables that might be linked together and why, and it allows the researcher to make hypotheses and define a study's context and scope. Ultimately, a proper literature review is a first critical step toward identifying relevant conceptual frameworks.
Another problem is that many medical education studies are methodologically weak. 12 Good research requires trained investigators who can articulate relevant research questions, operationally define variables of interest, and choose the best method for specific research questions. Conducting a proper literature review helps both novice and experienced researchers select rigorous research methodologies.
Finally, many studies in medical education are “one-offs,” that is, single studies undertaken because the opportunity presented itself locally. Such studies frequently are not oriented toward progressive knowledge building and generalization to other settings. A firm grasp of the literature can encourage a programmatic approach to research.
Approaching the Literature Review
Considering these issues, journals have a responsibility to demand from authors a thoughtful synthesis of their study's position within the field, and it is the authors' responsibility to provide such a synthesis, based on a literature review. The aforementioned purposes of the literature review mandate that the review occurs throughout all phases of a study, from conception and design, to implementation and analysis, to manuscript preparation and submission.
Planning the literature review requires understanding of journal requirements, which vary greatly by journal ( table 1 ). Authors are advised to take note of common problems with reporting results of the literature review. Table 2 lists the most common problems that we have encountered as authors, reviewers, and editors.
Sample of Journals' Author Instructions for Literature Reviews Conducted as Part of Original Research Article a

Common Problem Areas for Reporting Literature Reviews in the Context of Scholarly Articles

Locating and Organizing the Literature
Three resources may facilitate identifying relevant literature: human resources, search tools, and related literature. As the process requires time, it is important to begin searching for literature early in the process (ie, the study design phase). Identifying and understanding relevant studies will increase the likelihood of designing a relevant, adaptable, generalizable, and novel study that is based on educational or learning theory and can maximize impact.
Human Resources
A medical librarian can help translate research interests into an effective search strategy, familiarize researchers with available information resources, provide information on organizing information, and introduce strategies for keeping current with emerging research. Often, librarians are also aware of research across their institutions and may be able to connect researchers with similar interests. Reaching out to colleagues for suggestions may help researchers quickly locate resources that would not otherwise be on their radar.
During this process, researchers will likely identify other researchers writing on aspects of their topic. Researchers should consider searching for the publications of these relevant researchers (see table 3 for search strategies). Additionally, institutional websites may include curriculum vitae of such relevant faculty with access to their entire publication record, including difficult to locate publications, such as book chapters, dissertations, and technical reports.
Strategies for Finding Related Researcher Publications in Databases and Search Engines

Search Tools and Related Literature
Researchers will locate the majority of needed information using databases and search engines. Excellent resources are available to guide researchers in the mechanics of literature searches. 15 , 16
Because medical education research draws on a variety of disciplines, researchers should include search tools with coverage beyond medicine (eg, psychology, nursing, education, and anthropology) and that cover several publication types, such as reports, standards, conference abstracts, and book chapters (see the box for several information resources). Many search tools include options for viewing citations of selected articles. Examining cited references provides additional articles for review and a sense of the influence of the selected article on its field.
Box Information Resources
- Web of Science a
- Education Resource Information Center (ERIC)
- Cumulative Index of Nursing & Allied Health (CINAHL) a
- Google Scholar
Once relevant articles are located, it is useful to mine those articles for additional citations. One strategy is to examine references of key articles, especially review articles, for relevant citations.
Getting Organized
As the aforementioned resources will likely provide a tremendous amount of information, organization is crucial. Researchers should determine which details are most important to their study (eg, participants, setting, methods, and outcomes) and generate a strategy for keeping those details organized and accessible. Increasingly, researchers utilize digital tools, such as Evernote, to capture such information, which enables accessibility across digital workspaces and search capabilities. Use of citation managers can also be helpful as they store citations and, in some cases, can generate bibliographies ( table 4 ).
Citation Managers

Knowing When to Say When
Researchers often ask how to know when they have located enough citations. Unfortunately, there is no magic or ideal number of citations to collect. One strategy for checking coverage of the literature is to inspect references of relevant articles. As researchers review references they will start noticing a repetition of the same articles with few new articles appearing. This can indicate that the researcher has covered the literature base on a particular topic.
Putting It All Together
In preparing to write a research paper, it is important to consider which citations to include and how they will inform the introduction and discussion sections. The “Instructions to Authors” for the targeted journal will often provide guidance on structuring the literature review (or introduction) and the number of total citations permitted for each article category. Reviewing articles of similar type published in the targeted journal can also provide guidance regarding structure and average lengths of the introduction and discussion sections.
When selecting references for the introduction consider those that illustrate core background theoretical and methodological concepts, as well as recent relevant studies. The introduction should be brief and present references not as a laundry list or narrative of available literature, but rather as a synthesized summary to provide context for the current study and to identify the gap in the literature that the study intends to fill. For the discussion, citations should be thoughtfully selected to compare and contrast the present study's findings with the current literature and to indicate how the present study moves the field forward.
To facilitate writing a literature review, journals are increasingly providing helpful features to guide authors. For example, the resources available through JGME include several articles on writing. 17 The journal Perspectives on Medical Education recently launched “The Writer's Craft,” which is intended to help medical educators improve their writing. Additionally, many institutions have writing centers that provide web-based materials on writing a literature review, and some even have writing coaches.
The literature review is a vital part of medical education research and should occur throughout the research process to help researchers design a strong study and effectively communicate study results and importance. To achieve these goals, researchers are advised to plan and execute the literature review carefully. The guidance in this editorial provides considerations and recommendations that may improve the quality of literature reviews.
Literature Reviews (in the Health Sciences)
- Goals of a Literature Review
- Select Citation Management Software
- Select databases to search
- Conduct searches
- Track your searches
- Select articles to include
- Extract information from articles
- Structure your review
- Find "fill-in" information
- Other sources and help
Keeping these goals in mind throughout your project will help you stay organized and focused.
A literature review helps the author:
- Understand the scope, history, and present state of knowledge in a specific topic
- Understand application of research concepts such as statistical tests and methodological choices
- Create a research project that complements the existing research or fills in gaps
A literature review helps the reader:
- Understand how your research project fits into the existing knowledge and research in a field
- Understand that a topic is important/relevant to the world and persuade them to keep reading your project
- << Previous: Home
- Next: Select Citation Management Software >>
- Last Updated: Jul 29, 2024 2:12 PM
- URL: https://libguides.usc.edu/healthsciences/LitReview
- Open access
- Published: 26 August 2021
Advancing sustainable development goals through immunization: a literature review
- Catherine Decouttere 1 ,
- Kim De Boeck 1 &
- Nico Vandaele ORCID: orcid.org/0000-0001-7687-7376 1
Globalization and Health volume 17 , Article number: 95 ( 2021 ) Cite this article
18k Accesses
40 Citations
33 Altmetric
Metrics details
Immunization directly impacts health (SDG3) and brings a contribution to 14 out of the 17 Sustainable Development Goals (SDGs), such as ending poverty, reducing hunger, and reducing inequalities. Therefore, immunization is recognized to play a central role in reaching the SDGs, especially in low- and middle-income countries (LMICs). Despite continuous interventions to strengthen immunization systems and to adequately respond to emergency immunization during epidemics, the immunization-related indicators for SDG3 lag behind in sub-Saharan Africa. Especially taking into account the current Covid19 pandemic, the current performance on the connected SDGs is both a cause and a result of this.
We conduct a literature review through a keyword search strategy complemented with handpicking and snowballing from earlier reviews. After title and abstract screening, we conducted a qualitative analysis of key insights and categorized them according to showing the impact of immunization on SDGs, sustainability challenges, and model-based solutions to these challenges.
We reveal the leveraging mechanisms triggered by immunization and position them vis-à-vis the SDGs, within the framework of Public Health and Planetary Health. Several challenges for sustainable control of vaccine-preventable diseases are identified: access to immunization services, global vaccine availability to LMICs, context-dependent vaccine effectiveness, safe and affordable vaccines, local/regional vaccine production, public-private partnerships, and immunization capacity/capability building. Model-based approaches that support SDG-promoting interventions concerning immunization systems are analyzed in light of the strategic priorities of the Immunization Agenda 2030.
Conclusions
In general terms, it can be concluded that relevant future research requires (i) design for system resilience, (ii) transdisciplinary modeling, (iii) connecting interventions in immunization with SDG outcomes, (iv) designing interventions and their implementation simultaneously, (v) offering tailored solutions, and (vi) model coordination and integration of services and partnerships. The research and health community is called upon to join forces to activate existing knowledge, generate new insights and develop decision-supporting tools for Low-and Middle-Income Countries’ health authorities and communities to leverage immunization in its transformational role toward successfully meeting the SDGs in 2030.
With just one decade ahead to realize 17 ambitious but essential SDGs, most Sub-Saharan African (SSA) countries are struggling to meet and to sustain SDG3 Footnote 1 targets related to immunization: under-five mortality, elimination of vaccine-preventable diseases, and prevention of epidemics. There is a growing concern to support the transformation of immunization systems towards increased sustainability and resilience [ 1 , 2 ]. The 2020 Covid-19 pandemic supports this concern clearly, as it draws global attention and funds to restoring health systems across the globe and to the development of a vaccine, in an attempt to mitigate the devastating health and economic impact of the full-blown pandemic. Health care staff in Lower and Middle-Income Countries (LMICs) need to prepare their mostly weak health systems, already overburdened by ongoing struggles with active outbreaks of infectious diseases such as Measles, Ebola, and Lassa Fever, only to name a few.
Immunization directly impacts health (SDG3) and brings a contribution to 14 out of the 17 SDGs [ 3 ]. Moreover, it has proven to be one of the most cost-effective and long-lasting health interventions [ 4 ], protecting individuals and communities both in stable times and during humanitarian crises.
Advancing both the health-related and other SDGs in LMICs through immunization requires appropriate methods and tools that can support strategic decision-making and program implementation. Furthermore, a multi-sectoral perspective within a system-based approach, that involves the relevant SDG dimensions, seems mandatory to preserve sustainability. This entails the observation that immunization is at the interface between natural and human-made systems. Although the existence of many bi-directional links between the two systems, this paper will focus on the sustainable impact of immunization on the SDGs. A core element within this system-based approach is the notion of adaptability as a means to endorse resilience.
The natural system houses pathogens (e.g., bacteria, viruses, parasites) in reservoirs such as soil, water, plants, animals, and humans. When humans are exposed to pathogens, the immune system is activated. If the activation is not effective, an infection takes place including further transmission. An infection survivor gains immunity and if enough in number, a community can develop herd immunity. Susceptibility of the population is related to the strength of the immune response against the pathogen, which is linked to age, nutrition, previous infection, and general health status. This points to the impact of immunization on other SDGs than SDG3 and vice versa.
Driven by environmental change due to natural or anthropogenic causes, such as floods, river dam constructions, conversion of forest into farmland, or climate change, pathogen ecologies adapt accordingly. This adaptation is key and gives rise to the presence of pathogens in environments where they could not flourish before. The same happens when an infected human travels or migrates to uninfected areas. A pathogen entering a new area is not recognized by the population’s naïve immune systems. Therefore it can emerge in communities and result in outbreaks, larger epidemics, or even pandemics like Covid-19.
Zoonoses are diseases that are transmissible from vertebrate animals, such as pets, livestock, or wildlife, to humans. Driven by ecological disruption and increased contact between humans and wild reservoir species, these pathogens found the opportunity to “jump the species barrier”, leading to a new human infectious disease. In specific, anthropogenic environmental disturbance, including the increased livestock population in close contact with wildlife animal populations, increased the risk of zoonotic infection from wildlife [ 5 ]. Furthermore, emerging infectious diseases are fueled by increasing population density in urban areas and the interaction between humans and wildlife, through encroachment, road building, deforestation, hunting, and global wildlife trade [ 5 ]. In addition, loss of biodiversity following anthropogenic disturbance was shown to increase the abundance of rodent-borne pathogens in central Kenya [ 6 ]. Most pandemic threats have been caused by viruses from zoonotic or vector-borne sources [ 7 ]: Ebola, SARS, MERS, H1N1 pandemic flu, and eventually also Covid-19.
These phenomena represent adaptive behavior and are clearly bidirectional in their interaction with the human-made immunization system. Concluded, there is an intimate connection between environmental, animal, and human health. The typical behavior attributed to social-ecological systems, as described by Whitmee et al. [ 8 ] applies: these systems coevolve across spatial and temporal scales, which explains endemic and emerging disease behavior, nonlinearity in disease transmission outside and during outbreaks, and scale-free phenomena such as a single adapted virus in a single infected traveler that is capable of infecting entire continents.
By providing an analysis of the existing body of research dedicated to sustainable immunization and by showing directions for future research in this field, we contribute to support the strategic priorities of the Immunization Agenda 2030 and contribute to the other SDGs.
In this paper, we discuss insights based on a literature review in which we explored (a) how immunization impacts the SDGs, (b) the factors that endanger the sustainability of immunization in LMICs (c) the research gap to enhance decision making for SDG-promoting implementations related to immunization.
Search strategy and information sources
Considering the broad array of disciplines involved, including epidemiology, system research, operations management, and anthropology, both Scopus and Pubmed databases were initially searched between January 1st 1990 and March 21, 2021. As the search term based on the SDGs needed to be expanded in order to identify papers before 2015 and papers that clearly expressed the idea behind sustainable development without mentioning the SDGs, it was replaced by variations of sustainability and resilience, which finally resulted in 3401 papers as shown in Table 1 .
Similar searches were performed in Pubmed. While screening the papers based on titles and abstracts, additional papers were handpicked and found through snowballing from review papers.
Data extraction and synthesis
Title screening removed papers without a direct connection to the SDGs, such as theoretical topics in immunology and vaccinology, vaccine efficacy and clinical trials, technical papers on human or veterinary vaccine development, and papers related to cybersecurity.
Abstract screening mainly removed papers on livestock immunization or detailed human immunology. Similarly, papers that only briefly listed the sustainability aspect in the limitations section of their research were excluded at this point. in terms of eligibility, papers dealing with models and methods that qualify as applicable and relevant for decision-makers, implementers, and other stakeholders were included. the insights from all the resulting papers were extracted in excel for qualitative synthesis. The inclusion criteria were based on Kovacs and Moshtari [ 9 ] and Besiou, Stapleton, and Van Wassenhove [ 10 ], as shown in Table 2 .
The analysis turned out the paper structure as shown in Fig. 1 . All eligible and included papers, for which the numbers are listed in Table 3 , were manually allocated to three categories. This has been initiated by one researcher and reviewed independently by two other researchers. A final meeting was arranged to reach a consensus.
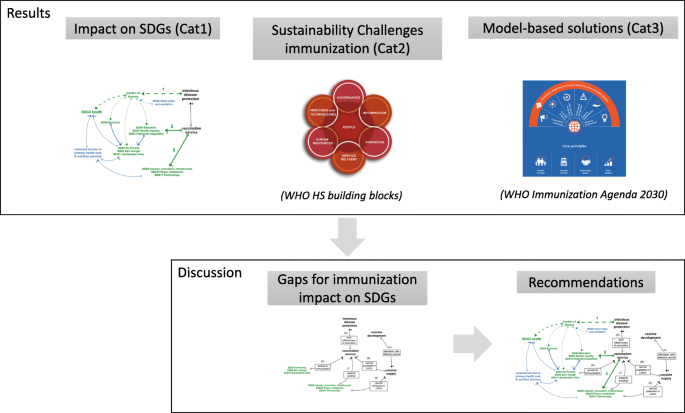
Paper structure. Paper structure combining literature analysis results with both the WHO Health System building blocks [ 11 ] and the WHO Immunization Agenda 2030 [ 2 ]
The insights from the qualitatively analyzed papers are categorized as follows: first (Cat1), insights that explain the essential role of immunization in LMICs for reaching the SDGs; second (Cat2), insights that represent challenges concerning the sustainability of the immunization system in LMICs; and third (Cat3), insights that propose model-based approaches to these challenges. From the Cat3 papers, modeling and methodological learnings could be drawn, which support strategies for immunization system improvement and for transformation towards achieving the SDGs. By comparing the challenges (Cat2) and model-based approaches (Cat3) found in the literature, under-addressed research fields were distilled and finally, recommendations are formulated. A synopsis is given in Table 3 .
Following the application of the inclusion criteria, a number of applied research papers that investigated the potential value of an intervention or optimal strategies within a single field, or in multiple fields but failing to make a connection with the SDGs, were not discussed in the Cat3 papers. However, the insights from these papers include promising elements to be leveraged by translational research in order to result in evidence-based decision support. Additionally, the interested reader is referred to De Boeck [ 19 ] for vaccine supply chain-related papers. Finally, the insights from the Cat1 papers have been used to formulate conceptual models, link the various elements and relate these elements to the SDGs, the Cat2 revealed the immunization challenges and the Cat3 allowed us to obtain an overview of model-based solutions. For each of these three steps, a focused group model building session was set up. The outcomes were iteratively validated until saturation was obtained.
The findings are structured according to the categories of Table 3 . First, the impact of immunization on the SDGs is discussed. Subsequently, the challenges for the sustainability of immunization are reviewed, and finally, the model-based approaches to solve these sustainability challenges are presented.
Impact of immunization on SDGs
The conceptual diagram in Fig. 2 represents the three pathways, identified from the reviewed papers, together with the ultimate impact these pathways have on the SDGs (both the pathways and the impact links are indicated in green). The first pathway (1) leads from the protection against vaccine-preventable diseases to a lower burden of disease and as such to a positive contribution to SDG3 and several other SDGs. A second pathway (2) leads from the vaccination service delivery to improved SDGs for the direct beneficiaries of immunization. A third pathway (3) also starts from vaccination service delivery and heads to SDG 17, 16, and 9, as the Expanded Program on Immunization (EPI) paves the way for partnerships in the context of health-related service delivery, that can be integrated with immunization and will lead to universal health coverage, ultimately contributing to SDG3. The indirect effects of immunization on the SDGs shown in blue, are only briefly discussed, as they lie outside the scope of this literature review.
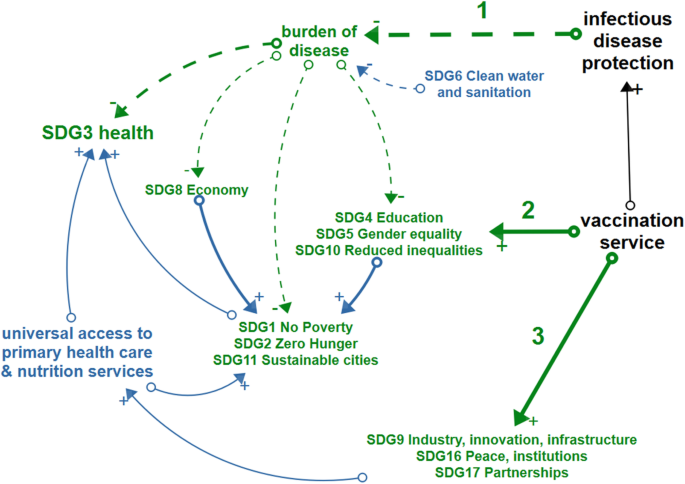
Conceptual model. Green items depict the impact of immunization on sustainable development goals which is realized through the mechanisms of (1) protecting people and communities against infectious diseases, (2) providing access to immunization services for all and (3) creating an environment for health system development. Blue arrows indicate the indirect consequences of immunization on SDGs. Black items show the overarching elements of sustainable immunization
In the following sections, the three pathways are discussed based on the Cat1 papers, referenced in Table 3 , while Table 4 gives a summary of each contribution of immunization to the SDGs.
Impact of protecting people and communities against vaccine-preventable diseases
One of the joint creeds of WHO and GAVI, “Immunization leads to saving lives, protecting health, and contributing to healthy and productive populations” [ 2 , 39 ], summarizes the impact of protecting individuals and communities against vaccine-preventable diseases and refers primarily to SDG3 – health and well-being, but also to SDG8 - productivity. The health-related goals of the immunization system are expressed by SDG3.2 (End preventable deaths of newborns and children < 5 years of age), SDG3.3 (End epidemics of AIDS, TB, Malaria, Neglected Tropical Diseases (NTDs) and combat other communicable diseases), SDG3.8 (Universal Health Coverage (UHC)) and SDG 3.d (International Health Regulations (IHR) and increasing resilience to shocks). Immunization program outcomes are measured by immunization coverage levels and equity of immunization with respect to all vaccines in the national schedule, elimination of epidemic-prone diseases such as measles, mumps and rubella, eradication of polio, number of Human Immunodeficiency Virus (HIV) cases, new vaccines introduced against NTDs and other indicators from the Global Vaccine Action Plan (GVAP) [ 40 ] and National immunization programs [ 24 ].
Concerning SDG3.8 (UHC), the EPI programs are set up in order to immunize the target population in accordance with the GVAP targets, which propose 90% coverage rates at the national level for most vaccines, and 80% at the district level. Herd immunity, the level of immunization coverage in a population at which the chain of disease transmission is broken, is attained in most cases at around 90% immunization coverage rate (95% for measles), requiring Universal Health Coverage (UHC) and aiming at reducing under-five mortality and avoiding epidemics as stipulated by SDG3. However, it must be noted that even when national and district level GVAP targets are met, outbreaks can still occur due to under-immunization at the community level. The prevention of emerging infectious diseases (SDG3.d) is mainly focused on the development of new vaccines, and more specifically on preparing against an epidemic of disease ‘X’, for instance by the Coalition of Epidemic Preparedness Innovations (CEPI [ 41 ]).
Next to the direct goal of immunization, SDG3, the contribution to boosting the productivity of the population and economic development (SDG8) is highlighted, as a healthy workforce is critical for economic development [ 2 , 26 ], which is undoubtedly undermined in case of epidemics.
On the level of households and individuals, avoiding Vaccine-Preventable Diseases (VPD) cases saves people from income loss and out-of-pocket health expenses (SDG1). In addition to malnutrition following from poverty, VPDs can lead to weakened children not taking up nutrients (SDG2), for instance in the case of cholera.
Impact of providing access to immunization services for all
The universal access to vaccination services boosts equality (SDG5 and SDG10) and provides health education to caregivers (SDG4) together with its synergetic effects with zero hunger (SDG2), quality education (SDG4), clean water (SDG6), and climate action (SDG13) [ 3 , 13 , 29 ]. Furthermore, immunization’s contribution to building a productive workforce (SDG8) turns it into a core driver of country development [ 2 , 26 ]. While endemic diseases by far represent the most significant burden of disease, the increasing number of outbreaks of emerging infectious diseases poses a major international concern as epidemics may rapidly spread, or even turn into a pandemic, and cause massive health, economic and emotional damage [ 42 ], illustrated by the Covid-19 pandemic.
Impact of creating an environment for health system development
Creating an environment that is beneficial for health system development is anything but trivial. Several elements from the literature can shape this pathway. First and foremost, there is the provision of resources to build capacity for immunization service delivery, disease surveillance, and early diagnosis. This last mile capacity building is further enhanced by strengthening national and regional public health systems. In this capacity building efforts, public-private partnership plays a central role. The latter accounts both for the vaccine production [ 33 ] as well as for partnership incentives for the delivery of integrated services [ 32 , 43 ], including in conflict settings where, for example, the implementation of the EPI program was found to create a “working encounter” with state and non-state actors in Myanmar which led to positive development and peacebuilding outcomes [ 30 , 31 , 35 ].
Indirect impact on the SDGs
In addition to SDGs that are directly impacted by immunization through the three pathways discussed above, a number of synergetic effects exist between SDG-promoting actions, such as access to clean water (SDG6) as a complementary factor to immunization in the prevention of cholera and adequate nutrition (SDG2), which improves the immune response triggered by immunization [ 3 , 39 ]. These indirect and synergetic effects are indicated in blue in Fig. 2 . Moreover, the emergence and prevalence of infectious diseases is often found to be related to environmental health and animal health conditions represented by SDG13, SDG14, and SDG15 and approached as Planetary Health [ 8 , 12 , 44 ]. Table 5 shows an overview of hurdles and strategies, identified from the Cat1 papers, in taking these synergetic and indirect effects of immunization on the SDGs into account.
Immunization system sustainability challenges
Immunization can only have a lasting impact on the SDGs in LMICs when immunization programs are intrinsically sustainable. Challenges observed concern the sustainability of the health outcomes reached [ 13 ], the difficulty of increasing SSA coverage levels over and above 85%, the important subnational under-immunization, and the reduced coverage rate of childhood immunization as a result of the COVID-19 pandemic [ 24 ]. Challenges for SDG3.3 are the delay in polio eradication and backward evolution in the elimination of TB, measles, and malaria, and the need for vaccine development for several NTDs such as Nipah Virus Infection and Lassa Fever, among others. In brief, at the current pace and based on the current strategies, it is expected that only SDG3.2 is likely to be achieved in SSA by 2030 [ 13 ]. Furthermore, the mechanisms that trigger epidemics and the emergence of infectious diseases related to the loss of biodiversity and climate change retrieved from the Cat1 papers will, even more, aggravate the risk of infectious diseases. In order to achieve sustainable protection against both endemic and Emerging Infectious Diseases (EIDs), there is a need for more focus on the resilience of the immunization system, than on the performance in an equilibrium state [ 58 ].
The Cat2 papers, as described in Table 3 , provide an overview of the challenges to the sustainable performance and continuation of immunization in LMICs. We found 104 papers raising issues endogenous to the national health system, 111 papers discussed topics beyond the national health system, and 9 papers dealing with issues covering both areas and counted in both, summarized in Fig. 3 .
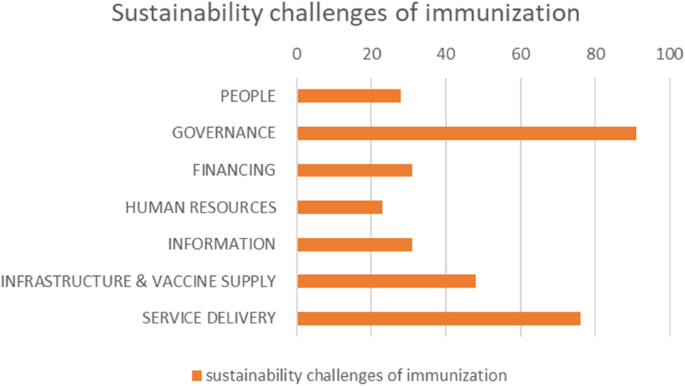
Sustainability challenges papers. Distribution of included papers, dealing with sustainability challenges of immunization in LMICs, categorized according to the WHO Health System building blocks [ 11 ]
Sustainability challenges discussed in the papers were connected to the human-centered health system building blocks as defined by the WHO [ 11 ]: People, Governance, Financing, Human resources, Information, Medicines & Technology , and Service Delivery . These are visually represented in Fig. 4 , together with some selected, key illustrative sustainability challenges, derived from the extensive overview listed in Table 6 .

WHO Health System building blocks. Selected key sustainability challenges from the reviewed literature, according to the WHO Health System building blocks
Health system building-blocks
As an inherent feature of a complex system, the challenges discussed are often part of several building blocks. In our categorization, we opted for the dominating building block. The referenced papers, organized according to the respective building blocks, are summarized in Table 6 .
Although the acknowledgment of patient-centeredness and human-centered design as an essential approach to supporting SDGs achievement has been globally confirmed, only a limited number of papers were found which explicitly discussed the challenges related to engaging and empowering people in order to achieve the SDGs or the related sustainability. While small in number (28 papers), these papers contain the main issues related to giving a voice to the “demand-side”: the target population for vaccination, or, more broadly, the individuals and communities that need protection from infectious diseases.
Other human factors that play in the supply side of vaccination, such as motivation of staff or decision making by national authorities, are either discussed under “Human resources” or “Governance.” Papers dealing with implementation challenges were categorized under “Service delivery.”
Even though nearly all papers refer to a specific geographical setting and context, generic challenges still emerged from them. First, the challenge of vaccine acceptance, which was declared by WHO as one of the ten greatest health threats to human health in 2019 [ 71 ], leads to unsustainable immunization coverage and puts a significant burden on disease elimination programs [ 72 ]. Vaccine acceptance is also an essential condition for a successful new vaccine introduction [ 74 ]. In the course of countering the current Covid19 pandemic, vaccine hesitancy in all its aspects became a considerable roadblock for immunization success [ 249 ]. Experiences with Human Papilloma Virus (HPV) introduction in Uganda, Rwanda, and Bhutan underlined the basic conditions of correct information to the population, strong political commitment, and local involvement [ 75 ]. Nevertheless, remaining cultural barriers require anthropologic research before implementation [ 70 ].
Second, a strong community engagement is required for any type of social mobilization during vaccination campaigns or routine immunization in order to create access to immunization for all. Engagement is based on connecting with the relevant community-level stakeholders and offering successful incentives. Stakeholders are traditional leaders, community health committees, and health providers, such as community health workers or “village doctors” [ 80 , 81 ] Incentives are relevant when behavioral change is required for a sustainable solution. Cases of traditional nursing habits conflicting with medical insights regarding infectious disease prevention were discussed, like birth habits impacting early life bacterial exposures [ 89 ]. Further research is needed to understand the role of Community Health Workers (CHWs) in reaching the SDGs. To recover from measles resurgence after the COVID-19 pandemic, community engagement for tailored solutions must be considered [ 79 ].
Third, the challenge of universal immunization to overcome the inequality (SDG10) resulting from the socio-economic determinants of health, such as poverty and education (SDGs1–6), requires the provision of access to immunization for all [ 26 , 91 , 93 ]. Tied by the Environment – Economy – Health nexus [ 57 ], vicious cycles of poverty need to be broken since they lead to greater vulnerability for infectious diseases and NTDs as well as to poor access to healthcare services [ 23 ].
The Governance building-block houses decision-making entities and frameworks related to immunization target-setting, policy decision-making, and resource allocation. Moreover, the sustainability challenges found in the literature call for improved decision support based on fine-grained data and system-wide long-term models that connect interventions with SDG-level outcomes [ 95 , 96 , 103 ]. At the global level, it includes the immunization targets and strategies in preventing epidemic disease prevalence and outbreaks, in the broader context of Planetary Health. In addition, sustainability challenges were detected in measuring health systems’ strength for comparison between countries [ 95 ] and health systems resilience in defining and measuring performance indicators towards reaching Grand Convergence , and towards coping with the emerging Double burden of disease (the latter being the rise of non-communicable diseases in LMICs as they converge with infectious diseases as main causes of death) [ 13 , 97 , 98 , 99 ]. At the national level, it concerns the country-specific priority setting and transformation path of health prevention and promotion as a driver for sustainable development.
A major fraction of governance-related challenges expresses the need to capture the complexity, context, and long-term perspective of the health system using systems thinking [ 14 , 103 , 104 ]. This is reflected in the quest for system-wide impact analysis in order to model health outcomes that result from interventions to the health system and ensuring program sustainability. Examples include the effect of changing vaccine doses per vial and vaccine thermostability [ 105 , 106 ].
Similarly, political commitment (SDG16) is needed to support programs for which a direct effect is difficult to link with health outcomes, which is often the case for Health System Strengthening (HSS) programs and to synergistically integrate vertical disease-specific programs into horizontal HSS programs [ 21 , 90 ]. Systems thinking is proposed as a stepping stone to dynamic modeling. Long-term system models, which reach for the 2030 SDGs and beyond, are able to show dynamic effects resulting from adaptation, such as the role of vaccines to reduce anti-microbial resistance [ 62 ], and unintended consequences, such as the behavioral reaction following mandatory immunizations [ 102 ].
Following SDG3.2, a central governance element is the continuous update of the national immunization plan and the sustainability of the Expanded Program on Immunization by taking up new vaccines and deciding on the coverage target. Challenges discussed in the papers mention that the evidence-based decision support and cost-effectiveness studies brought to the National Immunization Technical Advisory Group (NITAG), often lack the sustainability dimension and long-term or indirect effects [ 76 , 109 , 110 , 112 , 113 , 114 ]. Based on these approaches, decisions on whether or not to adopt a vaccine are made without considering the full impact of the additional vaccine on the total vaccine supply chain and on the country’s epidemiology, which is impacted by all vaccines compiled in the national plan. Furthermore, the full public health value of vaccination should be measured on the population level, not only on the individual level, while taking into account the impact of non-medical elements and different SDGs, such as infrastructure works in combination with a vaccine against cholera or malaria [ 22 , 111 ]. Finally, even when the local burden of disease data are not available, the NITAG needs scientifically sound decision support that captures the complex adaptive nature of the health system.
Aiming at disease elimination and polio eradication initiatives, the global coordination and national commitment to the vertical programs are of crucial importance since the last remaining disease case must be identified, and continued universal vaccination coverage is required. At the same time, disease cases are dwindling in the endgame, but disease dynamics urge for counter-intuitive strategies while the government’s commitment to the program is at risk of fading. Decision-supporting models that capture both the epidemiological dynamics and the country’s contextual landscape are needed [ 59 , 116 , 250 ].
Reported challenges for decision support related to UHC and equity (SDG3.8 and 3.b) were the scarcity of disaggregated data, defining differentiated approaches and strategies tailored to reach the unreached. Under-immunized populations often find themselves in humanitarian settings where case-specific immunization interventions are needed or where underlying determinants of immunization, related to other SDGs, need further investigation [ 21 , 117 , 118 , 119 , 120 , 121 , 122 , 123 ].
In supporting the WHO’s Integrated People-Centered Health Services (IPCHS) strategy “Engaging and empowering people,” appropriate processes are needed to support decentralized decision making, enabling self-organized local solutions, and building resilience [ 109 , 127 , 128 , 129 , 130 ]. In the case of local decision-making for enhanced EPI performance, it has been found that three conditions should be fulfilled: availability of data, understanding of the complexities in the system, and availability of decision power at the operational level [ 126 ]. Looking from the global perspective, one views self-organized local solutions as country-specific development paths to health outcomes, possibly grounded in the upscaling of proven best practices in each country [ 13 ].
In building resilience and preparedness towards disruptive events, challenges were reported regarding the relevance of cost-effectiveness-oriented optimization models for humanitarian operations and the need for incorporation in the health system of small-scale people-centered initiatives [ 132 , 133 , 134 ]. Adaptive behavior in a post-Ebola epidemics era gave rise to transformation strategies that need to be further implemented [ 135 ]. And of course, currently, the Covid19 pandemic showed the high need for resilient health systems in general and immunization systems in particular. It proved in a dramatic way that unpreparedness pays back not only health (SDG3) but impacts almost all SDG as mentioned earlier in our Background section.
Collaboration (SDG17) and coordination of cross-sectoral activities, between public and private partners or between nations, are needed to tackle vector-borne diseases and aim for disease eradication, integrate nutrition into the health system, foster sustainable innovation initiatives, strengthen weaker systems through regional collaboration, or apply health diplomacy to connect economic, social, and political sectors [ 43 , 54 , 82 , 138 , 139 , 140 , 141 , 143 ]. Understanding the interactions of these private or cross-sectoral initiatives with the health system is key. Global future-oriented health governance (SDG16) demands alignment in priorities stemming from IHR and SDGs, consultation of the global health community, understanding the relationship between health and behavior, and the role of regulation in supporting global health, as exemplified by the response to the Zika epidemic [ 142 ], or on a more permanent basis, the need for global support of synergies between horizontal and vertical programs. Global health diplomacy is proposed to avoid violation of IHR, for instance in the case of the COVID-19 pandemic [ 125 ].
In the context of LMIC immunization, the term “sustainability” is almost always used implicitly for “financial sustainability”. Clearly, every resource employed for immunization needs to be financed and, although the return on investment of immunization is estimated to be substantial, the funds are not available to LMIC governments to make the investments without external support. Challenges reported relate to donor dependency [ 76 , 107 , 108 , 145 , 147 , 148 , 149 , 150 , 151 , 152 , 251 ], finding the budget from domestic sources [ 108 , 124 , 146 , 148 , 156 , 161 , 162 , 163 , 164 ], and increased efficiency in service delivery. From the global perspective, both the transition out of GAVI support as well as the aftermath of political instability are recognized as critical milestones in the development paths of LMICs [ 154 , 155 , 156 , 157 , 158 , 159 ].
Human resources
Challenges in Human Resources were related to building capacity, accountability, and resilience. Capacity building to strengthen the scarce African healthcare human capital is needed on the level of capacity in leadership and governance, technical healthcare and supply chain skills, and in cross-sectoral disciplines in the framework of Planetary Health approaches [ 13 , 46 , 99 , 163 , 165 , 167 , 168 , 170 , 252 ]. Training programs should make a stronger link with health outcomes (SDG3) and other relevant SDGs encountered in the Planetary Health paradigm. Further challenges lie in rolling out training programs for vast numbers of local health workers and community health workers while ensuring the continuity of operations. Furthermore, synergies are expected from standardization in certificates and training programs across organizations and countries.
In the quest to obtain accountability of staff, the challenge of including health outcomes, such as under-five mortality (SDG3), in evaluation frameworks is discussed. An all-but straightforward endeavor due to the delayed effect of functioning and outcomes, and the multitude of actors in the system that play a role. Equally delicate are the challenges of installing effective and fair incentives for health care staff, without triggering unintended or unsustainable effects [ 166 , 174 , 175 , 176 ].
A key element for health system resilience is achieved by workforce commitment and absorptive capacity, to avoid immunization service disruptions due to health workers’ frustration and subsequent strikes [ 174 ]. Therefore, an appropriate level of empowerment is needed to allow decentralized decision-making. Equally important is a balanced workload that provides buffering, and a safe environment in times of disease outbreaks involving personal risks such as during the Ebola outbreaks [ 172 ].
Information
Based on a review study by Kumar, routine Health Information Systems in LMICs are not utilizing their full potential of supporting the health-related SDGs (SDG3) due to Health Information System design barriers that lead to poor data quality and data use [ 177 ]. Specifically, the authors argue that user-related factors are not sufficiently embedded in the Health Information System design and propose a systems-thinking approach to cope with the Health Information System design-user reality gap [ 179 , 180 , 181 ]. An earlier study in Uganda pointed to the lack of standardization and strategic alignment between the health vision and the information system, on top of user-related engagement issues [ 178 ]. A principal concern in LMICs remains the considerable effort and risks involved in the transition from paper-based to electronic health registries and databases, and the consequences for improved performance in Maternal and Child Health, the cornerstone of national immunization programs. On the other hand, the availability of mobile technology has led to a proliferation of health apps resulting in 40.000 mobile health apps and hundreds of communication platforms while collaboration between health providers and the adoption of technology still experience high barriers [ 13 ].
Classified according to the twelve common applications to overcome UHC in Maternal and Child Health and the mHealth roadmap for UHC, a number of challenges for immunization were found [ 13 , 93 , 171 , 184 , 185 , 186 , 188 , 189 , 190 , 253 ]. First, immunization and surveillance data collection and reporting involve identifying immunization inequity and triggering the need for enhanced interventions through immunization dashboards, such as District Health Information Software 2 also known as DHIS2. Good practices and Artificial Intelligence (AI) applications from disease-specific programs focusing on Meningitis A, Polio, and disease outbreaks in humanitarian operations, have paved the way for high-standard disease surveillance. The implementation of electronic health records is challenged with contextual factors such as power outages and usability factors. On the data usage side, electronic decision support in the form of burden of disease data to the NITAG, diagnostics tools for comorbidities of infectious diseases and non-infectious diseases, and local determinants of vaccination to drive service delivery planning are reported to be lacking. It has been found that immunization information can positively impact trust in vaccination on individual and community levels, one of the important sustainability factors. However, the information systems need to be further strengthened at this point. Health providers’ collaboration could be supported more adequately by regional and global data exchange systems and support systems for decentral decision making. In addition, provider training formats can enhance efficiency and resilience in service delivery, provided they are well accepted by the health providers and are not regarded as a threat to their expertise and value. Finally, Health Information Systems in LMICs are underutilized for supply chain management, hence the combination of the Health Information System and the Logistics Management Information System bears great potential.
Medicines and technology
On the level of medicines and technology, challenges in vaccine distribution are found in reaching and maintaining a sufficient level of effectiveness and efficiency in vaccine distribution and delivery, under increasingly stringent conditions resulting from population growth and the growing number of vaccines to be administered per person [ 13 , 19 , 76 , 107 , 163 , 168 , 192 , 193 , 194 , 195 , 198 , 199 , 254 ]. Supply chain strengthening efforts to avoid out-of-stocks and to increase immunization equity experience difficulties in getting adopted beyond demonstration projects. In addition, they experience difficulties in relating to the real-life context of available data, human resources, and existing infrastructure at the lower levels of the supply chain. In specific, the introduction of new vaccines needs to be carefully considered on its full benefits and long-term sustainability, including the phase of implementation and impact on the existing immunization. A critical part of the immunization infrastructure concerns the cold chain equipment where the following sustainability challenges were detected: (i) performance of cold chain equipment ensuring the potency of the vaccines (SDG3), (ii) emissions, (iii) energy and material used during production, (iv) use, and (v) post-use stages of the cold chain equipment (SDG7, SDG13, and SDG15) depending on cooling technology applied and maintenance efforts. Future directions are the integration of vaccines with other medicines, redesign for efficiency and effectiveness, and elimination of the cold chain when vaccines would become thermostable.
Availability of vaccines to LMICs for routine or emergency situations has been troubled - on top of financing-related issues discussed earlier - by disruptions, e.g., BCG in 2014–2015 [ 201 ]. This calls for improved alignment and collaboration between immunization partners, in line with SDG17, to tackle global health risks. Similar needs occur for vaccine stockpiles against epidemic-prone diseases, which are needed even after the eradication of the disease [ 202 ]. In addition, advancements to intellectual property frameworks and optimization of regulatory pathways that can lead to a significant reduction of registration time for new vaccines for LMICs are desperately needed in order to reach UHC (SDG3) [ 203 ]. In the same context, the development and viability of domestic vaccine production appear to face a high barrier that will not be easily overcome, particularly in SSA [ 204 , 205 , 206 , 207 , 208 , 209 ]. Not only technological development but also trust in domestic vaccines needs to be ensured [ 33 , 211 ].
New vaccine development presents a range of challenges [ 13 , 97 , 106 , 111 , 164 , 212 , 213 , 214 , 215 , 216 , 217 , 218 , 219 , 220 ]2. First, being prepared with a vaccine to prevent outbreaks from turning into large epidemics or pandemics (SDG3.d) requires seizing the momentum for vaccine development as soon as signs of pathogenic emergence appear. However, in reality, this proved to be difficult for many reasons, not in the least due to the engagement and priority setting that needs to be set by political, scientific, and funding partners into a working coalition. Next to diseases related to visible epidemics, there is an ongoing need for vaccines against a range of endemic infectious diseases that cause a large burden of disease in LMICs amongst the most vulnerable in the population (SDG3 and SDG10), including malaria, NTDs, and HIV. Future-oriented priority setting for vaccine development, in the light of the Grand Convergence, local epidemiological needs, full public health value, and alignment with the SDGs, results in a complex decision problem. In order to safeguard the vaccine’s potency and sustainable immune response in LMICs, vaccine delivery innovations in technology or vaccination schedules are potential candidates for improvement, provided that their impact under real circumstances in LMICs can be investigated safely.
Service delivery
The building block of Service Delivery covers the tactical and operational roll-out of the programs and interventions approved and supported by Governance , making use of the available resources, and leading to the aspired Goals and Outcomes. As such, the sustainability challenges in immunization Service Delivery were grouped under the following three categories, reflecting the main goal related to the challenge: Equity, Continuity, and Resilience. Principles and methodologies from the fields of Systems Thinking, Implementation Research, and strategies from WHO’s Reaching Every District framework and IPCHS framework, were applied to operational research problems encountered in immunization service delivery. The following challenges to sustainability were noted:
Reaching equitable coverage (SDG3.2 and SDG3.8), with the aim to increase immunization above the 85% level at which it has been stagnating since 2013, is attempted by improving access through offering tailored solutions adapted to the local context. A first element that needs to be further explored is measuring vulnerability from different data sources and translating it into meaningful indicators to derive the need for immunization services, such as a fine-grained spatial vulnerability map based on a multi-dimensional poverty index, infection data, and environmental health data [ 67 , 117 , 118 , 229 , 230 ]. A second challenge concerns the design of tailored immunization delivery approaches to actually reach the under-reached, according to the accessibility of the area, population mobility, and immunization service needs [ 25 , 48 , 79 , 119 , 225 , 226 , 227 , 228 ]. This leads to often unique solutions regarding logistics or community engagement, which are effective in a specific context and which can be continuously improved when needed. Research papers, review papers as well as case-based research confirmed the relevance and need for an enabling environment to create tailored interventions, and to sustainably incorporate them into the health system, alongside standard interventions. A third research need lies in the configuration of an integrated delivery platform, which aims at improved people-centered care, without overstretching the health system [ 76 , 127 , 186 , 231 , 232 , 233 , 234 , 235 , 255 ]. Services, next to routine immunization, include nutrition, mass drug administration against NTDs, campaigns from vertical immunization programs that aim at very high coverage (Measles), or new vaccine introduction platforms. Later-age vaccinations (MMR2 Footnote 2 at 15 months) and adolescent school vaccinations (HPV Footnote 3 at 12 years) seem to reach lower coverage levels and are more costly. It is concluded that the design of the intervention and its implementation phase are equally important and should be considered in parallel.
Second, the continuity of immunization service delivery is challenged by the increased load on the immunization system resulting from the introduction of new vaccines and population growth [ 63 , 65 , 175 , 213 , 238 , 239 , 240 , 241 ]. Four types of challenges were found. First, the pressure is felt at the limits of resource-related health system building blocks: the supply of vaccines and commodities, the availability of human resources, the financing from domestic and external sources, and the availability of information. These challenges were discussed in the dedicated sections above. Second, demand-side continuity factors, already discussed under People -building-block, which include trust in vaccination and community engagement, are threatening continuity. Third, the cost-effectiveness of operations is mentioned to endanger continuity, in particular activities for defaulter tracing, outreach, and campaigns are in need of more cost-efficient alternatives. Fourth, the sustainability of the vaccine-induced immune response must be well understood in order to plan Supplemental Immunization Activities (SIA) when needed. In addition, the surveillance of vaccine safety and adverse reactions to vaccination needs to be supported in the LMICs and must be preserved after GAVI transition. Coordination of critical immunization services, such as the implementation of switching vaccine presentations for polio eradication and rolling out SIA campaigns, add to the complexity of service delivery.
Third, resilience challenges were found in the phases of preparedness, response, and recovery in acute humanitarian emergencies [ 100 , 172 , 242 , 243 , 244 , 245 , 246 , 247 , 256 ]. Preparedness is not restricted to the availability of vaccines. Equally important in times of epidemics or a pandemic is the availability of diagnostics. Experiences with preparedness for Ebola recommend mobile training for CHWs and the recognition that humanitarian organizations can contribute to developing weaker health systems in order to build resilience for acute emergencies. A number of challenges apply to the response phase, such as the competitive effect between immunization campaigns in response to disease outbreaks (e.g., meningitis A, Ebola) and routine immunization services or planned polio eradication activities. Furthermore, it was found that decision support tools for humanitarian transportation planning during emergencies should aim primarily at being implementable in acute crisis conditions, rather than aiming for optimal calculations at the expense of usability. Post-conflict and long-term conflict situations in Afghanistan and Syria showed the need for a differentiated approach to immunization to avoid dramatically low immunization coverage and loss of health gains or reemergence of conflict during the transition between emergency and development [ 133 , 248 ].
Model-based solutions to LMIC immunization sustainability challenges
Going beyond the observations of the described immunization system sustainability challenges in literature, we analyzed a third category of papers, offering model-based approaches to resolve the challenges observed in contributing to the SDGs through immunization. We specifically filtered the literature on solution approaches that comply with the inclusion criteria defined in the Methods section, and which are expected to be customizable to different LMICs and settings for re-use.
In contrast to the previous subsection, the solution approaches are classified by use of a different framework that reflects the most relevant immunization priorities in immunization for the next decade: the seven Strategic Priorities (SPs) of the WHO Immunization Agenda 2030 [ 2 ].
Based on the inclusion criteria, a total of 47 papers with models were identified, spread across the strategic priorities, as shown in Fig. 5 . The main contributors were Duintjer Tebbens and Thompson [ 59 , 116 , 202 , 250 , 257 , 258 , 259 , 260 , 261 , 262 ], who published several papers with research mainly dedicated to polio eradication strategies and vaccine stockpiling, and Rwashana [ 263 , 264 , 265 , 266 ] focusing on the dynamics of the Ugandese immunization system. Compared to the entire set of papers, the purpose of the identified papers was to (i) provide the stakeholders with insight into the system’s complex behavior, (ii) deliver evidence-based decision support, (iii) demonstrate a re-usable best-practice approach, or (iv) to assess the impact of existing WHO guidelines. Methods applied in these papers include a majority of quantitative modeling approaches next to a limited number of qualitative modeling papers and papers demonstrating projects without modeling. The majority of quantitative models are based on system dynamics (SD), followed by agent-based models (ABM), analytical models, and hybrid models (the ones listed above combined with other methods such as Geographical Information System (GIS)-based spatial modeling and statistical models). The majority of qualitative models are constructed around causal-loop diagrams (CLDs), while the remaining papers apply a range of different techniques. Now we turn to a content-focused analysis of the model-based solution papers with respect to immunization sustainability.
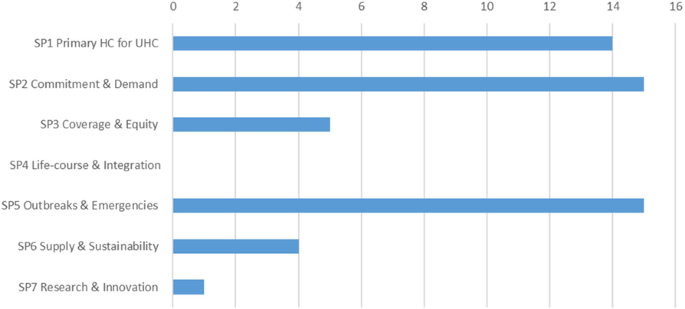
Strategic Priorities. Amount of papers with model-based solutions to Immunization system challenges classified according to the Strategic Priorities (SPs) of Immunization Agenda 2030 (version April 2020)
In support of SP1, immunization programs for Primary Health Care and Universal Health Coverage, through vaccine supply chain strengthening, Lennon et al. [ 193 ] provide a generic approach for root cause analysis and institutional learning for maintenance of refrigerators, using temperature monitoring technology. Besides sustainably improved reach and efficiency of immunization programs in LMICs, local employment and ownership are positively affected, and lower emissions are expected. Through the development of high-level CLDs and System Dynamics (SD) models, Rwashana et al. [ 263 , 264 , 265 , 266 ] identified country-specific impacting factors, both from the supply side and the demand side, on immunization coverage and neonatal mortality in Uganda, applicable for policy design at the national level. Recently, a modeling framework for decision tools for vaccine development, aiming at universal availability has been presented [ 267 ]. Furthermore, a decision-support platform for vaccine prioritization has been put forward, for use by NITAG, including financial and other dimensions [ 268 ].
Concerning the health workforce, the recurring questions of the sustainability of performance-based financing (PBF) and the causal link between immunization coverage and PBF as a financial incentive for the immunization personnel in the health facilities were approached by qualitative systems methods by different authors. Renmans et al. [ 269 ] applied both systems’ archetypes and theory-driven hypotheses in an intervention study in Uganda, whereby the CLDs increased transparency in the complexity of interactions. Another intervention study by Alonge et al. [ 270 ] in Afghanistan resulted in a system dynamics model, while the research by Sato and Belel [ 271 ] in Nigeria was based on statistical analysis. The sustainable effect of performance-based financing on the immunization rate appeared to depend on the specific context at hand, and PBF was found to be overshadowed by the financing of the polio eradication program. This leads us to the challenge of synergistically implementing vertical disease-specific programs to contribute to HSS at the point of service delivery, which was tackled by Doherty et al. [ 152 ] by relying on qualitative appraisal methods and by Utazi et al. [ 272 ] by applying geospatial statistical modeling. On the global scale, coordination of polio eradication was supported by the System Dynamics (SD) models of Thomson et al. [ 257 , 258 , 259 ], which translate the intricate transmission and adaptation mechanisms of poliovirus into clear support for policymaking. As a final element in SP1, a demonstration project of a cloud-based disease surveillance system for meningitis in Burkina Faso was evaluated by Diallo et al. [ 185 ] and the sustainability of the vaccine-induced immune response for pneumococcal disease in Kenya was monitored by Ojal et al. [ 65 ] using an extended susceptible-infectious-recovered (SIR) epidemiologic model.
SP2 revolves around Commitment and Demand, referring to the continued engagement of the providers of immunization services and the beneficiaries, respectively. Commitment is supported by strengthening evidence-based decision-making with modeling tools capable of showing the long-term health impact of disease control through vaccination uptake and disease elimination and eradication through intensified vaccination strategies. In their paper, Kivuti-Bitok et al. [ 273 ] developed an SD model to support policy-making for HPV vaccination and screening in Kenya. The model runs over a time horizon up to 2050 and was designed to evolve when new information becomes available. In two of their papers on polio eradication, Duintjer Tebbens and Thompson [ 59 , 250 ] focus on assisting policymaking from a long-term perspective and on acknowledging the counter-intuitive nature of the strategies proposed. Aimed at sustainably striving for UHC based on tailored solutions and empowering the district level to fulfill its role in this, Tetui et al. [ 274 ] propose an approach based on participatory action research to strengthening district health managers’ leadership capacity, as an improvement to non-participatory approaches. A comparable approach based on sense-making and discretionary power was found to sustainably support policy implementation at the Primary Health Center level in South Africa [ 275 ].
The demand for immunization relies heavily on creating sustainable public trust and vaccination confidence at the community level. To this end, Gilmore et al. [ 83 ] provided an approach based on realist evaluation to recognize the role and to support the engagement of the community health committee as a crucial stakeholder in the community-level immunization system. Sarriot et al. [ 276 ] derived a CLD for Rwanda’s integrated case management, revealing both organizational factors and context-dependent cultural motivational factors playing at national, district, and community levels in the system. In this way, they succeed in framing the role of performance-based financing in relation to political stability, sub-national program management, and utilization of services at the community level. Varghese et al. [ 277 ] also applied CLDs, among other methods applicable to complex adaptive systems, to reveal the basic triggers that led to stagnating vaccine acceptance in Kerala (India), resulting in dangerously low immunization coverage rates in certain districts. CLDs were also applied by Ozawa et al. [ 278 ] to explore pathways that lead to trust-building in vaccination. Through scenario analysis and mapping of health system experiences, communication, and social capital, reinforcing mechanisms and spill-over effects of distrust and the disruptive impact of the 2014 Ebola outbreak were revealed. A mathematical modeling approach in a non-LMIC context (US) was taken by Pananos et al. [ 279 ], who developed a measles outbreak prediction model based on immunization coverage and trust levels derived from social media. The approach is likely to be transferrable to LMICs. In order to activate people and communities from accepting vaccines to changing their health-related behavior Kumar et al. [ 89 ] show a community-centric design approach applied to India that aims at closing the evidence-practice gap and sustainably improving health impact. Sarriot et al. [ 280 ] investigated community learning of sustainability evaluation in a Northern Bangladesh urban health system.
Utazi et al. [ 272 , 281 ] pursued SP3, Coverage and Equity, by visualizing the under-immunized population on high-resolution age-structured geographical maps, using open source data, in order to reveal inequities in vaccination coverage. This information is applicable to guide geographical prioritization and immunization strategy design for increased equity. The implementation of a sustainable immunization service delivery based on local solutions, tailored to local needs, was investigated in Ethiopia by Manyazewal [ 227 ] using a continuous quality improvement approach. Duintjer Tebbens et al. [ 115 , 116 ] applied SD modeling to show the effect of polio under-vaccination on the immune response in populations of Pakistan and Afghanistan, thereby offering evidence for policymaking.
Except for the papers that provided decision support for the introduction of school-based HPV immunization targeting adolescents, no papers could be included, considering the inclusion criteria that were dedicated to supporting the delivery of SP4, Life-course and integration.
In the light of SP5, Outbreaks and Emergencies, two clusters of research resort [ 1 ]: anticipation and response to infectious disease outbreaks and [ 2 ] immunization during humanitarian crises.
First, related to anticipation and response, the prediction of disease outbreaks was tackled by Jaafar et al. [ 282 ] and Knerer et al. [ 283 ]. The authors present SD models to predict dengue outbreaks, in Malaysia and Thailand, respectively, and to evaluate combined vector-control and vaccination strategies taking into account weather conditions. In a cluster of papers, a vaccine stockpile design against a post-eradication polio outbreak was modeled by Duintjer Tebbens et al. [ 202 ] using an SD model. Later, a general vaccine stockpile design framework was proposed by Thompson et al. [ 260 ]. SD was also applied by Kalkowska et al. [ 262 ] to model polio immunity in northern Indian populations. To support outbreak response vaccination strategies during epidemics, Grais et al. [ 284 ] applied ABM to the 2003–2004 measles outbreak in Niamey. They concluded that early vaccination, and targeting a wider age range, has a larger effect with respect to managing the epidemic than putting effort and time in reaching a higher vaccination coverage in a specific age group. A similar conclusion was reached by Duijzer et al. [ 285 ] using an analytical model based on a generic case of an epidemic. In the aftermath of the 2009 H1N1 pandemic, model-based public health strategies for pandemic preparedness were investigated by Araz [ 286 ] using an SD model that considers vaccination, antiviral treatment, and non-medical interventions such as school closures. The economic impact and epidemic dynamics were evaluated on multiple criteria using Analytic Hierarchy Process along with different intervention strategies. Grefenstette et al. [ 287 ] applied ABM to census data in order to provide decision support to local authorities during epidemics. Learnings and data from the 2016 yellow fever epidemic in Angola led to the development of an adaptive vaccination strategy for Kinshasa, anticipating vaccine shortages, based on fractional dosing [ 288 ]. The 2014 outbreak in West Africa, the largest Ebola outbreak in history, exposed a painful need for a vaccine for this NTD and more adequate intervention policies. Based on data from Liberia, additional insights on missing data and human behavior during the epidemic, Pruyt et al. [ 289 ] and Auping et al. [ 290 ] developed SD models that are able to show the effect of different pro-active and reactive strategies based on available measures, such as quarantine, and -at the time- future measures, such as a vaccine. In a separate model, the authors investigate the effect of fear on health-seeking behavior and the effect of interventions on epidemic control.
Second, to support vaccination during humanitarian emergencies, research on implementable planning tools for humanitarian organizations by Gralla et al. [ 246 ] developed recommendations and concluded that heuristics-based approaches have a higher chance of being actually used compared to more complicated optimization approaches. A multi-sectoral perspective on the relations between extreme-weather-driven disasters, such as floods or droughts, and children’s health is mapped by Garcia and Sheehan [ 291 ] into a CLD which succeeds in providing an insightful overview of, on the one hand, risk factors (ecosystem and individual physical and mental health factors), and on the other hand, resilience factors (climate mitigation measures, health services, and individual coping factors). This research implies that reducing vulnerability and building individual child resilience is crucial, as immunity to VPDs under extreme-weather-driven disasters is often jeopardized.
To enable sustainable success for the immunization program, SP6 on Supply and Sustainability strives for a continued commitment to immunization materialized in vaccine supply and financial sustainability. The importance of safeguarding a national budget for health prevention and the vulnerability related to donor dependency was shown by the models of Bishai et al. [ 292 ] and Doherty et al. [ 152 ], respectively. However, broader and long-term planning models that cover multiple sectors related to different SDGs are required to design policies that encompass the EEH nexus. Similarly, these policies need to ensure fiscal sustainability needed to provide adequate health and immunization budgets.
The final strategic priority, SP7, covers Research & Innovation. A multitude of technical research papers was found, based on the search strategy, dedicated to innovations in vaccine cold chain technology, information technology, and vaccine delivery innovations. However, only the cloud-based surveillance demonstration project by Diallo et al. [ 185 ] contained a reusable demonstration project that sufficiently addressed the contributions to the SDGs, that involved human-related factors and that was context-relevant in order to be included.
In this Discussion section, we first examine the remaining hurdles in reaching the SDGs through immunization, along the lines and strategic priorities of the Immunization Agenda 2030. Second, we focus on hurdles specifically dealing with immunization sustainability, including the aspect of resilience and touching the current pandemic context. Third, we formulate some recommendations for future research.
Remaining hurdles in reaching the SDGs through immunization
Figure 5 in the Results shows large literature coverage differences across the SPs. These differences are as much a reflection of the magnitude of the topics behind the SPs as it is reflecting the historic emphasis on these SPs.
Indeed, as SP1 and SP2 jointly comprise the basis of the entire immunization system, including all of the systems building blocks, by bringing them together under two strategic priorities, de facto more focus is put on their functioning as a whole towards sustainable health outcomes instead of optimizing isolated subsystems. The model-based approaches that were found within this respect show promising approaches mainly based on CLDs and SD models. In addition, where SP1 represents the organization of the supply side of the immunization system as a human-made system, SP2 concerns leadership, decision making, and engagement from both the supply as well as the demand side. Moreover, the result of all efforts depends on the immune response, which belongs to the broader natural, biological system. Modeling these different dimensions requires transdisciplinary approaches and adequate modeling techniques that can deal with highly nonlinear phenomena resulting from feedback loops and delays. CLDs and SD models were found to be successful in this endeavor. A combination of systems thinking and implementation science can be put forward to accelerate universal access to vaccines for all children in Africa, even in the Covid19 situation [ 20 ]. In a related way, implementation design and intervention design are combined through a socio-ecological model of health, applied to routine immunization in Kyrgystan [ 293 ].
SP3, coverage and equity, gained more attention in recent years as it became clear that inequitable subnational coverage led to stagnating immunization levels and below-target health outcomes in SSA. Understanding and intervening in local under-immunization often require tailored approaches that combine context-specific vulnerability and limited access to immunization. Geographical information and spatial models combined with implementation science and human-centered design were deployed here. Moreover, these factors are interconnected in the SDG context, and their root causes largely lie outside the health system. Therefore, this strategy needs further research support both from the public health and from the Planetary Health community, in order to deliver feasible solutions to actual and future inequity in immunization coverage and health.
SP4, concerning lifelong immunization, has been added very recently to the strategic priorities, as it assumes an already functioning immunization system in place, in which an individual’s immunization status can be monitored. The duration of the protective effect of immunization determines the immunization efforts needed, and only targeting children for vaccination proves to be insufficient for the lifelong protection of a population against certain VPDs. In order to evaluate the feasibility and sustainability of lifelong immunization, the impact on the entire health system, from targeting adults and the elderly through new immunization delivery platforms to the acceptance by the population, must be understood and weighed against health outcomes depending on country-specific epidemiology. Lessons learned from HPV school-based vaccination provide an initial insight and a starting point for further research. SP5, outbreaks and emergencies, received more implementable research results as this SP is located at the crossing of disease surveillance and outbreak response immunization as part of the national immunization system. At the same time, it also includes research dedicated to humanitarian operations during crises. With respect to the speed and visibility of outbreaks and epidemics, the models are often centered around a SIR logic and focus exclusively on managing the epidemic. The challenges referring to the ability of the health system to cope with the outbreak and to continue routine immunization services, i.e., the existing health system’s resilience, has not been thoroughly investigated. Its importance, however, has been underlined again during the current COVID-19 pandemic [ 294 ].
Remaining hurdles with respect to sustainability
The challenges that came out of the literature review correspond with the Immunization Agenda 2030’s strategic priorities and core values. Under-addressed challenges include public-private partnerships, the role of sustainable innovation, cross-sectoral collaboration, and service coordination. In addition, root causes of infectious disease threat and mechanisms leading to inequitable immunization demand and access discussed in the Results section, are not directly addressed by the Immunization Agenda 2030 SPs, but appear as root causes for SP3, SP5, and SP6. Based on our review process, we did not find model-based solutions in the literature that relate interventions to these root causes with immunization and the SDGs. However, especially in the light of the COVID-19 pandemic, the need for actionable and sustainable policies to reduce the risk of future disease emergence is without a doubt.
Figure 6 represents the different stages in the immunization system and indicates challenges (A – F) when it comes to the sustainability of immunization, the prerequisite for realizing the impact on the SDGs by 2030 and beyond.

Immunization sustainability hurdles
It is interesting to observe that successful vaccination service boils down to the synchronization of the three fundamental flows that meet at the vaccination service point: (A) the person to be vaccinated needs to have proper access to the vaccination service in a fair and equitable way, (B) the vaccine has to be availability under the required conditions as a consequence of well-designed and operationally effective vaccine supply policies, and (C) the presence of a professional health care worker, supported by a well-performing health system benefiting from the transdisciplinary synergies of cross-sectoral collaboration and partnerships. Even after a successful vaccination, the job is not finished. Efficient surveillance needs to be in place to assess the local effectiveness of vaccination (D) and to detect possible pathogen adaptation, leading the complex interactions with the epidemiological part of the planetary-health system, such as the fact that vaccines can lead to an adapted, vaccine-derived strain of the pathogen, e.g., Polio. Furthermore, impacting the three flow confluent point, is the need for more regional and local production in LMICs (E), a sustainable way to increase resilience when it comes to global availability and equity. Also impacting are the efforts to develop affordable, safe and effective vaccines (F) through the appropriate and collaborative R&D actions in the field of existing and emerging vaccine technology platforms combined with technological innovations across the immunization system.
Unfortunately obvious, all of these vaccination hurdles are currently illustrated by the current pandemic. We can refer to limited access to vaccination for individuals within country-wide mass vaccination campaigns, including demand-side factors such as vaccine hesitancy (A); overloaded health care systems leading to multiple capacity-related bottlenecks, including human resources (B); the global availability of vaccines, not meeting both the time and volume expectations (C); the emergence of several local Covid19 variants, showcasing the importance of surveillance of local vaccine effectiveness (D); the absence of local vaccine production in LMICs, painfully highlighting the effects of vaccine nationalism and vaccine diplomacy (E); and the increased awareness that preparedness needs to kick-off with R&D efforts, manufacturing scale-up and country readiness, long before the outbreak, as promoted by global initiatives like CEPI, COVAX, etc. (F). Needless to state that CEPI’s quest for preparedness against disease ‘X’, is more than supported by the Covid19 vaccine development efforts.
Recommendations for future research
One of the main future contributions of the academic community lies in supporting decision-making and operational management by giving insight into how immunization contributes to the SDGs, and by supporting the design and implementation of valuable interventions to improve its long-term performance towards achieving the SDGs. In line with the core values of the Immunization Agenda 2030 and the criteria for relevant research by Kovacs & Moshtari [ 9 ] and Besiou et al. [ 10 ], the following recommendations for future research were derived, also illustrated in Fig. 7 .
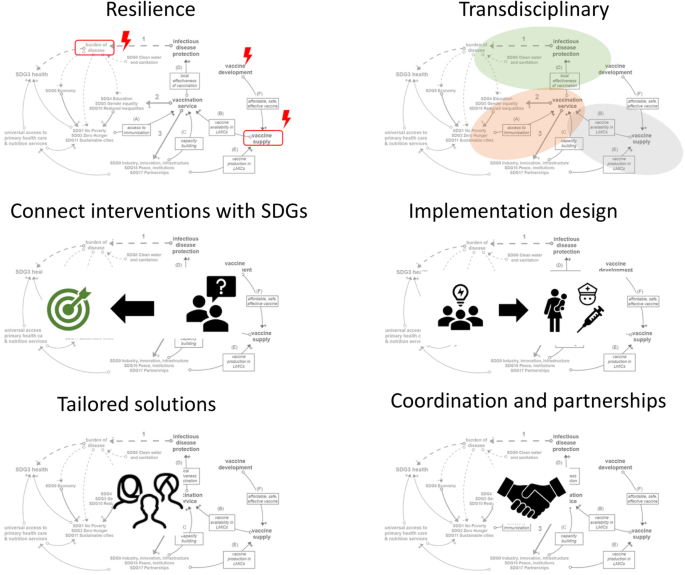
First, in order to be sustainable, research should support the transformation of the immunization system towards stronger resilience to respond to highly nonlinear demand patterns (e.g., caused by information delays, the onset of an outbreak), adaptation mechanisms (e.g., triggered by pathogens or human behavior) and phase shifts (e.g., from routine immunization regimes to emergency response situations and back). The inherent complexity stems from the position of immunization at the interface between the natural system (the immune system) and the human-made system (the immunization system), in which the natural system ultimately sets the rules and determines the health outcomes (SDG3). Furthermore, research and humanitarian operations should support the immunization system not only to respond to but also to anticipate adaptation and increasing stress faced by the system (e.g., induced by climate change) by building resilience in stable times in between disruptive events.
Second, a transdisciplinary approach relying on systems thinking and involving both STEM (science, technology, engineering, and math) and SHAPE (social sciences, humanities, and the arts for people and the economy) experts is recommended [ 295 ] to realistically model the dynamic behavior of the immunization system, to model human behavior, to validate models, to accommodate missing data without relying on unreliable assumptions [ 296 , 297 ]. This approach often includes epidemiology, human-centered design, spatial modeling using GIS, health economics, operations management, and operational research. There is a huge opportunity to activate existing research results that focused on a single subsystem, e.g., the vaccine supply chain, as pieces of information to build the comprehensive systems models that connect the subsystems. High-leverage interventions can be found at the interfaces between the subsystems.
Third, interventions should be explicitly connected to the SDGs they contribute to, with a sufficiently long time horizon, e.g., till 2030 and beyond. Interventions based on innovations should be equally sustainable. Therefore, the introduction of a new vaccine, refrigerator technology, or vaccination strategy should be measured by their impact on the SDG3-indicators and other SDGs such as Local employment (SDG8), Equity (SDG10), or Clean energy (SDG7) throughout their lifetime. In this way, the effect of the intervention on overall system performance is measured by its impact on the SDGs, and interventions leading to optimal modes of operation for only a subsystem (e.g., measured by vaccine supply chain efficiency) will be differentiated from overall optimal interventions (e.g., measured by under-five mortality, epidemic risk, equity, employment).
Fourth, the implementation design must be part of the intervention design, such that the intervention is people-centered, feasible, and adapted to the context it is intended for. The investigation of the complexity of introduction, usage, and maintenance, as well as the necessary infrastructure and skills for the intervention to work, avoids under-target outcomes from theoretically sound but infeasible interventions. For instance, human-centered design with clear stakeholder engagement is needed in order to design the type of health information system that can work in a specific community, district, or country where a specific infrastructure, leadership style, or immunization demand exists. This is in line with the five-step health system design approach of Decouttere et al. [ 298 ].
Fifth, the result could be that tailored solutions are proposed instead of generic ones in case of different needs for immunization or accessibility. In such cases, when “home-grown” solutions lead to higher engagement and resilience, they may outperform generic solutions, especially under strain conditions. Only a bottom-up research approach is able to reveal these. Therefore, research needs to investigate the appropriate setting, characterized by communities, endemic regions of a specific disease (e.g., meningitis, malaria), urban settlements, districts, and humanitarian settings. These settings do not necessarily match the administrative unit, usually delineating the modeled setting.
Sixth, research that supports the coordination of programs and partnerships, taking into account the time dimension as well as the collaboration between public and private stakeholders, has hardly been found and is definitely needed.
Main insights
We performed a literature review covering (a) how immunization impacts the SDGs, (b) the factors that endanger the sustainability of immunization in LMICs (c) the research gap to enhance decision making for SDG-promoting implementations related to immunization.
By categorizing papers based on their SDG impact, it was confirmed that immunization can contribute to 14 of the 17 SDGs through direct and indirect mechanisms (see Background section, Fig. 1 ). SDG3 represents the core purpose of the immunization system, but due to the interconnectedness of the SDGs, investing in health entails increased productivity and economic development. This, in turn, reinforces the strengthening of the health system, creating a positive reinforcing relationship. In contrast, environmental health is not automatically positively impacted by both human health and economic development. For instance, population growth and anthropogenic disturbance of the natural system can trigger a change in disease ecology. This can lead to increased exposure to pathogens and infectious disease transmission. Moreover, both the exposure and the transmission occur in an inequitable fashion, further depriving already marginalized populations and thereby disproportionally increasing their vulnerability to infection. The way forward, as sketched by the SDGs, should reconcile the environment-economic-health effects without relying on trade-offs but by changing the paradigm from short-term human-focused Public health to SDG-supporting Planetary health . Such an approach takes into account the connections between the SDGs for intervention design and evaluation.
Sustainability challenges were found in all of the WHO’s Health Systems Building-Blocks, including population engagement and inequity in access to vaccination, resource limitations and workforce empowerment, vaccine supply sustainability, and governance and evidence-based decision support.
Model-based research found in literature offers implementable solutions to the sustainability challenges but needs to be further expanded in order to significantly support the WHO Immunization Agenda2030.
Recommendations for future research include a focus on resilience, transdisciplinary modeling, evaluating interventions based on the SDGs, modeling implementation along with intervention, design tailored solutions when needed, support coordination of services and partnerships.
For ease of reference, we list the basic insights from this paper in Table 7 .
Limitations
This work has several limitations when it comes to the completeness of the literature review. The keyword “sustainability” was not very effective, and even by applying exclusion and inclusion criteria, there were many more papers that could be mentioned. As the purpose was not a bibliographic review but rather an exploration of the SDG universe, the position of immunization in it, and how research can contribute to it, the paper sample was considered suitable for our purposes.
Relevance in times of COVID-19
As this work was written, the world witnessed the COVID-19 pandemic and its devastating effect, in line with what could be expected from the pre-2020 literature. The paths on the system map explain what is happening. However, as long as they have not led to solutions, they have no substantial impact in preparing the world for the humanitarian and economic shock wave that a pandemic causes on top of already existing epidemics, the threat of famine, and ongoing unrest. The current pandemic painfully exposes the weaknesses in existing health systems worldwide and affects the routine immunization services that will require great efforts to recover and avoid other disease outbreaks. For this reality, the research community needs to take up its role to support the transformation to more sustainable and resilient immunization systems.
Availability of data and materials
Not applicable.
Ensure healthy lives and promote well-being for all at all ages ( https://sustainabledevelopment.un.org/sdg3 )
2nd dose of measles-mumps-rubella vaccine
Human papillomavirus
Abbreviations
Agent Based Modeling
Community Health Workers
Causal Loop Diagram
Emerging Infectious Disease
Expanded Program on Immunization
Geographical Information System
Global Vaccine Action program
Human Immunodeficiency Virus
Human Papilloma Virus
Health System
Health System Strengthening
International Health Regulations
Integrated People-Centered Health Services
National Immunization Technical Advisory Group
Neglected Tropical Disease
Low and Middle Income Country
Official Development Assistance
Performance Based Financing
System Dynamics
Social sciences, Humanities and the Arts for People and the Economy
Supplemental Immunization Activities
Susceptible-Infectious-Recovered
Strategic Priorities
Sub Saharan Africa
Science, Technology, Engineering, and Maths
Universal Health Care
Vaccine Preventable Disease
Talisuna AO, Okiro EA, Yahaya AA, Stephen M, Bonkoungou B, Musa EO, et al. Spatial and temporal distribution of infectious disease epidemics, disasters and other potential public health emergencies in the World Health Organisation Africa region, 2016-2018. Glob Health. 2020;16(1):1–12.
Article Google Scholar
WHO. Immunization Agenda 2030. 2019.
Google Scholar
World Health Organization. World Health Statistics 2017: Monitoring health for the sustainable development goals. World Health Organization. Geneva; 2017. 116.
Ozawa S, Clark S, Portnoy A, Grewal S, Brenzel L, Walker DG. Return on investment from childhood immunization in low- and middle-income countries, 2011–20. Health Aff. 2016;35(2):199–207.
Chiappelli F, Bakhordarian A, Thames AD, Du AM, Jan AL, Nahcivan M, et al. Ebola: translational science considerations. J Transl Med. 2015;13(1):11.
Article PubMed PubMed Central Google Scholar
Young HS, McCauley DJ, Dirzo R, Nunn CL, Campana MG, Agwanda B, et al. Interacting effects of land use and climate on rodent-borne pathogens in Central Kenya. Philos Trans R Soc B Biol Sci. 2017;372(1722):20160116.
Graham BS, Sullivan NJ. Emerging viral diseases from a vaccinology perspective: preparing for the next pandemic. Nat Immunol. 2018;19(1):20–8.
Article CAS PubMed Google Scholar
Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, et al. Safeguarding human health in the Anthropocene epoch: report of the Rockefeller Foundation–Lancet commission on planetary health. Lancet. 2015;386(10007):1973–2028.
Article PubMed Google Scholar
Kovacs G, Moshtari M. A roadmap for higher research quality in humanitarian operations: a methodological perspective. Eur J Oper Res. 2019;276(2):395–408.
Besiou M, Stapleton O, Van Wassenhove LN. System dynamics for humanitarian operations. J Humanit Logist Supply Chain Manag. 2011;1(1):78–103.
de Savigny D, Adam T. Systems thinking for health systems strengthening; 2009.
Boischio A, Sánchez A, Orosz Z, Charron D. Health and sustainable development: challenges and opportunities of ecosystem approaches in the prevention and control of dengue and Chagas disease. Cad Saude Publica. 2009;25(suppl 1):S149–54.
Agyepong IA, Sewankambo N, Binagwaho A, Coll-Seck AM, Corrah T, Ezeh A, et al. The path to longer and healthier lives for all Africans by 2030: the lancet commission on the future of health in sub-Saharan Africa. Lancet. 2017;390(10114):2803–59.
Verguet S, Feldhaus I, Jiang Kwete X, Aqil A, Atun R, Bishai D, et al. Health system modelling research: towards a whole-health-system perspective for identifying good value for money investments in health system strengthening. BMJ Glob Heal. 2019;4(2):e001311.
Carey G, Malbon E, Carey N, Joyce A, Crammond B, Carey A. Systems science and systems thinking for public health: a systematic review of the field. BMJ Open. 2015;5(12):e009002.
Cassidy R, Singh NS, Schiratti P-R, Semwanga A, Binyaruka P, Sachingongu N, et al. Mathematical modelling for health systems research: a systematic review of system dynamics and agent-based models. BMC Health Serv Res. 2019;19(1):845.
Chughtai S, Blanchet K. Systems thinking in public health: a bibliographic contribution to a meta-narrative review. Health Policy Plan. 2017;32(4):czw159.
Cilenti D, Issel M, Wells R, Link S, Lich KH. System dynamics approaches and collective action for community health: an integrative review. Am J Community Psychol. 2019;63(3–4):527–45.
De Boeck K, Decouttere C, Vandaele N. Vaccine distribution chains in low- and middle-income countries: A literature review. Omega. 2020;97:102097.
Adamu AA, Jalo RI, Habonimana D, Wiysonge CS. COVID-19 and routine childhood immunization in Africa: leveraging systems thinking and implementation science to improve immunization system performance. Int J Infect Dis. 2020;98:161–5.
Article CAS PubMed PubMed Central Google Scholar
Sheff MC, Bawah AA, Asuming PO, Kyei P, Kushitor M, Phillips JF, et al. Evaluating health service coverage in Ghana’s Volta region using a modified Tanahashi model. Glob Health Action. 2020;13(1):1732664.
Barnighausen T, Bloom DE, Cafiero-Fonseca ET, O’Brien JC. Valuing vaccination. Proc Natl Acad Sci. 2014;111(34):12313–9.
Bangert M, Molyneux DH, Lindsay SW, Fitzpatrick C, Engels D. The cross-cutting contribution of the end of neglected tropical diseases to the sustainable development goals. Infect Dis Poverty. 2017;6(1):73.
World health statistics 2020: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
Nelson KN, Wallace AS, Sodha SV, Daniels D, Dietz V. Assessing strategies for increasing urban routine immunization coverage of childhood vaccines in low and middle-income countries: a systematic review of peer-reviewed literature. Vaccine. 2016;34(46):5495–503.
Jimenez J. Vaccines - a wonderful tool for equity in health. Vaccine. 2001;19(17–19):2201–5.
Aung MN, Koyanagi Y, Yuasa M. Health inequality among different economies during early phase of COVID-19 pandemic. J Egypt Public Health Assoc. 2021;96(1):3.
Vale DB, Teixeira JC, Bragança JF, Derchain S, Sarian LO, Zeferino LC. Elimination of cervical cancer in low- and middle-income countries: inequality of access and fragile healthcare systems. Int J Gynecol Obstet. 2021;152(1):7–11.
Bowen KJ, Ebi KL. Governing the health risks of climate change: opportunities for regeneration in an age of planetary health. Curr Opin Environ Sustain. 2020;46:1–2.
Sami S, Mayai A, Sheehy G, Lightman N, Boerma T, Wild H, et al. Maternal and child health service delivery in conflict-affected settings: a case study example from upper Nile and Unity states, South Sudan. Confl Health. 2020;14(1):34.
Valadez JJ, Berendes S, Odhiambo J, Vargas W, Devkota B, Lako R, et al. Is development aid to strengthen health systems during protracted conflict a useful investment? The case of South Sudan, 2011–2015. BMJ Glob Heal. 2020;5(4):e002093.
Nyemba WR, Chinguwa S, Marango BL, Mbohwa C. Evaluation and feasibility assessment of the sustainability of refrigeration systems devoid of harmful refrigerants for storage of vaccines. Procedia Manuf. 2019;35:291–7.
Hartmann K, Pagliusi S, Precioso A. Landscape analysis of pharmacovigilance and related practices among 34 vaccine manufacturers’ from emerging countries. Vaccine. 2020;38(34):5490–7.
Pagliusi S, Ting CC, Lobos F, Datla M, Gao S, Homma A, et al. Vaccines: shaping global health. Vaccine. 2017;35(12):1579–85.
Décobert A. Partnerships for Universal Health Coverage in Myanmar: Power and Politics within ‘Immunisation Encounters’ in Kayah State and Kayin State. J Dev Stud. 2021;57(8):1267–81.
Mutabazi JC, Gray C, Muhwava L, Trottier H, Ware LJ, Norris S, et al. Integrating the prevention of mother-to-child transmission of HIV into primary healthcare services after AIDS denialism in South Africa: perspectives of experts and health care workers - a qualitative study. BMC Health Serv Res. 2020;20(1):582.
Andrus JK, Cochi SL, Cooper LZ, Klein JD. Combining global elimination of measles and rubella with strengthening of health systems in developing countries. Health Aff. 2016;35(2):327–33.
Mtema Z, Changalucha J, Cleaveland S, Elias M, Ferguson HM, Halliday JEB, et al. Mobile phones as surveillance tools: implementing and evaluating a large-scale Intersectoral surveillance system for rabies in Tanzania. PLoS Med. 2016;13(4):e1002002.
GAVI. Immunisation and the sustainable development goals. [cited 2021 Mar 23]. Available from: https://www.gavi.org/library/publications/gavi-fact-sheets/immunisation-and-the-sustainable-development-goals .
Decade of Vaccine Collaboration. Global Vaccine Action Plan 2011-2020, vol. 31: supp., Vaccine. Elsevier Ltd; 2013. p. B1–250. Available from: https://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/
COVAX: CEPI’s response to COVID-19 – CEPI [Internet]. [cited 2021 Mar 21]. Available from: https://cepi.net/COVAX/
Cleaveland S, Sharp J, Abela-Ridder B, Allan KJ, Buza J, Crump JA, et al. One health contributions towards more effective and equitable approaches to health in low- and middle-income countries. Philos Trans R Soc B Biol Sci. 2017;372(1725):20160168.
Salam RA, Das JK, Bhutta ZA. Integrating nutrition into health systems: What the evidence advocates. Matern CHILD Nutr. 2019;15(1, SI):e12738.
Myers SS. Planetary health: protecting human health on a rapidly changing planet. Lancet. 2017;390(10114):2860–8.
Antoine-Moussiaux N, Janssens de Bisthoven L, Leyens S, Assmuth T, Keune H, Jakob Z, et al. The good, the bad and the ugly: framing debates on nature in a one health community. Sustain Sci. 2019;14(6):1729–38.
Chatterjee P, Chauhan AS, Joseph J, Kakkar M. One health/EcoHealth capacity building programs in south and South East Asia: a mixed method rapid systematic review. Hum Resour Health. 2017;15(1):72.
Abbas SS, Kakkar M, Rogawski ET. Costs Analysis of a Population Level Rabies Control Programme in Tamil Nadu, India. PLoS Negl Trop Dis. 2014;8(2):e2721.
Canavese D, Ortega NRS. A proposal of a fuzzy rule-based system for the analysis of health and health environments in Brazil. Ecol Indic. 2013;34:7–14.
Morton S, Pencheon D, Squires N. Sustainable development goals (SDGs), and their implementation. Br Med Bull. 2017;124(1):1–10.
Bunch MJ. Ecosystem approaches to health and well-being: navigating complexity, promoting health in social-ecological systems. Syst Res Behav Sci. 2016;33(5):614–32.
Horton R, Beaglehole R, Bonita R, Raeburn J, McKee M, Wall S. From public to planetary health: a manifesto. Lancet. 2014;383(9920):847.
Lang T, Rayner G. Ecological public health: the 21st century’s big idea? An essay by Tim Lang and Geof Rayner. BMJ. 2012;345(aug21 1):e5466.
Hunter PR, Zmirou-Navier D, Hartemann P. Estimating the impact on health of poor reliability of drinking water interventions in developing countries. Sci Total Environ. 2009;407(8):2621–4.
Hsiao A, Hall AH, Mogasale V, Quentin W. The health economics of cholera: a systematic review. Vaccine. 2018;36(30):4404–24.
Brattig NW, Tanner M, Bergquist R, Utzinger J. Impact of environmental changes on infectious diseases: Key findings from an international conference in Trieste, Italy in May 2017. Acta Trop. 2021;213:105165.
Joffe M, Gambhir M, Chadeau-Hyam M, Vineis P. Causal diagrams in systems epidemiology. Emerg Themes Epidemiol. 2012;9(1):1.
Cerf ME. Sustainable development goal integration, interdependence, and implementation: the environment–economic–health Nexus and universal health coverage. Glob Challenges. 2019;3(9):1900021.
Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8(1):117.
Duintjer Tebbens RJ, Thompson KM. Priority shifting and the dynamics of managing eradicable infectious diseases. Manag Sci. 2009;55(4):650–63.
Barasa EW, Cloete K, Gilson L. From bouncing back, to nurturing emergence: reframing the concept of resilience in health systems strengthening. Health Policy Plan. 2017;32(suppl_3):iii91–4.
Blanchet K. Thinking shift on health systems: from blueprint health programmes towards resilience of health systems. Int J Heal policy Manag. 2015;4(5):307–9.
Jansen KU, Knirsch C, Anderson AS. The role of vaccines in preventing bacterial antimicrobial resistance. Nat Med. 2018;24(1):10–9.
Chen RT, Shimabukuro TT, Martin DB, Zuber PLF, Weibel DM, Sturkenboom M. Enhancing vaccine safety capacity globally: a lifecycle perspective. Am J Prev Med. 2015;33(4):D46–54.
Brandileone M-CC, Almeida SCG, Minamisava R, Andrade A-L. Distribution of invasive Streptococcus pneumoniae serotypes before and 5 years after the introduction of 10-valent pneumococcal conjugate vaccine in Brazil. Vaccine. 2018;36(19):2559–66.
Ojal J, Flasche S, Hammitt LL, Akech D, Kiti MC, Kamau T, et al. Sustained reduction in vaccine-type invasive pneumococcal disease despite waning effects of a catch-up campaign in Kilifi, Kenya: a mathematical model based on pre-vaccination data. Vaccine. 2017;35(35):4561–8.
Cleary S, Erasmus E, Gilson L, Michel C, Gremu A, Sherr K, et al. The everyday practice of supporting health system development: learning from how an externally-led intervention was implemented in Mozambique. Health Policy Plan. 2018;33(7):801–10.
Djukpen RO. Understanding the spatial and temporal patterns of measles infections in Nigeria. African Geogr Rev. 2005;24(1):71–91.
Oppenheim B, Gallivan M, Madhav NK, Brown N, Serhiyenko V, Wolfe ND, et al. Assessing global preparedness for the next pandemic: development and application of an epidemic preparedness index. BMJ Glob Heal. 2019;4(1):e001157.
Osakunor DNM, Sengeh DM, Mutapi F. Coinfections and comorbidities in African health systems: at the interface of infectious and noninfectious diseases. PLoS Negl Trop Dis. 2018;12(9):e0006711.
Banura C, Mirembe FM, Katahoire AR, Namujju PB, Mbidde EK. Universal routine HPV vaccination for young girls in Uganda: a review of opportunities and potential obstacles. Infect Agent Cancer. 2012;7(1):24.
Ratzan SC, Bloom BR, El-Mohandes A, Fielding J, Gostin LO, Hodge JG, et al. The Salzburg statement on vaccination acceptance. J Health Commun. 2019;24(5):581–3.
Handy LK, Maroudi S, Powell M, Nfila B, Moser C, Japa I, et al. The impact of access to immunization information on vaccine acceptance in three countries. PLoS One. 2017;12(8):e0180759.
Article PubMed PubMed Central CAS Google Scholar
Larson HJ. The state of vaccine confidence. Lancet. 2018;392:2244–6.
Gatera M, Bhatt S, Ngabo F, Utamuliza M, Sibomana H, Karema C, et al. Successive introduction of four new vaccines in Rwanda: high coverage and rapid scale up of Rwanda’s expanded immunization program from 2009 to 2013. Vaccine. 2016;34:3420–6.
Dorji T, Tshomo U, Phuntsho S, Tamang TD, Tshokey T, Baussano I, et al. Introduction of a national HPV vaccination program into Bhutan. Vaccine. 2015;33(31):3726–30.
Guignard A, Praet N, Jusot V, Bakker M, Baril L. Introducing new vaccines in low- and middle-income countries: challenges and approaches. Expert Rev Vaccines. 2019;18(2):119–31.
Pool R, Munguambe K, Macete E, Aide P, Juma G, Alonso P, et al. Community response to intermittent preventive treatment delivered to infants (IPTi) through the EPI system in Manhiça, Mozambique. Trop Med Int Health. 2006;11(11):1670–8.
Pan WK, Seidman JC, Ali A, Hoest C, Mason C, Mondal D, et al. Oral polio vaccine response in the MAL-ED birth cohort study: considerations for polio eradication strategies. Vaccine. 2019;37(2):352–65.
Cutts FT, Ferrari MJ, Krause LK, Tatem AJ, Mosser JF. Vaccination strategies for measles control and elimination: time to strengthen local initiatives. BMC Med. 2021;19(1):1–8.
Huang W, Long H, Li J, Tao S, Zheng P, Tang S, et al. Delivery of public health services by community health workers (CHWs) in primary health care settings in China: a systematic review (1996–2016). Glob Heal Res Policy. 2018;3(1):18.
Walsh A, Matthews A, Manda-Taylor L, Brugha R, Mwale D, Phiri T, et al. The role of the traditional leader in implementing maternal, newborn and child health policy in Malawi. Health Policy Plan. 2018;33(8):879–87.
Al Gunaid M, Lami F, Jarour N. A collaborative initiative to strengthen sustainable public health capacity for polio eradication and routine immunization activities in the eastern Mediterranean region. JMIR Public Heal Surveill. 2019;5(4):e14664.
Gilmore B, McAuliffe E, Larkan F, Conteh M, Dunne N, Gaudrault M, et al. How do community health committees contribute to capacity building for maternal and child health? A realist evaluation protocol. BMJ Open. 2016;6(11):e011885.
Behl AS, Vijayaraghavan M, Nordin JD, Maciosek MV, Strebel PM. Community-level incentives to increase the use of vaccination services in developing countries: an idea whose time has come? Vaccine. 2010;28(38):6123–4.
Goga A, Feucht U, Zar HJ, Vanker A, Wiysonge CS, McKerrow N, et al. Neonatal, infant and child health in South Africa: reflecting on the past towards a better future. South African Med J. 2019;109(11b):83.
Article CAS Google Scholar
Fiedler JL, Chuko T. The cost of child health days: a case study of Ethiopia’s enhanced outreach strategy (EOS). Health Policy Plan. 2008;23(4):222–33.
Tambo E, Ngogang JY, Ning X, Xiao NZ. Strengthening community support, resilience programmes and interventions in infectious diseases of poverty. East Mediterr Heal J. 2018;24(6):598–603.
Haines A, Sanders D, Lehmann U, Rowe AK, Lawn JE, Jan S, et al. Achieving child survival goals: potential contribution of community health workers. Lancet. 2007;369(9579):2121–31.
Kumar V, Kumar A, Ghosh AK, Samphel R, Yadav R, Yeung D, et al. Enculturating science: community-centric design of behavior change interactions for accelerating health impact. Semin Perinatol. 2015;39(5):393–415.
Amponsah-Dacosta E, Kagina BM, Olivier J. Health systems constraints and facilitators of human papillomavirus immunization programmes in sub-Saharan Africa: a systematic review. Health Policy Plan. 2020;35(6):701–17.
Srivastava S, Fledderjohann J, Upadhyay AK. Explaining socioeconomic inequalities in immunisation coverage in India: new insights from the fourth National Family Health Survey (2015-16). BMC Pediatr. 2020;20(1):295.
Chen YJ, Chindarkar N, Xiao Y. Effect of reliable electricity on health facilities, health information, and child and maternal health services utilization: evidence from rural Gujarat, India. J Heal Popul Nutr. 2019;38(1):7.
Arsenault C, Johri M, Nandi A, Mendoza Rodríguez JM, Hansen PM, Harper S. Country-level predictors of vaccination coverage and inequalities in Gavi-supported countries. Vaccine. 2017;35(18):2479–88.
Bosetti P, Poletti P, Stella M, Lepri B, Merler S, De Domenico M. Heterogeneity in social and epidemiological factors determines the risk of measles outbreaks. Proc Natl Acad Sci. 2020;117(48):30118–25.
Sherr K, Fernandes Q, Kanté AM, Bawah A, Condo J, Mutale W. Measuring health systems strength and its impact: experiences from the African health initiative. BMC Health Serv Res. 2017;17(S3):827.
Kruk ME, Ling EJ, Bitton A, Cammett M, Cavanaugh K, Chopra M, et al. Building resilient health systems: a proposal for a resilience index. BMJ. 2017;357(May):1–8.
Levine OS. What drivers will influence global immunizations in the era of grand convergence in global health? Vaccine. 2017;35:A6–9.
Jamison DT, Summers LH, Alleyne G, Arrow KJ, Berkley S, Binagwaho A, et al. Global health 2035: a world converging within a generation. Lancet. 2013;382(9908):1898–955.
Cerf ME. The sustainable development goals: contextualizing Africa’s economic and health landscape. Glob Challenges. 2018;2(8):1800014.
Mounier-Jack S, Burchett HED, Griffiths UK, Konate M, Diarra KS. Meningococcal vaccine introduction in Mali through mass campaigns and its impact on the health system. Glob Heal Sci Pract. 2014;2(1):117–29.
Haq Z, Shaikh BT, Tran N, Hafeez A, Ghaffar A. System within systems: challenges and opportunities for the expanded Programme on immunisation in Pakistan. Heal Res Policy Syst. 2019;17(1):51.
MacDonald NE, Harmon S, Dube E, Steenbeek A, Crowcroft N, Opel DJ, et al. Mandatory infant & childhood immunization: rationales, issues and knowledge gaps. Vaccine. 2018;36(39):5811–8.
Adam T. Advancing the application of systems thinking in health. Heal Res Policy Syst. 2014;12(1):50.
Bloom DE, Madhavan G. Vaccines: from valuation to resource allocation. Vaccine. 2015;33(S2):B52–4.
Heaton A, Krudwig K, Lorenson T, Burgess C, Cunningham A, Steinglass R. Doses per vaccine vial container: an understated and underestimated driver of performance that needs more evidence. Vaccine. 2017;35(17):2272–8.
Karp CL, Lans D, Esparza J, Edson EB, Owen KE, Wilson CB, et al. Evaluating the value proposition for improving vaccine thermostability to increase vaccine impact in low and middle-income countries. Vaccine. 2015;33(30):3471–9.
Dicko M, Souare B, Sarr LC, Gueye B. When technical achievements aren’t enough: lessons learned from efforts to catalyze policy action on supply chain in Senegal. Vaccine. 2017;35(17):2209–13.
Báscolo E, Cid C, Pablo Pagano J, Soledad Urrutia M, Del Riego A. The challenge of sustainability of expanded programs on immunization. Rev Panam Salud Pública. 2017;41:1.
González-Lorenzo M, Piatti A, Coppola L, Gramegna M, Demicheli V, Melegaro A, et al. Conceptual frameworks and key dimensions to support coverage decisions for vaccines. Vaccine. 2015;33(9):1206–17.
Pitman R, Fisman D, Zaric GS, Postma M, Kretzschmar M, Edmunds J, et al. Dynamic transmission modeling: a report of the ISPOR-SMDM modeling good research practices task Force-5. Value Heal. 2012;15(6):828–34.
Gessner BD, Kaslow D, Louis J, Neuzil K, O’Brien KL, Picot V, et al. Estimating the full public health value of vaccination. Vaccine. 2017;35(46):6255–63.
Howard N, Walls H, Bell S, Mounier-Jack S. The role of National Immunisation Technical Advisory Groups (NITAGs) in strengthening national vaccine decision-making: a comparative case study of Armenia, Ghana, Indonesia, Nigeria, Senegal and Uganda. Vaccine. 2018;36(37):5536–43.
Lee BY, Mueller LE, Tilchin CG. A systems approach to vaccine decision making. Vaccine. 2017;35:A36–42.
Dawa J, Chaves SS, Ba Nguz A, Kalani R, Anyango E, Mutie D, et al. Developing a seasonal influenza vaccine recommendation in Kenya: process and challenges faced by the National Immunization Technical Advisory Group (NITAG). Vaccine. 2019;37(3):464–72.
Duintjer Tebbens RJ, Pallansch MA, Cochi SL, Ehrhardt DT, Farag NH, Hadler SC, et al. Modeling poliovirus transmission in Pakistan and Afghanistan to inform vaccination strategies in Undervaccinated subpopulations. Risk Anal. 2018;38(8):1701–17.
Duintjer Tebbens RJ, Thompson KM. Evaluation of proactive and reactive strategies for polio eradication activities in Pakistan and Afghanistan. Risk Anal. 2019;39(2):389–401.
Brearley L, Eggers R, Steinglass R, Vandelaer J. Applying an equity lens in the decade of vaccines. Vaccine. 2013;31(SUPPL2):B103–7.
Rheingans R, Anderson JD, Bagamian KH, Laytner LA, Pecenka CJ, Gilani SSA, et al. Effects of geographic and economic heterogeneity on the burden of rotavirus diarrhea and the impact and cost-effectiveness of vaccination in Pakistan. Vaccine. 2018;36(51):7780–9.
Sadr-Azodi N, DeRoeck D, Senouci K. Breaking the inertia in coverage: mainstreaming under-utilized immunization strategies in the Middle East and North Africa region. Vaccine. 2018;36(30):4425–32.
Adedokun ST, Uthman OA, Adekanmbi VT, Wiysonge CS. Incomplete childhood immunization in Nigeria: a multilevel analysis of individual and contextual factors. BMC Public Health. 2017;17(1):236.
Eonomopoulou A, Pavli A, Stasinopoulou P, Giannopoulos LA, Tsiodras S. Migrant screening: lessons learned from the migrant holding level at the Greek-Turkish borders. J Infect Public Health. 2017;10(2):177–84.
Adams AM, Rabbani A, Ahmed S, Mahmood SS, Al-Sabir A, Rashid SF, et al. Explaining equity gains in child survival in Bangladesh: scale, speed, and selectivity in health and development. Lancet. 2013;382(9909):2027–37.
Phillips DE, Dieleman JL, Shearer JC, Lim SS. Childhood vaccines in Uganda and Zambia: determinants and barriers to vaccine coverage. Vaccine. 2018;36(29):4236–44.
Achoki T, Lesego A. The imperative for systems thinking to promote access to medicines, efficient delivery, and cost-effectiveness when implementing health financing reforms: a qualitative study. Int J Equity Health. 2017;16(1):53.
Javed S, Chattu VK. Strengthening the COVID-19 pandemic response, global leadership, and international cooperation through global health diplomacy. Heal Promot Perspect. 2020;10(4):300 –305–300–305.
Feldhaus I, Schütte C, Mwansa FD, Undi M, Banda S, Suharlim C, et al. Incorporating costing study results into district and service planning to enhance immunization programme performance: a Zambian case study. Health Policy Plan. 2019;34(5):327–36.
Goldhaber-Fiebert JD, Lipsitch M, Mahal A, Zaslavsky AM, Salomon JA. Quantifying Child Mortality Reductions Related to Measles Vaccination. PLoS One. 2010;5(11):e13842.
Kwamie A, van Dijk H, Agyepong IA. Advancing the application of systems thinking in health: realist evaluation of the leadership development Programme for district manager decision-making in Ghana. Heal Res Policy Syst. 2014;12(1):29.
Tumusiime P, Kwamie A, Akogun OB, Elongo T, Nabyonga-Orem J. Towards universal health coverage: reforming the neglected district health system in Africa. BMJ Glob Heal. 2019;4(Suppl 9):e001498.
Clements CJ, Watkins M, de Quadros C, Biellik R, Hadler J, McFarland D, et al. Researching routine immunization–do we know what we don’t know? Vaccine. 2011;29(47):8477–82.
Uzochukwu BSC, Okeke C, O’Brien N, Ruiz F, Sombie I, Hollingworth S. Health technology assessment and priority setting for universal health coverage: a qualitative study of stakeholders’ capacity, needs, policy areas of demand and perspectives in Nigeria. Glob Health. 2020;16(1):58.
De Vries H, Van Wassenhove LN. Do optimization models for humanitarian operations need a paradigm shift? Prod Oper Manag. 2019;29(1):55–61.
Akseer N, Rizvi A, Bhatti Z, Das JK, Everett K, Arur A, et al. Association of Exposure to civil conflict with maternal resilience and maternal and child health and health system performance in Afghanistan. JAMA Netw Open. 2019;2(11):e1914819.
Van Wassenhove LN. Humanitarian aid logistics: supply chain management in high gear. J Oper Res Soc. 2006;57(5):475–89.
Tambo E, Chengho CF, Ugwu CE, Wurie I, Jonhson JK, Ngogang JY. Rebuilding transformation strategies in post-Ebola epidemics in Africa. Infect Dis Poverty. 2017;6(1):71.
Shrivastava S, Shrivastava P. COVID-19 pandemic: ensuring health system sustainability through strengthening immunization activities. J Sci Soc. 2020;47(2):132.
Van Wassenhove LN. Sustainable innovation: pushing the boundaries of traditional operations management. Prod Oper Manag. 2019;28(12):2930–45.
Kirigia JM, Nabyonga-Orem J, Dovlo DYT. Space and place for WHO health development dialogues in the African region. BMC Health Serv Res. 2016;16(S4):221.
Shaikh BT, Hamid S, Hafeez A. Capacity building on health diplomacy: a training experience from Pakistan. East Mediterr Heal J. 2018;24(9):933–9.
Kamya C, Shearer J, Asiimwe G, Salisbury N, Waiswa P, Brinkerhoff J, et al. Evaluating Global Health partnerships: a case study of a Gavi HPV vaccine application process in Uganda. Int J Heal policy Manag. 2016;6(6):327–38.
Bennett B, Cohen IG, Davies SE, Gostin LO, Hill PS, Mankad A, et al. Future-proofing global health: governance of priorities. Glob Public Health. 2018;13(5):519–27.
Rasanathan JJKK, MacCarthy S, Diniz D, Torreele E, Gruskin S. Engaging human rights in the response to the evolving Zika virus epidemic. Am J Public Health. 2017;107(4):525–31.
Balabanova D, McKee M, Mills A, Walt G, Haines A. What can global health institutions do to help strengthen health systems in low income countries? Heal Res Policy Syst. 2010;8(1):22.
Arale A, Lutukai M, Mohamed S, Bologna L, Stamidis KV. Preventing Importation of Poliovirus in the Horn of Africa: The Success of the Cross-Border Health Initiative in Kenya and Somalia. Am J Trop Med Hyg. 2019;101(4_Suppl):100–6.
Kamya C, Abewe C, Waiswa P, Asiimwe G, Namugaya F, Opio C, et al. Uganda’s increasing dependence on development partner’s support for immunization – a five year resource tracking study (2012 – 2016). BMC Public Health. 2021;21(1):1–11.
Brenzel L. What have we learned on costs and financing of routine immunization from the comprehensive multi-year plans in GAVI eligible countries? Vaccine. 2015;33:A93–8.
Ozawa S, Grewal S, Portnoy A, Sinha A, Arilotta R, Stack ML, et al. Funding gap for immunization across 94 low- and middle-income countries. Vaccine. 2016;34(50):6408–16.
Griffiths UK, Bozzani FM, Chansa C, Kinghorn A, Kalesha-Masumbu P, Rudd C, et al. Costs of introducing pneumococcal, rotavirus and a second dose of measles vaccine into the Zambian immunisation programme: are expansions sustainable? Vaccine. 2016;34(35):4213–20.
Hanefeld J, Mayhew S, Legido-Quigley H, Martineau F, Karanikolos M, Blanchet K, et al. Towards an understanding of resilience: responding to health systems shocks. Health Policy Plan. 2018;33(3):355–67.
Haasis MA, Ceria JA, Kulpeng W, Teerawattananon Y, Alejandria M. Do Pneumococcal Conjugate Vaccines Represent Good Value for Money in a Lower-Middle Income Country? A Cost-Utility Analysis in the Philippines. PLoS One. 2015;10(7):e0131156.
Pfeiffer J, Gimbel S, Chilundo B, Gloyd S, Chapman R, Sherr K. Austerity and the “sector-wide approach” to health: the Mozambique experience. Soc Sci Med. 2017;187:208–16.
Doherty T, Besada D, Goga A, Daviaud E, Rohde S, Raphaely N. “If donors woke up tomorrow and said we can’t fund you, what would we do?” A health system dynamics analysis of implementation of PMTCT option B+ in Uganda. Global Health. 2017;13(1):51.
Nwude EC, Ugwoke RO, Uruakpa PC, Ugwuegbe US, Nwonye NG. Official development assistance, income per capita and health outcomes in developing countries: is Africa different? Cogent Econ Financ. 2020;8(1):1774970.
Cernuschi T, Gaglione S, Bozzani F. Challenges to sustainable immunization systems in Gavi transitioning countries. Vaccine. 2018;36(45):6858–66.
Saxenian H, Hecht R, Kaddar M, Schmitt S, Ryckman T, Cornejo S. Overcoming challenges to sustainable immunization financing: early experiences from GAVI graduating countries. Health Policy Plan. 2015;30(2):197–205.
Ikilezi G, Augusto OJ, Dieleman JL, Sherr K, Lim SS. Effect of donor funding for immunization from Gavi and other development assistance channels on vaccine coverage: evidence from 120 low and middle income recipient countries. Vaccine. 2020;38(3):588–96.
Akseer N, Salehi AS, Hossain SMMM, Mashal MT, Rasooly MH, Bhatti Z, et al. Achieving maternal and child health gains in Afghanistan: a countdown to 2015 country case study. Lancet Glob Health. 2016;4(6):e395–413.
McDonough A, Rodríguez DC. How donors support civil society as government accountability advocates: a review of strategies and implications for transition of donor funding in global health. Glob Health. 2020;16(1):1–18.
Fonjungo F, Banerjee D, Abdulah R, Diantini A, Kusuma ASW, Permana MY, et al. Sustainable financing for new vaccines in Indonesia: challenges and strategies. Sustain. 2020;12(21):1–14.
Griffiths UK, Asman J, Adjagba A, Yo M, Oguta JO, Cho C. Budget line items for immunization in 33 African countries. Health Policy Plan. 2020;35(7):753–64.
Chukwu E, Garg L, Eze G. Mobile health insurance system and associated costs: a cross-sectional survey of primary health centers in Abuja, Nigeria. JMIR mHealth uHealth. 2016;4(2):e37.
Blecher MS, Meheus F, Kollipara A, Hecht R, Cameron NA, Pillay Y, et al. Financing vaccinations - the south African experience. Vaccine. 2012;30(SUPPL.3):C79–86.
Brooks A, Habimana D, Huckerby G, Ma GH. Making the leap into the next generation: a commentary on how Gavi, the vaccine Alliance is supporting countries’ supply chain transformations in 2016-2020. Vaccine. 2017;35(17):2110–4.
Lee BY, Connor DL, Wateska AR, Norman BA, Rajgopal J, Cakouros BE, et al. Landscaping the structures of GAVI country vaccine supply chains and testing the effects of radical redesign. Vaccine. 2015;33(36):4451–8.
Blanchet K, Palmer J, Palanchowke R, Boggs D, Jama A, Girois S. Advancing the application of systems thinking in health: analysing the contextual and social network factors influencing the use of sustainability indicators in a health system – a comparative study in Nepal and Somaliland. Heal Res Policy Syst. 2014;12(1):46.
Falisse J-BBJ-BB, Ndayishimiye J, Kamenyero V, Bossuyt M. Performance-based financing in the context of selective free health-care: an evaluation of its effects on the use of primary health-care services in Burundi using routine data. Health Policy Plan. 2015;30(10):1251–60.
Nyirenda L, Flikke R. Frontline vaccinators and immunisation coverage in Malawi. Forum Dev Stud. 2013;40(1):27–46.
Burchett HED, Mounier-Jack S, Torres-Rueda S, Griffiths UK, Ongolo-Zogo P, Rulisa S, et al. The impact of introducing new vaccines on the health system: case studies from six low- and middle-income countries. Vaccine. 2014;32(48):6505–12.
Gallagher KE, Erio T, Baisley K, Lees S, Watson-Jones D. The impact of a human papillomavirus (HPV) vaccination campaign on routine primary health service provision and health workers in Tanzania: a controlled before and after study. BMC Health Serv Res. 2018;18(1):173.
Kasonde M, Steele P. The people factor: an analysis of the human resources landscape for immunization supply chain management. Vaccine. 2017;35(17):2134–40.
Etamesor S, Ottih C, Salihu IN, Okpani AI. Data for decision making: using a dashboard to strengthen routine immunisation in Nigeria. BMJ Glob Heal. 2018;3(5):e000807.
Mc Kenna P, Babughirana G, Amponsah M, Egoeh SG, Banura E, Kanwagi R, et al. Mobile training and support (MOTS) service-using technology to increase Ebola preparedness of remotely-located community health workers (CHWs) in Sierra Leone. mHealth. 2019;5:35.
Tesfaye B, Makam JK, Sergon K, Onuekwusi I, Muitherero C, Sowe A. The role of the Stop Transmission of Polio (STOP) program in developing countries: the experience of Kenya. BMC Public Health. 2020;20(1):1110.
Waithaka D, Kagwanja N, Nzinga J, Tsofa B, Leli H, Mataza C, et al. Prolonged health worker strikes in Kenya- perspectives and experiences of frontline health managers and local communities in Kilifi County. Int J Equity Health. 2020;19(1):1–15.
Dasgupta R, Sharma S, Sharma N, Banerjee K, Haran EGPGP, Muliyel JPP, et al. Successful switch (tOPV to bOPV) in India: tribute to a resilient health system. Vaccine. 2019;37(17):2394–400.
Farrenkopf BA, Lee C-W. Mapping health workforce development strategies across key global health agencies: an assessment of objectives and key interventions. Health Policy Plan. 2019;34(6):461–8.
Kumar M, Gotz D, Nutley T, Smith JB. Research gaps in routine health information system design barriers to data quality and use in low- and middle-income countries: a literature review. Int J Health Plann Manag. 2018;33(1):e1–9.
Odit MCA, Rwashana AS, Kituyi GM. Antecedents and dynamics for strategic alignment of health information Systems in Uganda. Electron J Inf Syst Dev Ctries. 2014;64(1):1–20.
Frøen JF, Myhre SL, Frost MJ, Chou D, Mehl G, Say L, et al. eRegistries: electronic registries for maternal and child health. BMC Pregnancy Childbirth. 2016;16(1):11.
Labrique AB, Vasudevan L, Kochi E, Fabricant R, Mehl G. Mhealth innovations as health system strengthening tools: 12 common applications and a visual framework. Glob Heal Sci Pract. 2013;1(2):160–71.
Mehl G, Labrique A. Prioritizing integrated mHealth strategies for universal health coverage. Science (80- ). 2014;345(6202):1284–7.
Mahadevan S, Broaddus-Shea ET. How should home-based maternal and child health records be implemented? A global framework analysis. Glob Heal Pract. 2020;8(1):100 –113–100–113.
Scobie HM, Edelstein M, Nicol E, Morice A, Rahimi N, MacDonald NE, et al. Improving the quality and use of immunization and surveillance data: summary report of the working Group of the Strategic Advisory Group of experts on immunization. Vaccine. 2020;38(46):7183–97.
Mihigo R, Okeibunor J, Anya B, Mkanda P, Zawaira F. Challenges of immunization in the African region. Pan Afr Med J. 2017;27(Suppl 3):12.
PubMed PubMed Central Google Scholar
Diallo AO, Kiemtoré T, Bicaba BW, Medah I, Tarbangdo TF, Sanou S, et al. Development and Implementation of a Cloud-Based Meningitis Surveillance and Specimen Tracking System in Burkina Faso, 2018. J Infect Dis. 2019;220(Supplement_4):S198–205.
Patel JC, Soeters HM, Diallo AO, Bicaba BW, Kadadé G, Dembélé AY, et al. MenAfriNet: A Network Supporting Case-Based Meningitis Surveillance and Vaccine Evaluation in the Meningitis Belt of Africa. J Infect Dis. 2019;220(Supplement_4):S148–54.
Kim S, Lee J, Jung E. Mathematical model of transmission dynamics and optimal control strategies for 2009 a/H1N1 influenza in the Republic of Korea. J Theor Biol. 2017;412:74–85.
Fernandez-Luque L, Imran M. Humanitarian health computing using artificial intelligence and social media: a narrative literature review. Int J Med Inform. 2018;114:136–42.
Clarke KENN, Chibawe CP, Essiet-Gibson I, Mwansa FD, Jacenko S, Rhee C, et al. Strengths, pitfalls, and lessons learned in implementing electronic collection of childhood vaccination data in Zambia: the SmartCare experience. Int J Med Inform. 2019;129:146–53.
Aiga H, Nguyen VD, Nguyen CD, Nguyen TTT, Nguyen LTP. Fragmented implementation of maternal and child health home-based records in Vietnam: need for integration. Glob Health Action. 2016;9(1):29924.
Jarrett S, Wilmansyah T, Bramanti Y, Alitamsar H, Alamsyah D, Krishnamurthy KR, et al. The role of manufacturers in the implementation of global traceability standards in the supply chain to combat vaccine counterfeiting and enhance safety monitoring. Vaccine. 2020;38(52):8318–25.
Lloyd J, Cheyne J. The origins of the vaccine cold chain and a glimpse of the future. Vaccine. 2017;35(17):2115–20.
Lennon P, Atuhaire B, Yavari S, Sampath V, Mvundura M, Ramanathan N, et al. Root cause analysis underscores the importance of understanding, addressing, and communicating cold chain equipment failures to improve equipment performance. Vaccine. 2017;35(17):2198–202.
Robertson J, Franzel L, Maire D. Innovations in cold chain equipment for immunization supply chains. Vaccine. 2017;35(17):2252–9.
McCarney S, Robertson J, Arnaud J, Lorenson K, Lloyd J. Using solar-powered refrigeration for vaccine storage where other sources of reliable electricity are inadequate or costly. Vaccine. 2013;31(51):6050–7.
Friel S, Pescud M, Malbon E, Lee A, Carter R, Greenfield J, et al. Using systems science to understand the determinants of inequities in healthy eating. PLoS One. 2017;12(11):e0188872.
van den Ent MMVX, Yameogo A, Ribaira E, Hanson CM, Ratoto R, Rasolomanana S, et al. Equity and immunization supply chain in Madagascar. Vaccine. 2017;35(17):2148–54.
Jata Nyirenda L, Ingstad Sandberg K, Justice J. Forum for development studies when are health systems ready for new vaccines? The introduction of pneumococcal vaccine in Malawi when are health systems ready for new vaccines? The introduction of pneumococcal vaccine in Malawi. Forum Dev Stud. 2014;41:317–36.
Duijzer LE, van Jaarsveld W, Dekker R. Literature review: the vaccine supply chain. Eur J Oper Res. 2018;268(1):174–92.
Sato R, Thompson A, Sani I, Metiboba L, Giwa A, Femi-Ojo O, et al. Effect of vaccine direct delivery (VDD) on vaccine stockouts and number of vaccinations: case study from Bauchi state, Nigeria. Vaccine. 2021;39(9):1445–51.
Cernuschi T, Malvolti S, Nickels E, Friede M. Bacillus Calmette-Guérin (BCG) vaccine: a global assessment of demand and supply balance. Vaccine. 2017;36(4):498–506.
Duintjer Tebbens RJ, Pallansch MA, Alexander JP, Thompson KM. Optimal vaccine stockpile design for an eradicated disease: application to polio. Vaccine. 2010;28(26):4312–27.
Dellepiane N, Pagliusi S. Challenges for the registration of vaccines in emerging countries: differences in dossier requirements, application and evaluation processes. Vaccine. 2018;36(24):3389–96.
Buss PM, Chamas C, Faid M, Morel C. Development, health, and international policy: the research and innovation dimension. Cad Saude Publica. 2016;32(suppl 2):e00046815.
Cole CB, Trolle S, Edwards DJ. Developing the latest framework to measure and incentivise pharmaceutical industry contributions to health research and development. Heal Res Policy Syst. 2018;16(1):73.
Keith JA, Agostini Bigger L, Arthur PA, Maes E, Daems R. Delivering the promise of the decade of vaccines: opportunities and challenges in the development of high quality new vaccines. Vaccine. 2013;31:B184–93.
Plotkin S, Robinson JM, Cunningham G, Iqbal R, Larsen S. The complexity and cost of vaccine manufacturing – an overview. Vaccine. 2017;35(33):4064–71.
Pagliusi S, Dennehy M, Kim H. Vaccines, inspiring innovation in health. Vaccine. 2018;36(48):7430–7.
Luter N, Kumar R, Hozumi D, Lorenson T, Larsen S, Gowda B, et al. An updated methodology to review developing-country vaccine manufacturer viability. Vaccine. 2017;35(31):3897–903.
Jarrett S, Yang L, Pagliusi S. Roadmap for strengthening the vaccine supply chain in emerging countries: manufacturers’ perspectives. Vaccine X. 2020;5:100068.
Gadelha CAG, Braga PS da C, Montenegro KBM, Cesário BB. Access to vaccines in Brazil and the global dynamics of the health economic-industrial complex. Cad Saude Publica. 2020;36(suppl 2):e00154519.
Rappuoli R, Hanon E. Sustainable vaccine development: a vaccine manufacturer’s perspective. Curr Opin Immunol. 2018;53:111–8.
Eriksson P, Gessner BD, Jaillard P, Morgan C, Le Gargasson JB, Bernard J, et al. Vaccine vial monitor availability and use in low- and middle-income countries : a systematic review. Vaccine. 2017;35(17):2155–61.
Franceschi S, Clifford GM, Baussano I. Options for design of real-world impact studies of single-dose vaccine schedules. Vaccine. 2018;36(32):4816–22.
Kristensen D, Chen D. Strategies to advance vaccine technologies for resource-poor settings. Vaccine. 2013;31:B157–62.
Farmer P, Almazor CP, Bahnsen ET, Barry D, Bazile J, Bloom BR, et al. Meeting Cholera’s Challenge to Haiti and the World: A Joint Statement on Cholera Prevention and Care. PLoS Negl Trop Dis. 2011;5(5):e1145.
Le Menestrel M, Van Wassenhove LN. Subjectively biased objective functions. EURO J Decis Process. 2016;4(1–2):73–83.
Famakinde D. Mosquitoes and the lymphatic filarial parasites: research trends and budding roadmaps to future disease eradication. Trop Med Infect Dis. 2018;3(1):4.
Article PubMed Central Google Scholar
Hotez PJ, Ferris MT. The antipoverty vaccines. Vaccine. 2006;24(31–32):5787–99.
Mackenzie GA, Plumb ID, Sambou S, Saha D, Uchendu U, Akinsola B, et al. Monitoring the introduction of pneumococcal conjugate vaccines into West Africa: design and implementation of a population-based surveillance system. PLoS Med. 2012;9(1):e1001161.
Homma A, da Silva Freire M, Possas C. Vaccines for neglected and emerging diseases in Brazil by 2030: the “valley of death” and opportunities for RD&I in Vaccinology 4.0. Cad Saude Publica. 2020;36(suppl 2):e00128819.
Vallès X, Stenseth NC, Demeure C, Horby P, Mead PS, Cabanillas O, et al. Human plague: An old scourge that needs new answers. PLoS Negl Trop Dis. 2020;14(8):e0008251.
Graham JE. Ebola vaccine innovation: a case study of pseudoscapes in global health. Crit Public Health. 2019;29(4):401–12.
Prausnitz MR, Goodson JL, Rota PA, Orenstein WA. A microneedle patch for measles and rubella vaccination: a game changer for achieving elimination. Curr Opin Virol. 2020;41:68–76.
Bazos DA, LaFave LRA, Suresh G, Shannon KC, Nuwaha F, Splaine ME. The gas cylinder, the motorcycle and the village health team member: a proof-of-concept study for the use of the microsystems quality improvement approach to strengthen the routine immunization system in Uganda. Implement Sci. 2015;10(1):30.
Hu Y, Luo S, Tang X, Lou L, Chen Y, Guo J, et al. Does introducing an immunization package of services for migrant children improve the coverage, service quality and understanding? An evidence from an intervention study among 1548 migrant children in eastern China. BMC Public Health. 2015;15(1):664.
Manyazewal T, Mekonnen A, Demelew T, Mengestu S, Abdu Y, Mammo D, et al. Improving immunization capacity in Ethiopia through continuous quality improvement interventions: a prospective quasi-experimental study. Infect Dis Poverty. 2018;7(1):119.
Manakongtreecheep K, Davis R. A review of measles control in Kenya, with focus on recent innovations. Pan Afr Med J. 2017;27(Suppl 3):15.
Deressa W, Kayembe P, Neel AH, Mafuta E, Seme A, Alonge O. Lessons learned from the polio eradication initiative in the Democratic Republic of Congo and Ethiopia: analysis of implementation barriers and strategies. BMC Public Health. 2020;20:1807.
Arsenault C, Harper S, Nandi A, Mendoza Rodríguez JM, Hansen PM, Johri M. Monitoring equity in vaccination coverage: a systematic analysis of demographic and health surveys from 45 Gavi-supported countries. Vaccine. 2017;35(6):951–9.
Fields R, Dabbagh A, Jain M, Sagar KS, Singh K. Moving forward with strengthening routine immunization delivery as part of measles and rubella elimination activities. Vaccine. 2013;31(2):B115–21.
Chauke-Moagi BE, Mumba M. New vaccine introduction in the east and southern African sub-region of the WHO African region in the context of GIVS and MDGs. Vaccine. 2012;30(SUPPL.3):C3–8.
Ngabo F, Levin A, Wang SA, Gatera M, Rugambwa C, Kayonga C, et al. A cost comparison of introducing and delivering pneumococcal, rotavirus and human papillomavirus vaccines in Rwanda. Vaccine. 2015;33(51):7357–63.
Soi C, Babigumira JB, Chilundo B, Muchanga V, Matsinhe L, Gimbel S, et al. Implementation strategy and cost of Mozambique’s HPV vaccine demonstration project. BMC Public Health. 2019;19(1):1406.
Clements CJ, Nshimirimanda D, Gasasira A. Using immunization delivery strategies to accelerate progress in Africa towards achieving the millennium development goals. Vaccine. 2008;26(16):1926–33.
Deconinck H, Hallarou M, Criel B, Donnen P, Macq J. Integrating acute malnutrition interventions into national health systems: lessons from Niger. BMC Public Health. 2016;16(1):249.
Riaz BK, Ali L, Ahmad SA, Islam MZ, Ahmed KR, Hossain S. Community clinics in Bangladesh: a unique example of public-private partnership. Heliyon. 2020;6(5):e03950.
Eze GU, Adeleye OO. Enhancing routine immunization performance using innovative Technology in an Urban Area of Nigeria. West Afr J Med. 2015;34(1):3–10.
CAS PubMed Google Scholar
Dafilis MP, Frascoli F, McVernon J, Heffernan JM, McCaw JM. Dynamical crises, multistability and the influence of the duration of immunity in a seasonally-forced model of disease transmission. Theor Biol Med Model. 2014;11(1):43.
Bravo-Alcántara P, Pérez-Vilar S, Molina-León HF, Sturkenboom M, Black S, Zuber PLF, et al. Building capacity for active surveillance of vaccine adverse events in the Americas: a hospital-based multi-country network. Vaccine. 2018;36(3):363–70.
Amarasinghe A, Black S, Bonhoeffer J, Deotti SM, Dodoo A, Eskola J, et al. Effective vaccine safety systems in all countries : a challenge for more equitable access to immunization. Vaccine. 2013;31:B108–14.
Kelly-Cirino CD, Nkengasong J, Kettler H, Tongio I, Gay-Andrieu F, Escadafal C, et al. Importance of diagnostics in epidemic and pandemic preparedness. BMJ Glob Heal. 2019;4(Suppl 2):e001179.
World Health Organization. Vaccination in Acute Humanitarian Emergencies: Framework for Decision-Making. 2017. Available from: http://apps.who.int/iris/bitstream/10665/255575/1/WHO-IVB-17.03-eng.pdf?ua=1
Carland C, Goentzel J, Montibeller G. Modeling the values of private sector agents in multi-echelon humanitarian supply chains. Eur J Oper Res. 2018;269(2):532–43.
Mbengue MAS, Sarr M, Faye A, Badiane O, Camara FBN, Mboup S, et al. Determinants of complete immunization among senegalese children aged 12–23 months: evidence from the demographic and health survey. BMC Public Health. 2017;17(1):630.
Gralla E, Goentzel J. Humanitarian transportation planning: evaluation of practice-based heuristics and recommendations for improvement. Eur J Oper Res. 2018;269(2):436–50.
de Lima PA, Southgate R, Ahmed H, O’Connor P, Cramond V, Lenglet A. Infectious disease risk and vaccination in northern Syria after 5 years of civil war: the MSF experience. PLoS Curr. 2018;2:10.
Clarke A, Blidi N, Dahn B, Agbo C, Tuopileyi R, Rude MJ, et al. Strengthening acute flaccid paralysis surveillance post Ebola virus disease outbreak 2015–2017: the Liberia experience. Pan Afr Med J. 2019;33(Suppl 2):2.
Larson HJ, Lee N, Rabin KH, Rauh L, Ratzan SCOTTC. Building confidence to CONVINCE. J Health Commun. 2020;25(10):838–42.
Duintjer Tebbens RJ, Thompson KM. Using integrated modeling to support the global eradication of vaccine-preventable diseases. Syst Dyn Rev. 2018;34(1):78–120.
Brenzel L, Young D, Walker DG. Costs and financing of routine immunization: approach and selected findings of a multi-country study (EPIC). Vaccine. 2015;33(1):A13–20.
Gallagher KE, LaMontagne DS, Watson-Jones D. Status of HPV vaccine introduction and barriers to country uptake. Vaccine. 2018;36(32):4761–7.
Kim SS, Patel M, Hinman A. Use of m-health in polio eradication and other immunization activities in developing countries. Vaccine. 2017;35(10):1373–9.
Van Den Ent MMVX, Yameogo A, Ribaira E, Hanson CM, Ratoto R, Rasolomanana S, et al. Equity and immunization supply chain in Madagascar q. Vaccine. 2017;35(17):2148–54.
Deconinck H, Hallarou ME, Pesonen A, Gérard JC, Criel B, Donnen P, et al. Understanding factors that influence the integration of acute malnutrition interventions into the national health system in Niger. Health Policy Plan. 2016;31(10):1364–73.
World Health Organization (WHO), World Health Organization. Accessing Affordable and Timely Supply of Vaccines for use in Humanitarian Emergencies: the Humanitarian Mechanism. WHO working document. 2017.
Thompson KM, Duintjer Tebbens RJ. Using system dynamics to develop policies that matter: global management of poliomyelitis and beyond. Syst Dyn Rev. 2008;24(4):433–49.
Thompson KM, Duintjer Tebbens RJ. Modeling the dynamics of oral poliovirus vaccine cessation. J Infect Dis. 2014;210(Suppl 1):S475–84.
Thompson KM, Duintjer Tebbens RJ, Pallansch MA, Wassilak SGF, Cochi SL. Polio eradicators use integrated analytical models to make better decisions. Interfaces (Providence). 2015;45(1):5–25.
Thompson KM, Duintjer Tebbens RJ. Framework for optimal global vaccine stockpile Design for Vaccine-Preventable Diseases: application to measles and cholera vaccines as contrasting examples. Risk Anal. 2016;36(7):1487–509.
Duintjer Tebbens RJ, Pallansch MA, Kalkowska DA, Wassilak SGF, Cochi SL, Thompson KM. Characterizing poliovirus transmission and evolution: insights from modeling experiences with Wild and vaccine-related polioviruses. Risk Anal. 2013;33(4):703–49.
Kalkowska DA, Tebbens RJD, Thompson KM. Modeling strategies to increase population immunity and prevent poliovirus transmission in 2 high-risk areas in northern India. J Infect Dis. 2014;210(November):S398–411.
Rwashana AS. System dynamics modeling in healthcare: the Ugandan immunisation system. Int J Comput ICT Res Int J Comput ICT Res Spec Issue. 2008;1(1):85–98.
Semwanga Rwashana A, Willeese WD. Enhancing healthcare delivery through ICTs: A case study of the Ugandan immunisation system, International Journal of Education and Development using Information and Communication Technology (IJEDICT), vol. 4; 2008.
Rwashana AS, Williams DW, Neema S. System dynamics approach to immunization healthcare issues in developing countries: a case study of Uganda. Health Informatics J. 2009;15(2):95–107.
Rwashana AS, Nakubulwa S, Adam T. Applying a system dynamics modelling approach to explore policy options for improving neonatal health in Uganda. Heal Res Policy Syst. 2016;14(1):35.
Guttieres D, Sinskey AJ, Springs SL. Modeling framework to evaluate vaccine strategies against the COVID-19 pandemic. Systems. 2021;9(1):4.
McCormick BJJ, Waiswa P, Nalwadda C, Sewankambo NK, Knobler SL. SMART Vaccines 2.0 decision-support platform: a tool to facilitate and promote priority setting for sustainable vaccination in resource-limited settings. BMJ Glob Heal. 2020;5(11):e003587.
Renmans D, Holvoet N, Criel B. Combining theory-driven evaluation and causal loop diagramming for opening the ‘Black box’ of an intervention in the health sector: a case of performance-based financing in Western Uganda. Int J Environ Res Public Health. 2017;14(9):1007.
Alonge O, Lin S, Igusa T, Peters DH. Improving health systems performance in low- and middle-income countries: a system dynamics model of the pay-for-performance initiative in Afghanistan. Health Policy Plan. 2017;32(10):1417–26.
Sato R, Belel A. The effect of performance-based financing on child vaccinations in northern Nigeria. Vaccine. 2020;38(9):2209–15.
Utazi CE, Thorley J, Alegana VA, Ferrari MJ, Takahashi S, Metcalf CJE, et al. Mapping vaccination coverage to explore the effects of delivery mechanisms and inform vaccination strategies. Nat Commun. 2019;10(1):1–10.
Kivuti-Bitok LW, McDonnell G, Abdul R, Pokhariyal GP. System dynamics model of cervical cancer vaccination and screening interventions in Kenya. Cost Eff Resour Alloc. 2014;12(1):26.
Tetui M, Coe A-B, Hurtig A-K, Bennett S, Kiwanuka SN, George A, et al. A participatory action research approach to strengthening health managers’ capacity at district level in eastern Uganda. Heal Res Policy Syst. 2017;15(S2):110.
Gilson L, Elloker S, Olckers P, Lehmann U. Advancing the application of systems thinking in health: south African examples of a leadership of sensemaking for primary health care. Heal Res Policy Syst. 2014;12(1):30.
Sarriot E, Morrow M, Langston A, Weiss J, Landegger J, Tsuma L. A causal loop analysis of the sustainability of integrated community case management in Rwanda. Soc Sci Med. 2015;131:147–55.
Varghese J, Kutty VR, Paina L, Adam T. Advancing the application of systems thinking in health: understanding the growing complexity governing immunization services in Kerala, India. Heal Res Policy Syst. 2014;12(1):47.
Ozawa S, Paina L, Qiu M. Exploring pathways for building trust in vaccination and strengthening health system resilience. BMC Health Serv Res. 2016;16(S7):639.
Pananos AD, Bury TM, Wang C, Schonfeld J, Mohanty SP, Nyhan B, et al. Critical dynamics in population vaccinating behavior. Proc Natl Acad Sci U S A. 2017;114(52):13762–7.
Sarriot EG, Kouletio M, Jahan S, Rasul I, Musha A. Advancing the application of systems thinking in health: sustainability evaluation as learning and sense-making in a complex urban health system in northern Bangladesh. Heal Res Policy Syst. 2014;12(1):45.
Utazi CE, Thorley J, Alegana VA, Ferrari MJ, Takahashi S, Metcalf CJE, et al. High resolution age-structured mapping of childhood vaccination coverage in low and middle income countries. Vaccine. 2018;36(12):1583–91.
Jaafar IA, Zainal Abidin N, Mohd Jamil J. Modelling the prediction of dengue outbreak using system dynamics approach. J Teknol. 2016;78(6–4):107–13.
Knerer G, Currie CSM, Brailsford SC. Impact of combined vector-control and vaccination strategies on transmission dynamics of dengue fever: a model-based analysis. Health Care Manag Sci. 2015;18(2):205–17.
Grais RF, Conlan AJK, Ferrari MJ, Djibo A, Le Menach A, Bjørnstad ON, et al. Time is of the essence: exploring a measles outbreak response vaccination in Niamey, Niger. J R Soc Interface. 2008;5(18):67–74.
Duijzer LE, van Jaarsveld W, Dekker R. The benefits of combining early aspecific vaccination with later specific vaccination. Eur J Oper Res. 2018;271(2):606–19.
Araz OM. Integrating complex system dynamics of pandemic influenza with a multi-criteria decision making model for evaluating public health strategies. J Syst Sci Syst Eng. 2013;22(3):319–39.
Grefenstette JJ, Brown ST, Rosenfeld R, DePasse J, Stone NT, Cooley PC, et al. FRED (a framework for reconstructing epidemic dynamics): an open-source software system for modeling infectious diseases and control strategies using census-based populations. BMC Public Health. 2013;13(1):940.
Wu JT, Peak CM, Leung GM, Lipsitch M. Fractional dosing of yellow fever vaccine to extend supply: a modelling study. Lancet. 2016;388(10062):2904–11.
Pruyt E, Auping WL, Kwakkel JH. Ebola in West Africa: model-based exploration of social psychological effects and interventions. Syst Res Behav Sci. 2015;32(1):2–14.
Auping WL, Pruyt E, Kwakkel JH. Simulating endogenous dynamics of intervention-capacity deployment: Ebola outbreak in Liberia. Int J Syst Sci Oper Logist. 2017;4(1):53–67.
Garcia DM, Sheehan MC. Extreme weather-driven disasters and Children’s health. Int J Health Serv. 2016;46(1):79–105.
Bishai D, Paina L, Li Q, Peters DH, Hyder AA. Advancing the application of systems thinking in health: why cure crowds out prevention. Heal Res Policy Syst. 2014;12(1):28.
Schiavo R, Basu Roy U, Faroul L, Solodunova G. Grounding evaluation design in the socio-ecological model of health: a logic framework for the assessment of a national routine immunization communication initiative in Kyrgyzstan. Glob Health Promot. 2020;27(4):59–68.
Nelson R. COVID-19 disrupts vaccine delivery. Lancet Infect Dis. 2020;3099(20):30304.
Shah H. COVID-19 recovery: science isn’t enough to save us. Nature. 2021;591(7851):503.
Fisher MC, Murray KA. Emerging infections and the integrative environment-health sciences: the road ahead. Nat Rev Microbiol. 2021;19(3):133–5.
Adamu AA, Gadanya MA, Jalo RI, Uthman OA, Nnaji CA, Bello IW, et al. Assessing readiness to implement routine immunization among patent and proprietary medicine vendors in Kano, Nigeria: a theory-informed cross-sectional study. Expert Rev Vaccines. 2020;19(4):395–405.
Decouttere C, Vandaele N, Lemmens S, Bernuzzi M. The Vaccine Supply Chain Multathlon: the Reconciliation of Technology, Economy and Access to Medicines. In: Advances in Managing Humanitarian Operations. Cham: Springer International Publishing; 2016. p. 205–27. (International Series in Operations Research & Management Science).
Download references
Acknowledgements
This research was supported by the GSK Research Chair on Re-Design of Healthcare Supply Chains in Developing Countries to increase Access-to-Medicines. KDB is funded by a PhD fellowship from the Research Foundation – Flanders. The funders had no role in the design and conduct of the study.
Author information
Authors and affiliations.
KU Leuven, Access-To-Medicines research Center, Naamsestraat 69, Leuven, Belgium
Catherine Decouttere, Kim De Boeck & Nico Vandaele
You can also search for this author in PubMed Google Scholar
Contributions
CD analyzed and interpreted the literature, performed the analysis and did the major portion of the writing. NV constructed main structure of the body and joint writing. KDB was a contributor in writing and reviewing the manuscript. All authors read and approved the final manuscript.
Authors’ information
Corresponding author.
Correspondence to Nico Vandaele .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests, additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Decouttere, C., De Boeck, K. & Vandaele, N. Advancing sustainable development goals through immunization: a literature review. Global Health 17 , 95 (2021). https://doi.org/10.1186/s12992-021-00745-w
Download citation
Received : 30 July 2020
Accepted : 23 July 2021
Published : 26 August 2021
DOI : https://doi.org/10.1186/s12992-021-00745-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Immunization
- Sustainable development goals
- Low- and middle-income countries
- Systems thinking
- Health systems modeling
Globalization and Health
ISSN: 1744-8603
- Submission enquiries: [email protected]
- General enquiries: [email protected]
UN sustainable development goals and management of non-instantaneous deteriorating items: a literature review and applications framework
- Original Research
- Published: 01 August 2024
Cite this article

- Pratik Maheshwari 1 ,
- Sachin Kamble 2 ,
- Amine Belhadi 3 &
- Satish Kumar ORCID: orcid.org/0000-0001-5200-1476 4
Recent decades have seen a surge in reports of mismanagement and mishandling of non-instantaneous deteriorating items (NIDIs), highlighting sustainability issues, environmental impact, and socio-economic changes in academia and industry. High complexity, continuous processes, integrated dynamics, and adaptability issues challenge the sustainable decision-making process for NIDIs’. Hence, the United Nations has directed 17 Sustainable Development Goals (SDGs) to overcome this ambiguity. This paper examines the challenges in monitoring the targets outlined in SDG 2 (2.3, 2.4, 2(a), 2(b), and 2(c)) and SDG 12 (12.1, 12.3, 12.5, 12.6, 12.7, and 12(a)) of the United Nations’s 2030 goals. The proposed goals could effectively address inventory stocks, appropriate policy selections, perishability, and stochastic market demand. Therefore, this study develops a novel framework by hand-mapping the SDGs and their targets with NIDIs sustainability practices, reflected in its environmental, social, and governance aspects. This paper also includes a systematic literature review (2006 to 2022) to identify sustainable models of NIDIs along with variables, barriers, different mathematical programming approaches, optimal performance criteria, and proposed application framework. Moreover, the findings offer a dual contribution: aiding academic analysis of NIDIs about SDGs and proposing a sustainable modeling framework for practitioners, fostering stakeholder collaboration, and integrating current research trends and agendas for future research directions.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

( Source Scopus database)

Ahmad, B., & Benkherouf, L. (2018). Economic-order-type inventory models for non-instantaneous deteriorating items and backlogging. RAIRO—Operations Research, 52 (3), 895–901.
Article Google Scholar
Ai, X.-Y., Zhang, J.-L., & Wang, L. (2017). Optimal joint replenishment policy for multiple non-instantaneous deteriorating items. International Journal of Production Research, 55 (16), 4625–4642.
Ai, X.-Y., Zhang, J.-L., Xu, H.-X., & Wang, L. (2018). Optimal joint replenishment policy for multiple non-instantaneous deteriorating products with deterioration-time-dependent demand. Kongzhi Yu Juece/control and Decision, 33 (4), 671–678.
Google Scholar
Akhtar, M., Manna, A. K., & Bhunia, A. K. (2023). Optimization of a non-instantaneous deteriorating inventory problem with time and price-dependent demand over a finite time horizon via a hybrid DESGO algorithm. Expert Systems with Applications . https://doi.org/10.1016/j.eswa.2022.118676
Aliabadi, L., Yazdanparast, R., & Nasiri, M. M. (2018). An inventory model for non-instantaneous deteriorating items with credit period and carbon emission sensitive demand: A signal geometric programming approach. International Journal of Management Science and Engineering Management . https://doi.org/10.1080/17509653.2018.1504331
Almathkour, F., & Benkherouf, L. (2022). Optimal policies for finite horizon model with time-varying demand rate, non-instantaneous deterioration, and backlogging. International Journal of Systems Science Operations and Logistics . https://doi.org/10.1080/23302674.2022.2041128
Aly, E., Elsawah, S., & Ryan, M. J. (2022). A review and catalogue to the use of models in enabling the achievement of sustainable development goals (SDG). Journal of cleaner production, 340, 130803
Ardra, S., & Barua, M. K. (2022). Halving food waste generation by 2030: The challenges and strategies of monitoring UN sustainable development goal target 12.3. Journal of Cleaner Production, 380 , 135042.
Bakker, M., Riezebos, J., & Teunter, RuudH. (2012). Review of inventory systems with deterioration since 2001. European Journal of Operational Research, 221 , 275–284.
Bardhan, S., Pal, H., Giri, B.C. (2017). Optimal replenishment policy and preservation technology investment for a non-instantaneous deteriorating item with stock-dependent demand. Operational Research, pp. 1–22.
Becerra, P., Mula, J., & Sanchis, R. (2021). Green supply chain quantitative models for sustainable inventory management: A review. Journal of Cleaner Production, 328 , 129544.
Biglari, S., Beiglary, S., & Arthanari, T. (2022). Achieving sustainable development goals: Fact or fiction?. Journal of Cleaner Production, 332 , 130032.
Burek, J., & Nutter, D. (2018). Life cycle assessment of grocery, perishable, and general merchandise multi-facility distribution center networks. Energy and Buildings, 174 , 388-401.
Cao, Y., Li, Y. M., & Li, Q. S. (2018). Research on pricing and inventory lot-size policies for non-instantaneous deteriorating items with stochastic demand and promotional efforts based on advance payments. Control and Decision, 33 (2), 301–308.
Chakraborty, D., Garai, T., Jana, D. K., & Roy, T. K. (2017). A three-layer supply chain inventory model for non-instantaneous deteriorating items with inflation and delay in payments in a random fuzzy environment. Journal of Industrial and Production Engineering, 34 (6), 407–424.
Chang, C.-T., Cheng, M.-C., & Ouyang, L.-Y. (2011). Optimal pricing and ordering policies for non-instantaneously deteriorating items under order-size-dependent payment delay. Applied Mathematical Modelling, 39 (2), 747–763.
Chang, C.-T., Teng, J.-T., & Goyal, S. K. (2010). Optimal replenishment policies for non-instantaneous deteriorating items with stock-dependent demand. International Journal of Production Economics, 123 (1), 62–68.
Chang, H. J., & Lin, W. F. (2010). A partial backlogging inventory model for non-instantaneous deteriorating items with stock-dependent consumption rate under inflation. Yugoslav Journal of Operations Research, 20 (1), 35–54.
Chapman, C. B., Ward, S. C., Cooper, D. F., & Page, M. J. (1984). Credit policy and inventory control. Journal of Operational Research Society, 35 (12), 1055–1065.
Chatterjee, S., Chaudhuri, R., Shah, M., & Maheshwari, P. (2022). Big data driven innovation for sustaining SME supply chain operation in post COVID-19 scenario: Moderating role of SME technology leadership. Computers & Industrial Engineering, 168 , 108058. https://doi.org/10.1016/j.cie.2022.108058
Chung, K.-J. (2009). A complete proof of the solution procedure for non-instantaneous deteriorating items with permissible delay in payment. Computers and Industrial Engineering, 56 (1), 267–273.
Chung, K.-J. (2010). Using the convexities of total annual relevant costs to determine the optimal cycle times of inventory models for deteriorating items with permissible delay in payments. Computers and Industrial Engineering, 58 (4), 801–808.
Chung, K.-J., Cárdenas-Barrón, L. E., & Ting, P.-S. (2014). An inventory model with non-instantaneous receipt and exponentially deteriorating items for an integrated three layer supply chain system under two levels of trade credit. International Journal of Production Economics, 155 , 310–317.
Daghigh, R., Jabalameli, M., Amiri, A., & Pishvaee, M. (2016). A multi-objective location-inventory model for 3PL providers with sustainable considerations under uncertainty. International Journal of Industrial Engineering Computations, 7 (4), 615–634.
Das, S. C., Manna, A. K., Rahman, M. S., Shaikh, A. A., & Bhunia, A. K. (2021). An inventory model for non-instantaneous deteriorating items with preservation technology and multiple credit periods-based trade credit financing via particle swarm optimization. Soft Computing, 25 (7), 5365–5384. https://doi.org/10.1007/s00500-020-05535-x
Dye, C.-Y. (2013). The effect of preservation technology investment on a non-instantaneous deteriorating inventory model. Omega (united Kingdom), 41 (5), 872–880.
Farughi, H., Khanlarzade, N., & Yegane, B. Y. (2014). Pricing and inventory control policy for non-instantaneous deteriorating items with time- and price-dependent demand and partial backlogging. Decision Science Letters, 3 (3), 325–334.
Galal, N. M., & El-Kilany, K. S. (2016). Sustainable agri-food supply chain with uncertain demand and lead time. International Journal of Simulation Modelling, 15 (3), 485–496.
Garg, C. P. (2022). Modelling and optimisation of reverse logistics network under fuzzy environment. International Journal of Operational Research, 44 (3), 360–388.
Geetha, K. V., & Uthayakumar, R. (2009). Optimal inventory control policy for items with time-dependent demand. American Journal of Mathematical and Management Sciences, 29 (3–4), 457–476.
Geetha, K. V., & Uthayakumar, R. (2010). Economic design of an inventory policy for non-instantaneous deteriorating items under permissible delay in payments. Journal of Computational and Applied Mathematics, 233 (10), 2492–2505.
Ghasemi, N. (2015). Developing EPQ models for non-instantaneous deteriorating items. Journal of Industrial Engineering International, 11 (3), 427–437.
Ghobadi, S. N., Kamalabadi, I. N., & Aghdasi, M. (2012). Joint pricing and inventory control for non instantaneous deteriorating items with stochastic demand. International Journal of Supply Chain Management, 1 (3), 43–53.
Ghoreishi, M., Mirzazadeh, A., & Kamalabadi, I. N. (2014a). Optimal pricing and lot-sizing policies for an economic production quantity model with non-instantaneous deteriorating items, permissible delay in payments, customer returns, and inflation. Proceedings of the Institution of Mechanical Engineers, Part B: Journal of Engineering Manufacture, 228 (12), 1653–1663.
Ghoreishi, M., Mirzazadeh, A., & Weber, G.-W. (2013). Optimal pricing and ordering policy for non-instantaneous deteriorating items under inflation and customer returns. Optimization, 63 (12), 1785–1804.
Ghoreishi, M., Weber, G.-W., & Mirzazadeh, A. (2014b). An inventory model for non-instantaneous deteriorating items with partial backlogging, permissible delay in payments, inflation- and selling price-dependent demand and customer returns. Annals of Operations Research, 226 (1), 221–238.
Gite, S. P. (2011). An inventory model for deteriorating items with stock-dependent demand under inflation and time value of money. International Journal of Agricultural and Statistical Sciences, 7 (2), 463–471.
Gor, A. S., & Patel, H. R. (2018). Optimal selling price and lot size for non-instantaneous deteriorating items with different demand rates and partial backlogging. International Journal of Procurement Management, 11 (3), 295–312.
Goyal, A. K., & Chauhan, A. (2016). An EOQ model for deteriorating items with selling price dependent demand rate with learning effect. Nonlinear Studies, 23 (4), 543–552.
Goyal, S. K., & Giri, B. C. (2001). Recent trends in modeling of deteriorating inventory. European Journal of operational research, 134 (1), 1–16.
Goyal, K., & Kumar, S. (2021). Financial literacy: A systematic review and bibliometric analysis. International Journal of Consumer Studies, 45 (1), 80–105.
Hao, J., Chen, G., Chen, P., Yao, Y., & Zhang, Y. (2013). An inventory model for non-instantaneous deteriorating items under two levels of trade credit and time value of money. Journal of Theoretical and Applied Information Technology, 48 (1), 87–93.
Hasan, M. R., Daryanto, Y., Roy, T. C., & Feng, Y. (2020). Inventory management with online payment and preorder discounts. Industrial Management and Data Systems, 120 (11), 2001–2023. https://doi.org/10.1108/IMDS-05-2020-0314
Hasan, S. T., Wood, M. O., & Singh, S. (2022). Revealing embedded carbon emissions within the comprehensive and progressive agreement for trans-pacific partnership. Economic Systems Research, 34 (3), 294–319.
He, Y., Gong, Y., & Hong, X. (2022). Demand information acquisition and disclosure in a non-instantaneous deteriorating items supply chain. Computers and Industrial Engineering . https://doi.org/10.1016/j.cie.2022.108250
Hosseini, Z. S., Flapper, S. D., & Pirayesh, M. (2022). Sustainable supplier selection and order allocation under demand, supplier availability and supplier grading uncertainties. Computers & Industrial Engineering, 165 , 107811.
Jaggi, C. K., Goel, S. K., & Tiwari, S. (2017a). Two-warehouse inventory model for non-instantaneous deteriorating items under different dispatch policies. Investigation Operational, 38 (4), 343–365.
Jaggi, C. K., Sharma, A., & Tiwari, S. (2015a). Credit financing in economic ordering policies for non-instantaneous deteriorating items with price dependent demand under permissible delay in payments: A new approach. International Journal of Industrial Engineering Computations, 6 (4), 481–502.
Jaggi, C. K., Tiwari, S., & Goel, S. K. (2016). Replenishment policy for non-instantaneous deteriorating items in a two storage facilities under inflationary conditions. International Journal of Industrial Engineering Computations, 7 (3), 489–506.
Jaggi, C. K., Tiwari, S., & Goel, S. K. (2017b). Credit financing in economic ordering policies for non-instantaneous deteriorating items with price dependent demand and two storage facilities. Annals of Operations Research, 248 (1–2), 253–280.
Jaggi, C. K., & Verma, P. (2010). An optimal replenishment policy for non-instantaneous deteriorating items with two storage facilities. International Journal of Services Operations and Informatics, 5 (3), 209–230.
Jaggi, C. K., Verma, P., & Gupta, M. (2015b). Ordering policy for non-instantaneous deteriorating items in two warehouse environment with shortages. International Journal of Logistics Systems and Management, 22 (1), 103–124.
Janssen, T. C., & Sauer, J. (2016). Literature review of deteriorating inventory models by key topics from 2012 to 2015. International Journal of Production Economics, 182 , 86–112.
Johri, A., Joshi, P., Kumar, S., & Joshi, G. (2024). Metaverse for sustainable development in a bibliometric analysis and systematic literature review. Journal of Cleaner Production, 435 , 140610.
Kamble, S., Gunasekaran, A., & Shradha, G. (2019). Achieving sustainable performance in a data-driven agriculture supply chain: A review for research and applications. International Journal of Production Economics . https://doi.org/10.1016/j.ijpe.2019.05.022
Kaur, J., Sharma, R., & Singh, A. P. (2013). An optimal ordering policy for inventory model with non-instantaneous deteriorating items and stock-dependent demand. Applied Mathematical Sciences, 7 (81–84), 4073–4080.
Krommyda, I.-P., Skouri, K., Konstantaras, I., & Ganas, I. (2013). Optimal pricing and replenishment policy for non instantaneous deteriorating items and two levels of storage. Asia-Pacific Journal of Operational Research, 30 (4), 1350001.
Kumar, N., Singh, S. R., & Kumari, R. (2012). Three echelon supply chain inventory model for deteriorating items with limited storage facility and lead-time under inflation. International Journal of Services and Operations Management, 13 (1), 98–118.
Kumar, N., Singh, S. R., & Kumari, R. (2013). Learning effect on an inventory model with two-level storage and partial backlogging under inflation. International Journal of Services and Operations Management, 16 (1), 105–122.
Kumar, S., Colombage, S., & Rao, P. (2017). Research on capital structure determinants: A review and future directions. International Journal of Managerial Finance, 13 (2), 106–132.
Kumar, S., & Rajput, U. S. (2014). A two warehouse inventory model for non-instantaneous deteriorating items with time dependent demand and partial backlogging. International Journal of Applied Engineering Research, 9 (11 SPEC ISSUE), 1347–1356.
Kumar, S., & Singh, A. K. (2015). An optimal replenishment policy for non instantaneous deteriorating items with stock dependent, price decreasing demand and partial backlogging. Indian Journal of Science and Technology, 8 (35), 12.
La Scalia, G., Micale, R., Miglietta, P. P., & Toma, P. (2019). Reducing waste and ecological impacts through a sustainable and efficient management of perishable food based on the Monte Carlo simulation. Ecological Indicators, 97 , 363–371.
Lashgari, M., Taleizadeh, A.A., & Ahmadi, A. (2016). Partial up-stream advanced payment and partial down-stream delayed payment in a three-level supply chain. Annals of Operations Research, 238 , 329–354.
Lashgari, M., Taleizadeh, A. A., & Sadjadi, S. J. (2018). Ordering policies for non-instantaneous deteriorating items under hybrid partial prepayment, partial trade credit and partial backordering. Journal of the Operational Research Society, 69 (8), 1167–1196.
Li, J., Lai, K. K., & Li, Y. (2022). Remanufacturing and low-carbon investment strategies in a closed-loop supply chain under multiple carbon policies. International Journal of Logistics Research and Applications, 1–23.
Li, G., He, X., Zhou, J., & Wu, H. (2019). Pricing, replenishment and preservation technology investment decisions for non-instantaneous deteriorating items. Omega (united Kingdom), 84 , 114–126.
Lim, M. K., Bahr, W., & Leung, S. C. (2013). RFID in the warehouse: A literature analysis (1995–2010) of its applications, benefits, challenges and future trends. International Journal of Production Economics, 145 (1), 409–430.
Mahato, C., & Mahata, G. C. (2022). Optimal replenishment, pricing and preservation technology investment policies for non-instantaneous deteriorating items under two-level trade credit policy. Journal of Industrial and Management Optimization, 18 (5), 3499–3537. https://doi.org/10.3934/jimo.2021123
Maheshwari, P., & Kamble, S. (2022). the application of supply chain digital twin to measure optimal inventory policy. IFAC-PapersOnLine, 55 (10), 2324–2329. https://doi.org/10.1016/j.ifacol.2022.10.055
Maheshwari, P., Kamble, S., Pundir, A., Belhadi, A., Ndubisi, N. O., & Tiwari, S. (2021). Internet of things for perishable inventory management systems: an application and managerial insights for micro, small and medium enterprises. Annals of Operations Research . https://doi.org/10.1007/s10479-021-04277-9
Maihami, R., Ghalehkhondabi, I., & Ahmadi, E. (2021). Pricing and inventory planning for non-instantaneous deteriorating products with greening investment: A case study in beef industry. Journal of Cleaner Production . https://doi.org/10.1016/j.jclepro.2021.126368
Maihami, R., & Karimi, B. (2014). Optimizing the pricing and replenishment policy for non-instantaneous deteriorating items with stochastic demand and promotional efforts. Computers and Operations Research, 51 , 302–312.
Maihami, R., Karimi, B., & Fatemi Ghomi, S. M. T. (2017). Effect of two-echelon trade credit on pricing-inventory policy of non-instantaneous deteriorating products with probabilistic demand and deterioration functions. Annals of Operations Research, 257 (1–2), 237–273.
Magnanini, M. C., & Tolio, T. (2018). A threshold-based control policy for scrap reduction of perishable in-process inventories. Procedia CIRP, 78 , 184–189.
Maihami, R., & Nakhai Kamalabadi, I. (2012). Joint pricing and inventory control for non-instantaneous deteriorating items with partial backlogging and time and price dependent demand. International Journal of Production Economics, 136 (1), 116–122.
Malladi, K. T., & Sowlati, T. (2018). Sustainability aspects in inventory routing problem: A review of new trends in the literature. Journal of Cleaner Production, 197 , 804–814.
Manna, S. K., Lee, C. C., & Chiang, C. (2009). EOQ model for non-instantaneous deteriorating items with time-varying demand and partial backlogging. International Journal of Industrial and Systems Engineering, 4 (3), 241–254.
Mishra, U., Wu, J. Z., Tsao, Y. C., & Tseng, M. L. (2020). Sustainable inventory system with controllable non-instantaneous deterioration and environmental emission rates. Journal of Cleaner Production . https://doi.org/10.1016/j.jclepro.2019.118807
Mishra, V. K. (2014). Deteriorating inventory model with controllable deterioration rate for time-dependent demand and time-varying holding cost. Yugoslav Journal of Operations Research, 24 (1), 87–98.
Mohanty, D. J., Kumar, R. S., & Goswami, A. (2016). A two-warehouse inventory model for non-instantaneous deteriorating items over stochastic planning horizon. Journal of Industrial and Production Engineering, 33 (8), 516–532.
Mu, X., & Antwi-Afari, M. F. (2024). The applications of Internet of Things (IoT) in industrial management: A science mapping review. International Journal of Production Research, 62 (5), 1928–1952.
Nagare, M., Dutta, P., & Suryawanshi, P. (2017). Optimal procurement and discount pricing for single-period non-instantaneous deteriorating products with promotional efforts. Operational Research, 20 , 1–29.
Nagare, M., Dutta, P., & Suryawanshi, P. (2020). Optimal procurement and discount pricing for single-period non-instantaneous deteriorating products with promotional efforts. Operational Research, 20 (1), 89–117. https://doi.org/10.1007/s12351-017-0318-5
Nahmias, S. (1982). Perishable inventory theory: A review. Operations research, 30 (4), 680–708.
Nylund, P. A., Agarwal, N., Probst, C., & Brem, A. (2022). Firm engagement in UN sustainable development goals: Introduction of a constraints map from a corporate reports content analysis. Journal of Cleaner Production, 371 , 133446.
Ouyang, L.-Y., Wu, K.-S., & Yang, C.-T. (2006). A study on an inventory model for non-instantaneous deteriorating items with permissible delay in payments. Computers and Industrial Engineering, 51 (4), 637–651.
Ouyang, L.-Y., Wu, K.-S., & Yang, C.-T. (2008). Retailer’s ordering policy for non-instantaneous deteriorating items with quantity discount, stock-dependent demand and stochastic backorder rate. Journal of the Chinese Institute of Industrial Engineers, 25 (1), 62–72.
Pal, H., Bardhan, S., & Giri, B. C. (2018). Optimal replenishment policy for non-instantaneously perishable items with preservation technology and random deterioration start time. International Journal of Management Science and Engineering Management, 13 (3), 188–199.
Palanivel, M., Mirzazadeh, A., Weber, G.-W., & Nakhai-Kamalabadi, I. (2014). Joint pricing and replenishment decisions for non-instantaneous deteriorating items with partial backlogging, inflation- and selling price-dependent demand and customer returns. Journal of Industrial and Management Optimization, 11 (3), 933–949.
Palanivel, M., Priyan, S., & Mala, P. (2018). Two-warehouse system for non-instantaneous deterioration products with promotional effort and inflation over a finite time horizon. Journal of Industrial Engineering International, 14 (3), 603–612.
Palanivel, M., Sundararajan, R., & Uthayakumar, R. (2016). Two-warehouse inventory model with non-instantaneously deteriorating items, stock-dependent demand, shortages and inflation. Journal of Management Analytics, 3 (2), 152–173.
Palanivel, M., & Uthayakumar, R. (2015). Finite horizon EOQ model for non-instantaneous deteriorating items with price and advertisement dependent demand and partial backlogging under inflation. International Journal of Systems Science, 46 (10), 1762–1773.
Palanivel, M., & Uthayakumar, R. (2016a). Finite horizon EOQ model for non-instantaneous deteriorating items with probabilistic deterioration and partial backlogging under inflation. International Journal of Mathematics in Operational Research, 8 (4), 449–476.
Palanivel, M., & Uthayakumar, R. (2016b). Two-warehouse inventory model for non-instantaneous deteriorating items with stock dependent demand, partial backlogging and inflation over a finite time horizon. International Journal of Services and Operations Management, 25 (2), 206–235.
Palanivel, M., & Uthayakumar, R. (2016c). Two-warehouse inventory model for non-instantaneous deteriorating items with partial backlogging and inflation over a finite time horizon. Opsearch, 53 (2), 278–302.
Palanivel, M., & Uthayakumar, R. (2016d). Two-warehouse inventory model for non–instantaneous deteriorating items with optimal credit period and partial backlogging under inflation. Journal of Control and Decision, 3 (2), 132–150.
Palanivel, M., & Uthayakumar, R. (2017a). Two-warehouse inventory model for non-instantaneous deteriorating items with partial backlogging and permissible delay in payments under inflation. International Journal of Operational Research, 28 (1), 35–69.
Palanivel, M., & Uthayakumar, R. (2017b). An EOQ model for non-instantaneous deteriorating items with partial backlogging and permissible delay in payments under inflation. International Journal of Industrial and Systems Engineering, 26 (1), 63–89.
Pasandideh, S. H. R., Rahbari, M., & Sadati-Keneti, Y. (2023). A Lagrangian relaxation algorithm and hybrid genetic algorithm-black widow optimization for perishable products supply chain with sustainable development goals consideration. Annals of Operations Research, 1–36.
Patel, H., Gor, A. (2018). Salvage value and three variable Weibull deteriorating rate for non-instantaneous deteriorating items.Asian-European Journal of Mathematics, 12(1).
Pérez, F. A., Torres, F., & Mendoza, D. (2019). Stocking and price-reduction decisions for non-instantaneous deteriorating items under time value of money. International Journal of Industrial Engineering Computations, 10 (1), 89–110.
Pundir, A., Devpriya, J., Chakraborty, M., Ganpathy, L. (2019b). Technology integration for improved performance: a case study in digitization of supply chain with integration of internet of things and blockchain technology. In: 2019 IEEE 9th Annual computing and communication workshop and conference (CCWC), Las Vegas, NV, USA, 2019, pp. 0170-0176.
Pundir, A., Jagannath, D., Ganapathy, L. (2019a). Improving supply chain visibility using IoT-Internet of Things. In: IEEE 9th Annual computing and communication workshop and conference (CCWC), Las Vegas, NV, USA, 2019, pp. 0156-0162.
Punj, N., Ahmi, A., Tanwar, A., & Rahim, S. A. (2023). Mapping the field of green manufacturing: A bibliometric review of the literature and research frontiers. Journal of Cleaner Production, 423 , 138729.
Raafat, F. (1991). Survey of literature on continuously deteriorating inventory models. Journal of the Operational Research society, 42 (1), 27–37.
Rabbani, M., Zia, N. P., & Rafiei, H. (2015). Coordinated replenishment and marketing policies for non-instantaneous stock deterioration problem. Computers and Industrial Engineering, 88 , 49–62.
Rabbani, M., Zia, N. P., & Rafiei, H. (2017). Joint optimal inventory, dynamic pricing and advertisement policies for non-instantaneous deteriorating items. RAIRO - Operations Research, 51 (4), 1251–1267.
Rangarajan, K., & Karthikeyan, K. (2017). EOQ models for non-instantaneous/instantaneous deteriorating items with cubic demand rate under inflation and permissible delay in payments. Italian Journal of Pure and Applied Mathematics, 37 , 197–218.
Rapolu, C. N., & Kandpal, D. H. (2020). Joint pricing, advertisement, preservation technology investment and inventory policies for non-instantaneous deteriorating items under trade credit. Opsearch, 57 (2), 274–300. https://doi.org/10.1007/s12597-019-00427-7
Rastogi, M., Kushwah, P., & Singh, S. R. (2018). An inventory model for non-instantaneous deteriorating products having price sensitive demand and partial backlogging of occurring shortages. International Journal of Operations and Quantitative Management, 24 (1), 59–73.
Rezagholifam, M., Sadjadi, S. J., Heydari, M., & Karimi, M. (2022). Optimal pricing and ordering strategy for non-instantaneous deteriorating items with price and stock sensitive demand and capacity constraint. International Journal of Systems Science: Operations and Logistics, 9 (1), 121–132. https://doi.org/10.1080/23302674.2020.1833259
Samanta, A., & Pal, M. (2015). Periodic review inventory policy for non-instantaneous deteriorating items with time dependent deterioration rate. Pakistan Journal of Statistics and Operation Research, 11 (3), 409–419.
Saunders, M. N., & Bezzina, F. (2016). Reflections on conceptions of research methodology among management academics. European Management Journal, 33 (5), 297–304.
Shah, N. H., Soni, H. N., & Patel, K. A. (2013). Optimizing inventory and marketing policy for non-instantaneous deteriorating items with generalized type deterioration and holding cost rates. Omega (united Kingdom), 41 (2), 421–430.
Shaikh, A. A., Cárdenas-Barrón, L. E., & Tiwari, S. (2017). A two-warehouse inventory model for non-instantaneous deteriorating items with interval-valued inventory costs and stock-dependent demand under inflationary conditions. Neural Computing and Applications, 31 , 1–18.
Singh, S. R., & Rathore, H. (2014). An inventory model for deteriorating item with reliability consideration and trade credit. Pakistan Journal of Statistics and Operation Research, 10 (3), 349–360.
Singh, S., Singh, S. R., & Sharma, S. (2017). A partially backlogged EPQ model with demand dependent production and non-instantaneous deterioration. International Journal of Mathematics in Operational Research, 10 (2), 211–228.
Skaf, L., Franzese, P. P., Capone, R., & Buonocore, E. (2021). Unfolding hidden environmental impacts of food waste: An assessment for fifteen countries of the world. Journal of Cleaner Production, 310 , 127523.
Soni, H. N. (2013). Optimal replenishment policies for non-instantaneous deteriorating items with price and stock sensitive demand under permissible delay in payment. International Journal of Production Economics, 146 (1), 259–268.
Soni, H. N., Gor, A. S., & Patel, H. R. (2018). Vendor managed inventory model for non-instantaneous deteriorating product with quadratic demand allowing partial backlogging. Uncertain Supply Chain Management, 6 (3), 321–334.
Soni, H. N., & Patel, K. A. (2012). Optimal pricing and inventory policies for non-instantaneous deteriorating items with permissible delay in payment: Fuzzy expected value model. International Journal of Industrial Engineering Computations, 3 (3), 281–300.
Soni, H. N., & Patel, K. A. (2013). Joint pricing and replenishment policies for non-instantaneous deteriorating items with imprecise deterioration free time and credibility constraint. Computers and Industrial Engineering, 66 (4), 944–951.
Soni, H. N., & Suthar, D. N. (2018). Pricing and inventory decisions for non-instantaneous deteriorating items with price and promotional effort stochastic demand. Journal of Control and Decision . https://doi.org/10.1080/23307706.2018.1478327
Soni, H. N., & Suthar, D. N. (2020). Optimal pricing and replenishment policy for non-instantaneous deteriorating items with varying rate of demand and partial backlogging. Opsearch, 57 (3), 986–1021. https://doi.org/10.1007/s12597-020-00451-y
Sugapriya, C., & Jeyaraman, K. (2008). An EPQ model for non-instantaneous deteriorating item in which holding cost varies with time. Electronic Journal of Applied Statistical Analysis, 1 (1), 16–23.
Sundararajan, R., Palanivel, M., & Uthayakumar, R. (2021). An EOQ model of non-instantaneous deteriorating items with price, time-dependent demand and backlogging. Journal of Control and Decision, 8 (2), 135–154. https://doi.org/10.1080/23307706.2019.1656560
Tashakkor, N., Mirmohammadi, S. H., & Iranpoor, M. (2018). Joint optimization of dynamic pricing and replenishment cycle considering variable non-instantaneous deterioration and stock-dependent demand. Computers and Industrial Engineering, 123 , 232–241.
Tat, R., Taleizadeh, A. A., & Esmaeili, M. (2013). Developing economic order quantity model for non-instantaneous deteriorating items in vendor-managed inventory (VMI) system. International Journal of Systems Science, 46 (7), 1257–1268
Tat, R., Taleizadeh, A. A., & Esmaeili, M. (2015). Developing economic order quantity model for non-instantaneous deteriorating items in vendor-managed inventory (VMI) system. International Journal of Systems Science, 46 (7), 1257–1268.
Tayal, S., Singh, S. R., Sharma, R., & Singh, A. P. (2015). An EPQ model for non-instantaneous deteriorating item with time dependent holding cost and exponential demand rate. International Journal of Operational Research, 23 (2), 145–162.
Tayyab, M., Habib, M. S., Jajja, M. S. S., & Sarkar, B. (2022). Economic assessment of a serial production system with random imperfection and shortages: A step towards sustainability. Computers & Industrial Engineering, 171 , 108398.
Thangam, A., & Uthayakumar, R. (2008). Evaluation of supply chain structures using a delayed product differentiation process. International Journal of Advanced Manufacturing Technology, 39 (3–4), 401–408.
Ting, P.-S., & Chung, K.-J. (1994). Inventory replenishment policy for deteriorating items with a linear trend in demand considering shortages. International Journal of Operations & Production Management, 14 (8), 102–110.
Tiwari, S., Cárdenas-Barrón, L. E., Khanna, A., & Jaggi, C. K. (2016). Impact of trade credit and inflation on retailer’s ordering policies for non-instantaneous deteriorating items in a two-warehouse environment. International Journal of Production Economics, 176 , 154–169.
Tiwari, S., Jaggi, C. K., Bhunia, A. K., Shaikh, A. A., & Goh, M. (2017). Two-warehouse inventory model for non-instantaneous deteriorating items with stock-dependent demand and inflation using particle swarm optimization. Annals of Operations Research, 254 (1–2), 401–423.
Tiwari, S., Jaggi, C. K., Gupta, M., & Cárdenas-Barrón, L. E. (2018). Optimal pricing and lot-sizing policy for supply chain system with deteriorating items under limited storage capacity. International Journal of Production Economics, 200 , 278–290.
Tranfield, D., Denyer, D., & Smart, P. (2006). Towards a methodology for developing evidence-informed management knowledge by means of systematic review. British Journal of Management, 14 , 207–222.
Tripathy, M., Sharma, G., & Sharma, A. K. (2022). An EOQ inventory model for non-instantaneous deteriorating item with constant demand under progressive financial trade credit facility. Opsearch, 59 (4), 1215–1243. https://doi.org/10.1007/s12597-022-00573-5
Tsao, Y.-C. (2016). Joint location, inventory, and preservation decisions for non-instantaneous deterioration items under delay in payments. International Journal of Systems Science, 47 (3), 572–585.
Tsao, Y.-C., Zhang, Q., Fang, H.-P., & Lee, P.-L. (2017). Two-tiered pricing and ordering for non-instantaneous deteriorating items under trade credit. Operational Research, 19 , 1–20.
Tyagi, A. P., Pandey, R. K., & Singh, S. (2014). An optimal replenishment policy for non-instantaneous deteriorating items with stock-dependent demand and variable holding cost. International Journal of Operational Research, 21 (4), 466–488.
Udayakumar, R. (2022). An EOQ model for non-instantaneous deteriorating items with time-dependent demand under partial backlogging. Journal of Management Analytics . https://doi.org/10.1080/23270012.2022.2073571
Udayakumar, R., & Geetha, K. V. (2017). Economic ordering policy for single item inventory model over finite time horizon. International Journal of Systems Assurance Engineering and Management, 8 , 734–757.
Udayakumar, R., & Geetha, K. V. (2018). An EOQ model for non-instantaneous deteriorating items with two levels of storage under trade credit policy. Journal of Industrial Engineering International, 14 (2), 343–365.
UN. (2022). Transforming our world: the 2030 agenda for sustainable development. division for sustainable development goals, New York, NY, USA. https://unstats.un.org/sdgs/report/2022/ .
Uthayakumar, R., & Geetha, K. V. (2009a). Replenishment policy for single item inventory model with money inflation. Opsearch, 46 (3), 345–357.
Uthayakumar, R., & Geetha, K. V. (2009b). A replenishment policy for non-instantaneous deteriorating inventory system with partial backlogging. Tamsui Oxford Journal of Mathematical Sciences, 25 (3), 313–332.
Valliathal, M., & Uthayakumar, R. (2011). Optimal pricing and replenishment policies of an EOQ model for non-instantaneous deteriorating items with shortages. International Journal of Advanced Manufacturing Technology, 54 (1–4), 361–371.
Valliathal, M., & Uthayakumar, R. (2012). Designing retailer’s replenishment policies for non-instantaneous deteriorating items under fuzzy costs. International Journal of Services and Operations Management, 13 (4), 415–440.
Valliathal, M., & Uthayakumar, R. (2013). Designing and computing optimal policies on a production model for non-instantaneous deteriorating items with shortages. International Journal of Production Research, 51 (1), 215–229.
Valliathal, M., & Uthayakumar, R. (2016). Optimal replenishment policies of an EOQ model for non-instantaneous Weibull deteriorating items with ramp-type of demand under shortages. International Journal of Mathematics in Operational Research, 8 (1), 60–86.
VandanaSharma, B. K. (2016). An inventory model for non-instantaneous deteriorating items with quadratic demand rate and shortages under trade credit policy. Journal of Applied Analysis and Computation, 6 (3), 720–737.
Wang, Y., Zhang, J., & Tang, W. (2015). Dynamic pricing for non-instantaneous deteriorating items. Journal of Intelligent Manufacturing, 26 (4), 629–640.
Wu, J., Skouri, K., Teng, J.-T., & Ouyang, L.-Y. (2014). A note on “optimal replenishment policies for non-instantaneous deteriorating items with price and stock sensitive demand under permissible delay in payment.” International Journal of Production Economics, 155 , 324–329.
Wu, K.-S., Ouyang, L.-Y., & Yang, C.-T. (2006). An optimal replenishment policy for non-instantaneous deteriorating items with stock-dependent demand and partial backlogging. International Journal of Production Economics, 101 (2), 369–384.
Wu, K.-S., Ouyang, L.-Y., & Yang, C.-T. (2009). Coordinating replenishment and pricing policies for non-instantaneous deteriorating items with price-sensitive demand. International Journal of Systems Science, 40 (12), 1273–1281.
Xu, T.-T., & Xiao, T.-J. (2013). Coordination of supply chain with a non-instantaneous deteriorating item based on quantity discount policy. Xitong Gongcheng Lilun Yu Shijian/system Engineering Theory and Practice, 33 (7), 1690–1698.
Xu, Z., Peng, J., Qiu, S., Liu, Y., Dong, J., & Zhang, H. (2022). Responses of spatial relationships between ecosystem services and the sustainable development goals to urbanization. Science of the Total Environment, 850 , 157868.
Yang, C.-T., Ouyang, L.-Y., & Wu, H.-H. (2009). Retailer’s optimal pricing and ordering policies for non-instantaneous deteriorating items with price-dependent demand and partial backlogging. Mathematical Problems in Engineering, 2009 , 198305.
Zhang, J., Wang, Y., Lu, L., & Tang, W. (2015). Optimal dynamic pricing and replenishment cycle for non-instantaneous deterioration items with inventory-level-dependent demand. International Journal of Production Economics, 170 , 136–145.
Zhang, Y., Wang, Y., & Gong, B. (2016). Quantity discount coordination for deteriorating items supply chain based on non-instantaneous replenishment. Computer Integrated Manufacturing Systems, CIMS, 22 (12), 2858–2866.
Download references
Author information
Authors and affiliations.
Indian Institute of Management Jammu, Jammu, 180016, India
Pratik Maheshwari
EDHEC Business School, Roubaix, France
Sachin Kamble
Rabat Business School, International University of Rabat, Sale, Morocco
Amine Belhadi
Indian Institute of Management Nagpur, Nagpur, India
Satish Kumar
You can also search for this author in PubMed Google Scholar

Corresponding author
Correspondence to Satish Kumar .
Ethics declarations
Conflict of interest.
Author have no conflict of intertest to declare.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1: Comprehensive literature review on NIDIs
Keywords | Deterioration | NIDIs | Demand | Demand-dependent distribution functions | Shortage | Replenishment rate | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Sr. no | Authors name | NIDIs | Single items | Multi items | Deterministic | Stochastic | Stock | Time | Constant | Price | No | Partial | Fully | Infinite | Finite |
1 | Wu et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
2 | Ouyang et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
3 | Ouyang et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
4 | Thangam and Uthayakumar ( ) | √ | √ | √ | √ | ||||||||||
5 | Sugapriya and Jeyaraman ( ) | √ | √ | √ | √ | √ | √ | ||||||||
6 | Geetha and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
7 | Chung ( ) | √ | √ | √ | √ | √ | √ | ||||||||
8 | Manna et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
9 | Uthayakumar and Geetha ( ) | √ | √ | √ | √ | √ | √ | ||||||||
10 | Uthayakumar and Geetha ( ) | √ | √ | √ | √ | √ | √ | ||||||||
11 | Wu et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
12 | Yang et al. ( ) | √ | √ | √ | √ | √ | |||||||||
13 | Chang et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
14 | Geetha and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
15 | Chung ( ) | √ | √ | √ | √ | √ | √ | ||||||||
16 | Jaggi and Verma ( ) | √ | √ | √ | √ | √ | |||||||||
17 | Chang et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
18 | Valliathal and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
19 | Chang et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
20 | Gite ( ) | √ | √ | √ | √ | √ | √ | ||||||||
21 | Ghobadi et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
22 | Maihami and Nakhai Kamalabadi ( ) | √ | √ | √ | √ | √ | √ | ||||||||
23 | Soni and Patel ( ) | √ | √ | √ | √ | √ | √ | ||||||||
24 | Kumar et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
25 | Valliathal and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
26 | Valliathal and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
27 | Ghoreishi et al. ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
28 | Hao et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
29 | Shah et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
30 | Xu and Xiao ( ) | √ | √ | √ | √ | √ | |||||||||
31 | Kaur et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
32 | Krommyda et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
33 | Kumar et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
34 | Dye ( ) | √ | √ | √ | √ | √ | √ | ||||||||
35 | Soni ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
36 | Soni and Patel ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
37 | Singh and Rathore ( ) | √ | √ | √ | √ | √ | √ | ||||||||
38 | Mishra ( ) | √ | √ | √ | √ | √ | √ | ||||||||
39 | Farughi et al. ( ) | √ | √ | √ | √ | √ | |||||||||
40 | Tyagi et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
41 | Kumar and Rajput ( ) | √ | √ | √ | √ | √ | √ | ||||||||
42 | Maihami and Karimi ( ) | √ | √ | √ | √ | √ | √ | ||||||||
43 | Ghoreishi et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
44 | Ghoreishi et al. ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
45 | Palanivel et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
46 | Wu et al. ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
47 | Chung et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
48 | Samanta and Pal ( ) | √ | √ | √ | √ | √ | √ | ||||||||
49 | Jaggi et al. ( , ) | √ | √ | √ | √ | √ | √ | ||||||||
50 | Palanivel and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
51 | Ghasemi ( ) | √ | √ | √ | √ | √ | |||||||||
52 | Tayal et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
53 | Jaggi et al. ( , ) | √ | √ | √ | √ | √ | √ | ||||||||
54 | Tat et al. ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
55 | Rabbani et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
56 | Wang et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
57 | Kumar and Singh ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
58 | Zhang et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
59 | Palanivel and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
60 | Vandana and Sharma ( ) | √ | √ | √ | √ | √ | √ | ||||||||
61 | Palanivel et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
62 | Goyal and Chauhan ( ) | √ | √ | √ | √ | √ | |||||||||
63 | Valliathal and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
64 | Tsao ( ) | √ | √ | √ | √ | √ | |||||||||
65 | Palanivel et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
66 | Palanivel et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
67 | Palanivel and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
68 | Jaggi et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
69 | Tiwari et al. ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
70 | Mohanty et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
71 | Zhang et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
72 | Singh et al. ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
73 | Jaggi et al. ( , ) | √ | √ | √ | √ | √ | √ | ||||||||
74 | Palanivel and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
75 | Rangarajan and Karthikeyan ( ) | √ | √ | √ | √ | √ | √ | ||||||||
76 | Jaggi et al. ( , ) | √ | √ | √ | √ | √ | √ | √ | |||||||
77 | Palanivel and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | ||||||||
78 | Bardhan et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
79 | Tsao et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
80 | Nagare et al. ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
81 | Tiwari et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
82 | Ai et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
83 | Chakraborty et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
84 | Shaikh et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
85 | Maihami et al. ( ) | √ | √ | √ | √ | √ | |||||||||
86 | Rabbani et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
87 | Udayakumar and Geetha ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
88 | Soni et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
89 | Gor and Patel ( ) | √ | √ | √ | √ | √ | √ | ||||||||
90 | Soni et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
91 | Aliabadi et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
92 | Cao et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
93 | Rastogi et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
94 | Ai et al. ( ) | √ | √ | √ | √ | √ | |||||||||
95 | Patel and Gor ( ) | √ | √ | √ | √ | √ | √ | ||||||||
96 | Udayakumar and Geetha ( ) | √ | √ | √ | √ | √ | √ | ||||||||
97 | Ahmad and Benkherouf ( ) | √ | √ | √ | √ | √ | √ | ||||||||
98 | Pal et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
99 | Lashgari et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
100 | Tashakkor et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
101 | Palanivel et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
102 | Pérez et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
103 | Li et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
104 | Akhtar et al. ( ) | √ | √ | √ | √ | √ | |||||||||
105 | Almathkour and Benkherouf ( ) | √ | √ | √ | √ | √ | |||||||||
106 | Das et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
107 | Hasan et al. ( ) | √ | √ | √ | √ | √ | |||||||||
108 | He et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
109 | Mahato and Mahata ( ) | √ | √ | √ | √ | √ | √ | ||||||||
110 | Maihami et al. ( ) | √ | √ | √ | √ | ||||||||||
111 | Mishra et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
112 | Nagare et al. ( ) | √ | √ | √ | √ | √ | √ | √ | |||||||
113 | Rapolu and Kandpal ( ) | √ | √ | √ | √ | √ | |||||||||
114 | Rezagholifam et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
115 | Soni and Suthar ( ) | √ | √ | √ | √ | ||||||||||
116 | Sundararajan et al. ( ) | √ | √ | √ | √ | √ | √ | ||||||||
117 | Maheshwari et al. ( ) | √ | √ | √ | √ | ||||||||||
118 | Tripathy et al. ( ) | √ | √ | √ | √ | √ | |||||||||
119 | Udayakumar ( ) | √ | √ | √ | √ | √ | |||||||||
Keywords | Promotional cost | Lead time | Credit policy | Delay in payment | Rate of inflation | Time value of money | Pricing | Preservation technology | Warehouse | Customer returns | Time horizon | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Sr. no | Authors name | OW | RW | Infinite | Finite | |||||||||
1 | Wu et al. ( ) | √ | √ | |||||||||||
2 | Ouyang et al. ( ) | √ | √ | |||||||||||
3 | Ouyang et al. ( ) | √ | ||||||||||||
4 | Thangam and Uthayakumar ( ) | √ | ||||||||||||
5 | Sugapriya and Jeyaraman ( ) | √ | ||||||||||||
6 | Geetha and Uthayakumar ( ) | √ | ||||||||||||
7 | Chung ( ) | √ | √ | |||||||||||
8 | Manna et al. ( ) | √ | ||||||||||||
9 | Uthayakumar and Geetha ( ) | √ | √ | √ | ||||||||||
10 | Uthayakumar and Geetha ( ) | √ | √ | |||||||||||
11 | Wu et al. ( ) | √ | √ | |||||||||||
12 | Yang et al. ( ) | √ | √ | |||||||||||
13 | Chang et al. ( ) | √ | √ | |||||||||||
14 | Geetha and Uthayakumar ( ) | √ | √ | |||||||||||
15 | Chung ( ) | √ | ||||||||||||
16 | Jaggi and Verma ( ) | √ | √ | √ | ||||||||||
17 | Chang et al. ( ) | √ | √ | |||||||||||
18 | Valliathal and Uthayakumar ( ) | √ | √ | |||||||||||
19 | Chang et al. ( ) | √ | √ | √ | ||||||||||
20 | Gite ( ) | √ | √ | √ | ||||||||||
21 | Ghobadi et al. ( ) | √ | √ | |||||||||||
22 | Maihami and Nakhai Kamalabadi ( ) | √ | √ | |||||||||||
23 | Soni and Patel ( ) | √ | √ | √ | ||||||||||
24 | Kumar et al. ( ) | √ | √ | √ | √ | |||||||||
25 | Valliathal and Uthayakumar ( ) | √ | √ | |||||||||||
26 | Valliathal and Uthayakumar ( ) | √ | ||||||||||||
27 | Ghoreishi et al. ( ) | √ | √ | √ | √ | |||||||||
28 | Hao et al. ( ) | √ | √ | √ | ||||||||||
29 | Shah et al. ( ) | √ | √ | |||||||||||
30 | Xu and Xiao ( ) | √ | ||||||||||||
31 | Kaur et al. ( ) | √ | √ | √ | ||||||||||
32 | Krommyda et al. ( ) | √ | √ | √ | √ | |||||||||
33 | Kumar et al. ( ) | √ | √ | √ | √ | √ | ||||||||
34 | Dye ( ) | √ | √ | |||||||||||
35 | Soni ( ) | √ | ||||||||||||
36 | Soni and Patel ( ) | √ | √ | √ | ||||||||||
37 | Singh and Rathore ( ) | √ | √ | √ | ||||||||||
38 | Mishra ( ) | √ | √ | |||||||||||
39 | Farughi et al. ( ) | √ | √ | |||||||||||
40 | Tyagi et al. ( ) | √ | ||||||||||||
41 | Kumar and Rajput ( ) | √ | √ | √ | ||||||||||
42 | Maihami and Karimi ( ) | √ | √ | √ | ||||||||||
43 | Ghoreishi et al. ( ) | √ | √ | √ | √ | √ | ||||||||
44 | Ghoreishi et al. ( ) | √ | √ | √ | √ | √ | ||||||||
45 | Palanivel et al. ( ) | √ | √ | √ | ||||||||||
46 | Wu et al. ( ) | √ | √ | |||||||||||
47 | Chung et al. ( ) | √ | √ | √ | ||||||||||
48 | Samanta and Pal ( ) | √ | ||||||||||||
49 | Jaggi et al. ( , ) | √ | √ | √ | √ | |||||||||
50 | Palanivel and Uthayakumar ( ) | √ | √ | √ | √ | |||||||||
51 | Ghasemi ( ) | √ | ||||||||||||
52 | Tayal et al. ( ) | √ | ||||||||||||
53 | Jaggi et al. ( , ) | √ | √ | √ | √ | √ | ||||||||
54 | Tat et al. ( ) | √ | ||||||||||||
55 | Rabbani et al. ( ) | √ | √ | √ | ||||||||||
56 | Wang et al. ( ) | √ | √ | |||||||||||
57 | Kumar and Singh ( ) | √ | ||||||||||||
58 | Zhang et al. ( ) | √ | √ | |||||||||||
59 | Palanivel and Uthayakumar ( ) | √ | √ | √ | √ | |||||||||
60 | Vandana and Sharma ( ) | √ | √ | √ | ||||||||||
61 | Palanivel et al. ( ) | √ | √ | √ | √ | |||||||||
62 | Goyal and Chauhan ( ) | √ | √ | |||||||||||
63 | Valliathal and Uthayakumar ( ) | √ | ||||||||||||
64 | Tsao ( ) | √ | √ | √ | √ | |||||||||
65 | Palanivel et al. ( ) | √ | √ | √ | √ | √ | ||||||||
66 | Palanivel et al. ( ) | √ | √ | √ | √ | √ | √ | |||||||
67 | Palanivel and Uthayakumar ( ) | √ | √ | √ | √ | √ | ||||||||
68 | Jaggi et al. ( ) | √ | √ | √ | √ | |||||||||
69 | Tiwari et al. ( ) | √ | √ | √ | √ | √ | ||||||||
70 | Mohanty et al. ( ) | √ | √ | √ | ||||||||||
71 | Zhang et al. ( ) | √ | √ | √ | ||||||||||
72 | Singh et al. ( ) | √ | √ | √ | ||||||||||
73 | Jaggi et al. ( , ) | √ | √ | √ | ||||||||||
74 | Palanivel and Uthayakumar ( ) | √ | √ | √ | √ | √ | √ | √ | ||||||
75 | Rangarajan and Karthikeyan ( ) | √ | √ | √ | √ | |||||||||
76 | Jaggi et al. ( , ) | √ | √ | √ | √ | |||||||||
77 | Palanivel and Uthayakumar ( ) | √ | √ | √ | √ | |||||||||
78 | Bardhan et al. ( ) | √ | √ | |||||||||||
79 | Tsao et al. ( ) | √ | √ | √ | ||||||||||
80 | Nagare et al. ( ) | √ | √ | √ | ||||||||||
81 | Tiwari et al. ( ) | √ | √ | √ | √ | |||||||||
82 | Ai et al. ( ) | √ | ||||||||||||
83 | Chakraborty et al. ( ) | √ | √ | √ | ||||||||||
84 | Shaikh et al. ( ) | √ | √ | √ | √ | |||||||||
85 | Maihami et al. ( ) | √ | √ | √ | √ | |||||||||
86 | Rabbani et al. ( ) | √ | √ | √ | ||||||||||
87 | Udayakumar and Geetha ( ) | √ | √ | √ | ||||||||||
88 | Soni et al. ( ) | √ | ||||||||||||
89 | Gor and Patel ( ) | √ | ||||||||||||
90 | Soni et al. ( ) | √ | √ | |||||||||||
91 | Aliabadi et al. ( ) | √ | √ | |||||||||||
92 | Cao et al. ( ) | √ | √ | |||||||||||
93 | Rastogi et al. ( ) | √ | ||||||||||||
94 | Ai et al. ( ) | √ | √ | |||||||||||
95 | Patel and Gor ( ) | √ | ||||||||||||
96 | Udayakumar and Geetha ( ) | √ | √ | √ | √ | |||||||||
97 | Ahmad and Benkherouf ( ) | √ | √ | |||||||||||
98 | Pal et al. ( ) | √ | √ | √ | ||||||||||
99 | Lashgari et al. ( ) | √ | √ | √ | ||||||||||
100 | Tashakkor et al. ( ) | √ | √ | √ | √ | |||||||||
101 | Palanivel et al. ( ) | √ | √ | √ | √ | √ | √ | √ | ||||||
102 | Pérez et al. ( ) | √ | √ | √ | √ | √ | ||||||||
103 | Li et al. ( ) | √ | √ | √ | √ | |||||||||
104 | Akhtar et al. ( ) | √ | √ | |||||||||||
105 | Almathkour and Benkherouf ( ) | √ | √ | √ | ||||||||||
106 | Das et al. ( ) | √ | √ | √ | √ | |||||||||
107 | Hasan et al. ( ) | √ | √ | √ | √ | |||||||||
108 | He et al. ( ) | √ | √ | |||||||||||
109 | Mahato and Mahata ( ) | √ | √ | √ | √ | √ | √ | |||||||
110 | Maihami et al. ( ) | √ | √ | √ | √ | √ | ||||||||
111 | Mishra et al. ( ) | √ | √ | √ | √ | |||||||||
112 | Nagare et al. ( ) | √ | √ | √ | √ | |||||||||
113 | Rapolu and Kandpal ( ) | √ | √ | √ | √ | |||||||||
114 | Rezagholifam et al. ( ) | √ | √ | √ | ||||||||||
115 | Soni and Suthar ( ) | √ | √ | √ | √ | |||||||||
116 | Sundararajan et al. ( ) | √ | √ | √ | ||||||||||
117 | Maheshwari et al. ( ) | |||||||||||||
118 | Tripathy et al. ( ) | √ | √ | √ | √ | |||||||||
119 | Udayakumar ( ) | √ | √ | |||||||||||
Appendix 2: Summary of SDG
SDG1 | Aims to end poverty globally with paid leave, providing financial lifesaving assistance, paying living wages, and the right to equality |
SDG 2 | Ending world hunger, achieving food security, improving nutrition, and promoting sustainable agriculture. Since most of the NIDIs-related literature targets perishable items such as meat, poultry, fish, eggs, dairy products, cooked leftovers, grains, fruits, and vegetables, we specifically explored this SDG |
SDG 3 | To ensure good health and well-being in the work environment, companies are working on minimizing the injury rate of their employees through means such as ensuring all factory employees complete mandatory safety training |
SDG 4 | To provide an inclusive, equitable, and high-quality education |
SDG 5 | Gender equality |
SDG 6 | Firm engagement in water stewardship, which ensures efficient water consumption and enables high water quality |
SDG 7 | Ensuring affordable and renewable energy through various initiatives, with some companies providing technologies for cheap, reliable, sustainable, and modern energy |
SDG 8 | Committing to human rights and labor rights in the workplace |
SDG 9 | Integrative and sustainable industrialization, supporting innovation, and strengthening infrastructure |
SDG 10 | The reduction of inequalities |
SDG 11 | The promotion of sustainable cities and communities |
SDG 12 | Ensures sustainable consumption and production patterns |
SDG 13 | Climate-related goals |
SDG 14 | Preservation and sustainable use of oceans, seas, and marine resources |
SDG 15 | Protect biodiversity and natural habitats |
SDG 16 | Addresses peace, justice, and strong institutions |
SDG 17 | Global partnership for sustainable development |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Maheshwari, P., Kamble, S., Belhadi, A. et al. UN sustainable development goals and management of non-instantaneous deteriorating items: a literature review and applications framework. Ann Oper Res (2024). https://doi.org/10.1007/s10479-024-06144-9
Download citation
Received : 03 March 2023
Accepted : 02 July 2024
Published : 01 August 2024
DOI : https://doi.org/10.1007/s10479-024-06144-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sustainable development goals
- Inventory management
- Non-instantaneous deteriorating items
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 31 July 2024
Clinical implications of the family history in patients with lung cancer: a systematic review of the literature and a new cross-sectional/prospective study design (FAHIC: lung)
- Fabrizio Citarella 1 , 2 ,
- Kazuki Takada 3 ,
- Priscilla Cascetta 4 ,
- Pierfilippo Crucitti 2 , 5 ,
- Roberta Petti 5 , 6 ,
- Bruno Vincenzi 1 , 2 ,
- Giuseppe Tonini 1 , 2 ,
- Francesco M. Venanzi 7 , 8 ,
- Alessandra Bulotta 7 , 8 ,
- Sara Oresti 7 , 8 ,
- Carlo Greco 2 , 9 ,
- Sara Ramella 2 , 9 ,
- Lucio Crinò 10 ,
- Angelo Delmonte 10 ,
- Roberto Ferrara 7 , 8 ,
- Massimo Di Maio 11 ,
- Fiorella Gurrieri 2 , 6 &
- Alessio Cortellini ORCID: orcid.org/0000-0002-1209-5735 1 , 2 , 12
Journal of Translational Medicine volume 22 , Article number: 714 ( 2024 ) Cite this article
1 Altmetric
Metrics details
Compared to other malignancies, few studies have investigated the role of family history of cancer (FHC) in patients with lung cancer, yielding largely heterogeneous results. We performed a systematic literature review in accordance with PRISMA guidelines, searching the PubMed and Scopus databases from their inception to November 25, 2023, to identify studies reporting on the role of FHC in patients with lung cancer. A total of 53 articles were included, most with a retrospective design and encompassing a variety of geographical areas and ethnicities.
Thirty studies (56.6%) assessed patients with non-small cell lung cancer (NSCLC), while 17 studies (32.1%) assessed patients with mixed histologies. Overall, the rates of FHC ranged from 8.3 to 68.9%, and the rates of family history of lung cancer ranged from 2 to 46.8%. Twenty-seven studies investigated FHC as a potential risk factor for lung cancer, with more than half reporting an increased risk for subjects with FHC. Five studies reported on the potential role of FHC in determining clinical outcomes, and twelve studies examined the relationship between FHC and germline mutations. Notably, only one study reported a significantly increased rate of germline mutations, including ATM , BRCA2 , and TP53 , for patients with a family history of lung cancer compared to those without, but both groups had a low prevalence of mutations (< 1%).
The FAHIC—Lung (NCT06196424) is the first cross-sectional/prospective study specifically developed to identify FHC patterns and within-family clusters of other risk factors, including smoking, to guide patients with NSCLC to systematic genetic counseling. Acknowledging the largely heterogeneous results of our systematic review and considering the clinical implications of detecting pathogenic germline variants (PGVs), the FAHIC-lung study aims to identify patients potentially enriched with PGVs/likely PGVs to direct them to germline screening outside of the research setting.
Introduction
Familial aggregation and inherited predisposition have been increasingly investigated in multiple cancer types. In breast, ovarian, prostate, and colorectal malignancies, international guidelines recommend genetic counselling in patients showing risk criteria for syndromes of inherited susceptibility to cancer, as aggregations with other malignancies have been widely described within families of these patient populations [ 1 , 2 , 3 ].
With a predicted number of death of about 160 000 cases in 2023 in Europe and 127 070 in US [ 4 , 5 ], Non-Small Cell Lung Cancer (NSCLC) still remains a leading cause of cancer death worldwide. A positive smoking history represents the main risk factor [ 6 ], while environmental factors such as exposure to radon, asbestosis and air pollution have been linked to lung cancer among never smokers [ 7 , 8 , 9 ].
Few studies have investigated the impact of a positive family history of cancer (FHC) in patients with NSCLC, describing the malignancies that can occur among relatives of patients with NSCLC, while only few and rare genetic syndromes associated with inherited germline genetic mutations, such as the Li-Fraumeni, have been directly linked to lung cancer risk [ 10 ]. Most of the studies did not provide information on the potential within-family clusters of other risk factors, including exposure to tobacco smoking, environmental carcinogens, and other geographical/epidemiological factors. Additionally, retrospective approaches to this topic are heavily impacted by recall bias and misclassification [ 11 , 12 ].
To underline the importance and potential clinical implications of investigating family history of cancer (FHC) in patients with non-small cell lung cancer (NSCLC), a recent retrospective study conducted in a cohort of 7.788 patients with NSCLC, who underwent commercially available germline genetic testing and reported an FHC of 71%, found that pathogenic germline variants (PGVs) or likely PGVs were present in 14.9% of the cases. Additionally, 2.9% of the cases carried a single PGV in a gene associated with autosomal recessive inheritance. Among positive patients, 61.3% carried a PGV/likely PGV in DNA damage and response (DDR) genes, and 95.1% of them harbored a PGV in genes with potential clinical implications, including BRCA2 (2.8%), CHEK2 (2.1%), ATM (1.9%), TP53 (1.3%), BRCA1 (1.2%), and EGFR (1.0%) [ 13 ].
In this manuscript, we present the results of a systematic review of the available evidence on the role of FHC in patients with lung cancer, and the design of the FAHIC-lung study (NCT06196424), a cross-sectional study that aims to prospectively describe the FHC and the potential within-family distribution of smoking and other risk factors, to identify patients more likely to be carriers of PGVs or likely PGVs.
Systematic review—methods
Literature search strategy and study selection criteria.
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We searched the PubMed and Scopus databases from their inception date to November 25, 2023, to identify potentially relevant articles. The search terms were “non-small cell lung cancer or NSCLC,” “family history,” “lung cancer,” and “risk.”
The inclusion criteria for the study selection were as follows: (1) patients diagnosed with NSCLC of any stage; (2) available information on the family history of cancer for the included population (e.g., prevalence and type of family history). The exclusion criteria were as follows: (1) lack of information on the family history of cancer; (2) studies not published in English; and (3) case reports.
As this study was a systematic review, ethical approval and informed consent were not required. The study protocol was registered in PROSPERO, an international prospective register of systematic reviews funded by the National Institute for Health Research (NIHR), with the registration code CRD4202450742 (available at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42024507422 ).
Data extraction and data synthesis
Two authors (F.C. and K.T.) performed the literature search and evaluated the eligibility of studies using the PICO (patients, interventions, comparison, and outcome) framework following the PRISMA criteria. Assuming a certain heterogeneity in the results, we adopted a textual narrative synthesis approach to summarize the included publications [ 14 ]. In view of that, we did not establish specific criteria for data synthesis (e.g., the minimum number of studies or level of consistency required for synthesis).
F.C. and T.K. independently reviewed and extracted data from the published papers, including first author, journal name, and year of publication. The prevalence (as a rate) of family history of cancer was summarized in a master table, along with the type of family history collected (e.g., lung-cancer specific vs. family history of any malignancy), study design, study population characteristics, smoking status of study participants and screened relatives (if available), primary tumor type (e.g., NSCLC, small cell lung cancer [SCLC], or others), number of patients included, and disease stage (e.g., early stage vs. advanced stage, if available). Study characteristics, context, and findings were summarized, and similarities/differences across studies were described in detail. Disagreements between the two authors (F.C. and K.T.) were discussed and resolved with a third independent author (A.C.).
Systematic review—results
We identified a total of 198 potentially relevant articles from the PubMed and Scopus online databases through an initial search strategy. After excluding 41 duplicate articles, we screened and reviewed the titles and abstracts of 157 articles, resulting in 54 being assessed for eligibility. Finally, a total of 53 articles were included in this systematic review. The flow diagram of the study selection process is shown in Fig. 1 while the whole search strategy with publications assessed at each step (identification, screening, eligibility and inclusion) is available as supplementary material (search strategy).

Flow diagram of the studies selection process according to the PRISMA guidelines
Overall, the vast majority of the studies had a retrospective design, with most of them being case–control or observational retrospective studies, with only one cross-sectional study [ 15 ] and one prospective study [ 16 ]. Study populations encompassed a variety of geographical areas/ethnicities, with 23 studies (43.4%) enrolling Asian patients, 13 studies (24.5%) enrolling patients with multiple ethnicities (all with a majority of white patients), 11 studies (20.7%) including non-specified ethnicities, and six studies (11.3%) including other populations. Even the included histology types showed heterogeneity, with 30 studies (56.6%) assessing patients with NSCLC, 17 studies (32.1%) assessing patients with a mixed type of lung cancer including small cell lung cancer (SCLC), four studies (7.5%) assessing other/unspecified types of lung cancer, one study (1.9%) assessing patients with adenocarcinoma, and one study (1.9%) assessing patients with EGFR -positive adenocarcinoma only.
FHC was collected through questionnaires in only three studies [ 17 , 18 , 19 ], while none of them used ad-hoc questionnaires specifically developed to collect FHC and the within-family distribution of other risk factors, including smoking. Twenty-five studies (47.2%) assessed family history (FH) by collecting all malignancies reported among relatives, 21 studies (39.6%) assessed FH of lung cancer, three studies (5.7%) assessed FHC and FH of lung cancer separately, three studies (5.7%) assessed FH of smoking-related and smoking-unrelated cancers, and two studies (3.8%) assessed FH of pre-specified types of cancer. The degree of relatedness ranged from first to second degree, although it was not reported for the majority of the included studies. One study reported on the smoking status among the relatives of study participants [ 20 ] and one study included the assessment of environmental factors (coal exposure) among the risk factors for lung cancer [ 21 ].
Overall, the rate of FHC in patients with lung cancer ranged from 8.3 [ 22 ] to 68.9% [ 20 ], while the rates of FH of lung cancer from 2 [ 23 ] to 46.8% [ 21 ]. Some studies enrolled cohorts of patients potentially enriched for FHC, such as 11 studies which assessed female patients only reporting FHC ranging from 7.7 [ 24 ] to 59.4% [ 25 ] and FH of lung cancer ranging from 6.2 [ 26 ] to 28% [ 27 ], four studies which specifically assessed never/light smoker patients only, reporting FHC ranging from 29.1 [ 28 ] to 68.9 [ 20 ], two studies assessing patients with small aggressive NSCLC, one study assessing male patients only, one study assessing smokers specifically, and one study assessing patients aged ≤ 45 years. A synoptic table with organization of results is available as supplementary file 1.
Studies investigating FHC as a risk factor for lung cancer
Overall, 27 studies investigated FHC as a potential risk factor for lung cancer (Table 1 ) [ 16 , 17 , 20 , 23 , 24 , 25 , 26 , 27 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. Six out of 11 studies (54.5%) that investigated the role of FHC as a whole or in pre-specified type of cancers reported an increased risk of developing lung cancer for patients with FHC, while 11 out of 16 studies (68.7%) that investigated the role of FH of lung cancer reported a significant association.
One study reported a more pronounced increased risk for women aged ≤ 45 years and a synergistic effect of smoking and FHC in increasing the risk of lung cancer [ 29 ], while another study reported that FH of lung cancer was specifically associated with an increased risk of early on set lung cancer (< 55 years old) [ 17 ]. One study that failed to demonstrate an association between FHC and lung cancer diagnosis, reported a significant effect for patients in whom at least one relative with cancer was diagnosed < 50 years of age [ 20 ], while one study that failed to demonstrate an association between FH of lung cancer and lung cancer risk, reported a significant effect for female patients only [ 42 ].
One study confirmed that FH of lung cancer was associated with risk of lung cancer in both the whole study population and among smokers [ 37 ], while another study reported that FH of lung cancer was more strongly associated with lung cancer risk in case of first/second degree of relatedness compared to collateral relatives [ 40 ].
Studies investigating the potential impact of FHC on clinical outcomes.
Five studies reported on the potential role of FHC in determining clinical outcomes (Table 2 ) [ 19 , 28 , 48 , 49 , 50 , 51 , 52 ]. One study reported no association between FH of lung cancer and outcomes [ 48 ], two studies reported a differential effect for FHC and FH of lung cancer [ 28 , 49 ] and one study reported a decreased risk of death for patients with FHC [ 50 ]. Similarly, one study reported improving outcomes from PD-1 immunotherapy with increasing burden of FHC [ 52 ].
Studies investigating associations between FHC and germline mutations.
Overall, 12 studies reported on the potential relationship between FHC and germline mutations (Table 3 ) [ 33 , 36 , 37 , 39 , 44 , 46 , 51 , 53 , 54 , 55 , 56 , 57 ]. Two studies did not show an enrichment of the germline mutations/polymorphisms of interest in patients with FHC [ 53 , 55 ], while three studies suggested a potential enrichment [ 46 , 54 , 57 ], with only one of them specifically reporting an increased rate of germline mutations including ATM, BRCA2 and TP53 for patients with family history of lung cancer compared to those with no FH [ 46 ]. Two studies reported a significant effect of the germline status in increasing the risk of lung cancer among patients with no FHC [ 33 , 36 ], while in three other studies the effect was independent of FHC [ 39 , 44 , 46 ]. One study showed a synergistic effect in increasing the risk of lung cancer of XRCC3/XRCC4 variants and FHC [ 37 ]. Two studies investigated the potential impact of germline polymorphisms on clinical outcomes, one showing an association between hOGG1 single nucleotide polymorphisms and worse survival specifically in patients without FHC [ 51 ], the other showing multifaceted effects of germline NOTCH4 polymorphisms depending on the FHC status [ 56 ].
Studies investigating associations between FHC and lung cancer somatic features.
Seven studies reported on the potential association between FHC and lung cancer somatic features (Table 4 ) [ 15 , 52 , 58 , 59 , 60 , 61 , 62 ]. Three studies did not confirm significant associations between FHC and somatic microsatellite instability status [ 58 ], somatic DDR genes status [ 52 ], or KRAS mutational status [ 59 ], while 2 studies reported a significant association between FHC and EGFR mutation [ 60 , 61 ]. In addition, another study reported an association between FHC and the occurrence of multiple somatic mutations in patients tested for multiple genes [ 62 ].
Studies investigating associations between FHC and other lung cancer features.
Nine studies included in this subgroup reported on associations between FHC and other lung cancer features (Table 5 ) [ 18 , 19 , 21 , 22 , 63 , 64 , 65 , 66 , 67 ]. One study reported a link between younger age at diagnosis female gender and FHC [ 63 ], one study reported an increased prevalence of FH of breast cancer among female patients with lung cancer [ 64 ], while another study reported a 10-years increasing trend over time for the prevalence of FHC [ 22 ]. Importantly, one study reported a significant association between FHC and smoking [ 19 ], while another study reported that FH of lung cancer was more frequent among young women, with synergistic effect with smoking and coil exposure in determining the younger age at diagnosis [ 21 ].
FAHIC lung—methods/design
Study design and objectives.
The FAHIC—Lung study (observational, prospective, multicenter study to investigate the family history of cancer in patients with non-small cell lung cancer) is a cross-sectional/prospective, observational, multicenter study. Consecutive patients with histologically diagnosed NSCLC will be enrolled, regardless of their age, TNM stage, smoking status, and other clinicopathologic characteristics. ClinicalTrials.gov identifier: NCT06196424.
The primary objective of the study is the identification of FHC patterns and within-family clusters of other risk factors to address patients with NSCLC for systematic genetic counseling for germline next-generation sequencing (NGS) testing to identify PGVs and likely PGVs. Secondary objectives include the description of clinicopathological and oncological characteristics of patients with NSCLC according to FHC patterns.
Patients’ family history will be carefully collected by investigators through a dedicated self-reported study questionnaire, which has been developed for the purpose of this study and validated by the genetic expert of the steering committee (F.G.) (Supplementary file 2). Study questionnaire will focus on: (1) family history of cancer; (2) type of tumors/primary tumor sites among relatives with history of cancer; (3) age at diagnosis among relatives with history of cancer; (4) biological sex of relatives with history of cancer; (5) exposure to tobacco smoking and smoking habits among relatives with history of cancer; (6) geographical origin of participants and relatives with history of cancer; (7) personal history of multiple malignancies; (8) potential professional and environmental exposure to carcinogens of participants and relatives with history of cancer; (9) ethnicity of both participants and relatives with history of cancer.
To minimize risks of recalling bias, patients will be followed up for four weeks through two study visits: the first study visit at enrolment and the follow-up study visit. During the first study visit all patient’s clinic-pathologic will be collected and study participants will be given the ad-hoc questionnaire, which will be returned to the study personnel at the follow-up study visit (Fig. 2 ).

FAHIC-lung study design diagram
The following clinic-pathologic characteristics will be collected: (1) smoking status (active/passive, package/year, total years of smoking); (2) Eastern Cooperative Oncology Group Performance Status (ECOG-PS); (3) age at diagnosis; (4) tumor histology; (5) tumor stage at diagnosis according to the 8th edition of TNM staging system; (6) ethnicity; (7) professional and environmental exposure to carcinogens; (8) programmed death ligand-1 tumor proportion score (PD—L1 TPS); (9) any available oncogenic drivers including EGFR, KRAS, BRAF, c-MET , mutations and ALK, ROS-1, RET, NTRK translocation/gene fusions; (10) personal history of other synchronous/metachronous primary malignancies.
The study plan includes an observational phase and an analytical phase:
Observational phase : after collecting participants’ questionnaires, we will first reconstruct patients’ family trees with additional information on how other potential risk factors, such as smoking history and exposure to professional/environmental carcinogens, segregate within the families with a history of cancer.
Analytical phase : once we have identified family clusters of malignancies and risk factors potentially associated with the highest risk of being carriers of germline PGVs or likely PGVs, we will proceed with the collection of blood samples for germline testing in a subgroup of patients. This will enable us to assess and compare the prevalence of PGVs/likely PGVs between patients more likely to be carriers and the control cohort. This approach aims to achieve a robust comparison, minimize systematic referrals to genetic counseling for all NSCLC patients, and optimize NGS testing requests outside the research setting. Considering the validity and comprehensiveness of high-throughput techniques in identifying PGVs/likely PGVs [ 68 ], we will assess the germline status of the groups of interest through whole exome sequencing (WES) after DNA extraction from blood samples in a two step analysis.
In the first step, the raw sequencing data (FASTQ files) will undergo bioinformatic processing. Mapping will be performed using a high-throughput aligner to ensure accurate alignment of the sequenced reads to the human genome. Variant calling will then be conducted to identify deviations from the reference genome. Filtering and annotation of these variants will focus on a pre-specified list of pre-specified genes known to be associated potentially associated with cancer (Supplementary file 3). This curated gene list will be used to prioritize PGVs/likely PGVs variants. Online tools will be utilized for variant prioritization, organizing the genes based on their correlation with lung cancer, thus enabling us to pinpoint the most relevant variants for further investigation.
In the second step, we aim to discover novel variants that may contribute to lung cancer predisposition. This phase involves a more exploratory analysis of the FASTQ data, looking beyond the known pathogenic variants. We will leverage the extensive genealogical data we have collected on the patients’ family histories to identify potential new genetic markers. The stored FASTQ files will be re-analyzed to detect previously unreported variants, incorporating bioinformatics tools and techniques for variant discovery. These include advanced algorithms for variant detection and annotation, as well as integrative approaches to assess the potential pathogenicity of novel variants. The integration of genealogical data will enhance our ability to correlate these novel variants with familial patterns of lung cancer, potentially uncovering new genetic predispositions. This comprehensive approach ensures that we maximize the utility of the sequencing data, providing a robust platform for both targeted and discovery-driven genetic analysis.
Participants selection
Inclusion Criteria include: (1) histopathological diagnosis of NSCLC (all stages); (2) age ≥ 18 years old; (3) signed written informed consent; (4) availability of familiar and/or personal anamnestic data of cancer. Exclusion Criteria include: (1) unavailability of familiar and/or personal anamnestic data of cancer; (2) patient’s refusal.
Statistical plan and sample size
The sample size of patients enrolled has been determined only for the observational phase of the study. This determination focuses on identifying patients who are more likely to be carriers of pathogenic germline variants (PGVs) or likely PGVs. This approach acknowledges the lack of information on the prevalence of germline PGVs/likely PGVs in patients with NSCLC who are not selected based on family history of cancer (FHC), as well as the limited knowledge regarding the potential characteristics that will define our group of interest. We hypothesized a prevalence of 10% of participants with an especially enriched family history of cancer to be directed to systematic germline testing; assuming a confidence level of 95% with a total width for the confidence interval of 0.1 (precision of ± 5%), the minimum number of subjects needed to properly describe the group of interest, following a binomial “exact” calculation of the sample size, is 175. To account for potential dropouts, we will enroll a minimum of 180 patients.
Descriptive statistics will be used as appropriate to report FHC data, the distribution of within-family other risk factors, and baseline clinicopathologic characteristics. Analyses will be performed using R-Studio software (R Core Team, 2021), and MedCalc® Statistical Software version 20 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org ; 2021).
To the best of our knowledge, this is the first systematic review summarizing the available evidence on the role of FHC in patients with lung cancer, and the FAHIC-lung study (NCT06196424) is the first cross-sectional/prospective study specifically designed to identify patients with NSCLC more likely to be carrier of PGVs/likely PGVs, that should be systematically referred to genetic counselling and germline testing.
Our review shows that few studies have focused on the family history of cancer (FHC) in patients with lung cancer, resulting in overall heterogeneous results, beginning with the extremely wide range of FHC and family history of lung cancer rates. The category with the highest number of reports included studies assessing FHC as a potential risk factor for developing lung cancer. However, even in this category, the results were largely discordant, with a variety of different approaches and categorizations. Most of the included studies followed a retrospective approach, which is inherently associated with recall bias in collecting family history information, and none used questionnaires specifically designed to collect FHC. To mitigate this bias, we developed our ad-hoc study questionnaire, while the cross-sectional/prospective approach with the 4-week interval will allow study participants to gather and report FHC information as carefully as possible.
Something that set lung cancer apart from other malignancies, where the FHC has an established role in defining the probability of being a carrier of PGVs/likely PGVs, such as ovarian, breast, prostate, and colorectal cancer, is the role of smoking. As mentioned, smoking history represents the main risk factor for lung cancer [ 6 ], several evidence shows that passive smoking from family members can be a detrimental factor and that even the smoking habit can be “inherited”, with a sort of intergenerational transmission [ 69 , 70 ]. The FAHIC-lung questionnaire will allow us to mitigate this potential bias as well, collecting smoking habit information and environmental exposure to carcinogens among patients’ relatives with cancer.
More than a half of the studies that assessed FHC and FH of lung cancer as a potential risk factor for lung cancer concluded that FHC plays a detrimental role, with a potential synergistic effect with smoking, that seems even more pronounced among young/female patients. Our systematic review also suggests that younger patients, female, Asian, and never/light smokers may be especially enriched in FHC, although with no clear/conclusive results, while no somatic genomic feature seems to be significantly associated with FHC, except for EGFR mutations.
Recently, increasing attention has been focused on the study of germline mutations as risk factor for lung cancer, highlighting how DDR genes alterations can be found among patients with lung adenocarcinoma, even in the context of wider within-family primary tumors spectrums, including breast/pancreatic cancers or hematological malignancies [ 10 ]. Even in the context of TP53-associated genetic susceptibility, FHC is gaining a clearer role, to the point of recommending genetic counselling for patients with lung adenocarcinoma younger than 46 years old and with an especially enriched FHC or personal history of multiple primary tumors [ 71 ].
Importantly, in our systematic review only one of the studies that investigated the multifaceted role of germline mutations reported a significant enrichment among patients with FHC [ 46 ]. Rifkin and colleagues first reported a systematic review on the evidence linking germline mutations with lung cancer risk, then validated through a large case–control study of patients undergoing germline whole exome sequencing (WES) the significant association between lung cancer risk and ATM , BRCA2 and TP 53 pathogenetic/likely pathogenetic germline mutations [ 46 ]. However, despite the overall enrichment among controls, variant-based and gene-based analyses showed a low prevalence of germline PGV/likely PGV in both cases and controls [ 46 ]. In addition, they reported a higher rate of carriers among study participants with FH of lung cancer compared to those without, but with a very low overall prevalence (0.8% vs 0.7% for the combination of ATM/BRCA2/TP53 ) [ 46 ], suggesting that a simplified collection of FHC information is not enough to identify patients with the highest probability of being carriers and to properly optimize germ-line NGC access.
Among gene-specific susceptibility for lung cancer, EGFR -associated one needs a special mention. Genetic counselling is already recommended for patients with somatic EGFR positive NSCLC younger than 50 years, regardless of their family history [ 10 ], however, a proper syndromic EGFR -associated lung cancer should be suspected in the case of the novo EGFR T790M mutations, especially with a somatic variant allele frequency (VAF) ≥ 35% [ 10 , 72 ], with even more rare EGFR variants, such as V834L and V843I being increasingly recognized [ 73 , 74 ]. Lastly, we will have to consider the complexity related to the multifaceted role of multiple primary tumors. Beyond the consisting evidence linking DDR genes mutations to a personal history of multiple malignancies, recent studies reported on the potential role of pleiotropic loci in determining the risk of multiple malignancies [ 75 ].
Our study plan has, however, some limitations. First, we will have to rely on patients' ability and willingness to reconstruct their family history, therefore the recall bias will exert a certain effect despite the cross/sectional prospective approach. In addition, we have no strictly predefined definition of potential family clusters to be analyzed. However, we can anticipate that the identified group of interest will likely include young female patients with adenocarcinoma histology, never or light smokers, patients with EGFR mutations, patients with a history of multiple primary tumors, and patients with a high burden of family history. This high burden of family history is particularly expected to be enriched in non-smoking associated cancers, including lung cancer, and in the DDR-genes associated cancer spectrum, such as breast, ovarian, prostate, melanoma, and pancreatic cancers.To ensure a comprehensive analysis, we also plan to incorporate other factors collected through our detailed questionnaire. These factors include smoking habits of the patients, passive smoking exposure, working exposure to carcinogens, and smoking habits of family members. By evaluating these additional factors, we aim to identify within-family clusters of other risk factors. Specifically, we will focus on selecting patients without a history of passive smoking, identifying patients with a younger age at diagnosis among their relatives with cancer, and considering patients with low working exposure to carcinogens. Despite having these anticipations, we have deliberately chosen to adopt an unbiased approach without pre-established features to define patients for germline tests. Considering the very low prevalence of germline mutations reported so far [ 46 ], this strategy allows for a more comprehensive and inclusive analysis, ensuring that we do not overlook any potential associations or risk factors to unravel the complexity of FHC information and identify patients especially enriched in PGVs/likely PGVs. Furthermore, considering that this is an observational study, we decided to adopt a two steps approach, in order to identify patients at risk as a first step. This, to minimize the potential clinical implications for study participants and let their treating physicians refer them to genetic counseling as per their existing clinical practice. Once the group of interest will be identified, we will amend the protocol to collect blood samples and allocate fundings for germline testing. Lastly, we have to consider that the FAIHC lung study is being conducted in Italy, therefore the study population will mostly consist of white/Caucasian patients. Although this will prevent us from gathering broader information on the potential implications of different races, we will be able to focus and obtain reliable results on patients with European ancestry.
In the context of a worldwide progressive implementation of chest computed tomography based screening programs in subject with smoking history [ 76 ], and considering the initial evidence of the potential benefit of screening programs among never smokers and other subjects potentially enriched in FHC/PGVs [ 77 ], identifying patients with the highest risk of being carrier of PGVs/likely PGVs would be extremely important to develop dedicated preventing measures in non-smoker subjects. Considering the costs of commercially available germline NGS tests and the potential preventive, prognostic, and therapeutic implications of the detection of germline mutations related to familial cancers, we believe that establishing FHC patterns to identify a subgroup of patients especially enriched in PGVs to direct to germline screening outside of the research setting, would be extremely helpful in optimizing resources, spare time and eventually improve patients’ outcomes.
Data Availability
This systematic review does not involve the generation of new data. The data analyzed in this study are derived from publicly available studies and publications that are cited within the paper. All sources of data, including databases and search strategies used to identify relevant studies, are described in the Methods section. Readers interested in accessing the underlying data can refer to the referenced studies and publications for more detailed information. Due to data management regulations, individual patient-level data from the FAIHC-lung study are not available. However, inquiries from third parties can be directed to the corresponding author.
Guidelines Detail: https://www.nccn.org/guidelines/guidelines-detail .
Stjepanovic N, Moreira L, Carneiro F, et al. Hereditary gastrointestinal cancers: ESMO clinical practice guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2019;30:1558–71.
Article CAS PubMed Google Scholar
Genetics of Prostate Cancer (PDQ ® )–Health Professional Version—NCI https://www.cancer.gov/types/prostate/hp/prostate-genetics-pdq .
Lung Cancer Statistics | How common is lung cancer? https://www.cancer.org/cancer/lung-cancer/about/key-statistics.html . Accessed 12 Mar 2023.
Malvezzi M, Santucci C, Boffetta P, et al. European cancer mortality predictions for the year 2023 with focus on lung cancer. Ann Oncol. 2023;34:410–9.
Steuer CE, Jegede OA, Dahlberg SE, et al. Smoking behavior in patients with early-stage NSCLC: a report from ECOG-ACRIN 1505 trial. J Thorac Oncol. 2021;16:960–7.
Article PubMed PubMed Central Google Scholar
Malhotra J, Malvezzi M, Negri E, et al. Risk factors for lung cancer worldwide. Eur Respir J. 2016;48:889–902.
Article PubMed Google Scholar
Riudavets M, Garcia de Herreros M, Besse B, et al. Radon and lung cancer: current trends and future perspectives. Cancers. 2022;14:3142.
Article CAS PubMed PubMed Central Google Scholar
A New Pathway from Air Pollution to Lung Cancer in Non-Smokers https://dailyreporter.esmo.org/esmo-congress-2022/research-advances-in-the-last-months/a-pathway-from-air-pollution-to-lung-cancer-in-non-smokers-has-been-identified .
Benusiglio PR, Fallet V, Sanchis-Borja M, et al. Lung cancer is also a hereditary disease. Eur Respir Rev. 2021;30: 210045.
Chang ET, Smedby KE, Hjalgrim H, et al. Reliability of self-reported family history of cancer in a large case-control study of lymphoma. J Natl Cancer Inst. 2006;98:61–8.
Murff HJ, Spigel DR, Syngal S. Does this patient have a family history of cancer? An evidence-based analysis of the accuracy of family cancer history. JAMA. 2004;292:1480–9.
Sorscher S, LoPiccolo J, Chen E, et al. Landscape of pathogenic germline variants in patients with lung cancer. JCO. 2022;40:388570–388570.
Article Google Scholar
Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol. 2009;9:59.
Lashkarizadeh M, Lashkarizadeh M, Nikian M, et al. The expression of HER2/neu in patients with lung cancer and its associated factors. Clin Respir J. 2023;17:90–5.
Tammemagi MC, Schmidt H, Martel S, et al. Participant selection for lung cancer screening by risk modelling (the Pan-Canadian early detection of lung cancer [PanCan] study): a single-arm, prospective study. Lancet Oncol. 2017;18:1523–31.
Cassidy A, Balsan J, Vesin A, et al. Cancer diagnosis in first-degree relatives and non-small cell lung cancer risk: results from a multi-centre case-control study in Europe. Eur J Cancer. 2009;45:3047–53.
Gaur P, Bhattacharya S, Kant S, et al. Hospital-based study on demographic, hematological, and biochemical profile of lung cancer patients. J Cancer Res Ther. 2020;16:839–42.
Isla D, Felip E, Viñolas N, et al. Lung cancer in women with a family history of cancer: the Spanish female-specific database WORLD07. Anticancer Res. 2016;36:6647–53.
Gorlova OY, Zhang Y, Schabath MB, et al. Never smokers and lung cancer risk: a case-control study of epidemiological factors. Int J Cancer. 2006;118:1798–804.
Chen Y, Li G, Lei Y, et al. Lung cancer family history and exposure to occupational/domestic coal combustion contribute to variations in clinicopathologic features and gene fusion patterns in non-small cell lung cancer. Thorac Cancer. 2019;10:695–707.
Zang R, Shi J-F, Lerut TE, et al. Ten-year trends of clinicopathologic features and surgical treatment of lung cancer in China. Ann Thorac Surg. 2020;109:389–95.
Tsugane S, Watanabe S, Sugimura H, et al. Smoking, occupation and family history in lung cancer patients under fifty years of age. Jpn J Clin Oncol. 1987;17:309–17.
CAS PubMed Google Scholar
Chen K-Y, Hsiao C-F, Chang G-C, et al. Hormone replacement therapy and lung cancer risk in Chinese. Cancer. 2007;110:1768–75.
Titan AL, He H, Lui N, et al. The influence of hormone replacement therapy on lung cancer incidence and mortality. J Thorac Cardiovasc Surg. 2020;159:1546-1556.e4.
Jin K, Hung RJ, Thomas S, et al. Hormonal factors in association with lung cancer among Asian women: a pooled analysis from the international lung cancer consortium. Int J Cancer. 2021;148:2241–54.
Pathak A, Wenzlaff AS, Hyland PL, et al. Apoptosis-related single nucleotide polymorphisms and the risk of non-small cell lung cancer in women. J Cancer Ther Res. 2014;3:1.
Article CAS Google Scholar
Lee Y, Jeon JH, Goh S-H, et al. The clinical impact of family history of cancer in female never-smoker lung adenocarcinoma. Lung Cancer. 2019;136:15–22.
Osann KE. Lung cancer in women: the importance of smoking, family history of cancer, and medical history of respiratory disease. Cancer Res. 1991;51:4893–7.
Schwartz AG, Wenzlaff AS, Prysak GM, et al. Reproductive factors, hormone use, estrogen receptor expression and risk of non small-cell lung cancer in women. J Clin Oncol. 2007;25:5785–92.
Tammemagi CM, Freedman MT, Church TR, et al. Factors associated with human small aggressive non small cell lung cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:2082–9.
Cote ML, Yoo W, Wenzlaff AS, et al. Tobacco and estrogen metabolic polymorphisms and risk of non-small cell lung cancer in women. Carcinogenesis. 2009;30:626–35.
Hong Y-S, Kang H-J, Kwak J-Y, et al. Association between microRNA196a2 rs11614913 genotypes and the risk of non-small cell lung cancer in Korean population. J Prev Med Public Health. 2011;44:125–30.
Schwartz AG, Wenzlaff AS, Bock CH, et al. Admixture mapping of lung cancer in 1812 African-Americans. Carcinogenesis. 2011;32:312–7.
Sin DD, Tammemagi CM, Lam S, et al. Pro-surfactant protein B as a biomarker for lung cancer prediction. J Clin Oncol. 2013;31:4536–43.
Xu P, Liu L, Wang J, et al. Genetic variation in BCL2 3’-UTR was associated with lung cancer risk and prognosis in male Chinese population. PLoS ONE. 2013;8: e72197.
He F, Chang S-C, Wallar GM, et al. Association of XRCC3 and XRCC4 gene polymorphisms, family history of cancer and tobacco smoking with non-small-cell lung cancer in a Chinese population: a case-control study. J Hum Genet. 2013;58:679–85.
Yilmaz M, Kacan T, Sari I, et al. Lack of association between the MTHFRC677T polymorphism and lung cancer in a Turkish population. Asian Pac J Cancer Prev. 2014;15:6333–7.
Tian G, Wang M, Xu X. The role of NQO1 polymorphisms in the susceptibility and chemotherapy response of Chinese NSCLC patients. Cell Biochem Biophys. 2014;69:475–9.
Li J, Zhang M, Yang F, et al. High risk occupational exposure and family history were risk factors in young lung cancer in Chinese. Int J Clin Exp Med. 2016;9(12):23650–7.
Google Scholar
White RW, Horvitz E. Evaluation of the feasibility of screening patients for early signs of lung carcinoma in web search logs. JAMA Oncol. 2017;3:398–401.
Warkentin MT, Tammemägi MC, Freedman MT, et al. Factors associated with small aggressive non-small cell lung cancers in the national lung screening trial: a validation study. JNCI Cancer Spectr. 2018;2:pkx010.
Brown D, Zingone A, Yu Y, et al. Relationship between circulating inflammation proteins and lung cancer diagnosis in the national lung screening trial. Cancer Epidemiol Biomarkers Prev. 2019;28:110–8.
Pineda Lancheros LE, Rojo Tolosa S, Gálvez Navas JM, et al. Effect of single nucleotide polymorphisms in the vitamin d metabolic pathway on susceptibility to non-small-cell lung cancer. Nutrients. 2022;14:4668.
Albano D, Dhamija A, Liao Y, et al. Lung cancer in nonsmokers—a risk factor analysis. Cancer Epidemiol. 2023;86: 102439.
Rifkin AS, Less EM, Wei J, et al. Association of reported candidate monogenic genes with lung cancer risk. Clin Lung Cancer. 2023;24:313–21.
Liu L, Yu H, Bai J, et al. Positive association of serum vitamin B6 levels with intrapulmonary lymph node and/or localized pleural metastases in non-small cell lung cancer: a retrospective study. Nutrients. 2023;15:2340.
Yang J, Li Y, Khoury T, et al. Relationships of hHpr1/p84/Thoc1 expression to clinicopathologic characteristics and prognosis in non-small cell lung cancer. Ann Clin Lab Sci. 2008;38:105–12.
CAS PubMed PubMed Central Google Scholar
Li N, Shao K, Chen Z, et al. The impact of positive cancer family history on the clinical features and outcome of patients with non-small cell lung cancer. Fam Cancer. 2011;10:331–6.
Li X, Pan X, Wang P, et al. Expression of ERCC1 mRNA in non-small cell lung cancer tissues and survival analysis of patients. Life Sci J. 2013;10(2):1926–31.
Su Y, Zhang H, Xu F, et al. DNA repair gene polymorphisms in relation to non-small cell lung cancer survival. Cell Physiol Biochem. 2015;36:1419–29.
Cortellini A, Giusti R, Filetti M, et al. High familial burden of cancer correlates with improved outcome from immunotherapy in patients with NSCLC independent of somatic DNA damage response gene status. J Hematol Oncol. 2022;15:9.
Tefre T, Børresen AL, Aamdal S, et al. Studies of the L-myc DNA polymorphism and relation to metastasis in Norwegian lung cancer patients. Br J Cancer. 1990;61:809–12.
Javid J, Mir R, Mirza M, et al. CC genotype of anti-apoptotic gene BCL-2 (-938 C/A) is an independent prognostic marker of unfavorable clinical outcome in patients with non-small-cell lung cancer. Clin Transl Oncol. 2015;17:289–95.
Liu Y, Kheradmand F, Davis CF, et al. Focused analysis of exome sequencing data for rare germline mutations in familial and sporadic lung cancer. J Thorac Oncol. 2016;11:52–61.
Xu Q, Lin D, Li X, et al. Association between single nucleotide polymorphisms of NOTCH signaling pathway-related genes and the prognosis of NSCLC. Cancer Manag Res. 2019;11:6895–905.
Liu M, Liu X, Suo P, et al. The contribution of hereditary cancer-related germline mutations to lung cancer susceptibility. Transl Lung Cancer Res. 2020;9:646–58.
Suzuki K, Ogura T, Yokose T, et al. Microsatellite instability in female non-small-cell lung cancer patients with familial clustering of malignancy. Br J Cancer. 1998;77:1003–8.
Yilmaz A, Mohamed N, Patterson KA, et al. Clinical and metabolic parameters in non-small cell lung carcinoma and colorectal cancer patients with and without KRAS mutations. Int J Environ Res Public Health. 2014;11:8645–60.
Cheng P-C, Cheng Y-C. Correlation between familial cancer history and epidermal growth factor receptor mutations in Taiwanese never smokers with non-small cell lung cancer: a case-control study. J Thorac Dis. 2015;7:281–7.
PubMed PubMed Central Google Scholar
Hsu K-H, Tseng J-S, Wang C-L, et al. Higher frequency but random distribution of EGFR mutation subtypes in familial lung cancer patients. Oncotarget. 2016;7:53299–308.
Chang F, Zhang H, Chen C, et al. Concomitant genetic alterations are associated with plasma D-dimer level in patients with non-small-cell lung cancer. Future Oncol. 2022;18:679–90.
Ambrosone CB, Rao U, Michalek AM, et al. Lung cancer histologic types and family history of cancer. Analysis of histologic subtypes of 872 patients with primary lung cancer. Cancer. 1993;72:1192–8.
Tsuchiya M, Iwasaki M, Otani T, et al. Breast cancer in first-degree relatives and risk of lung cancer: assessment of the existence of gene sex interactions. Jpn J Clin Oncol. 2007;37:419–23.
Banik A, Schwarzer R, Pawlowska I, et al. Women with family cancer history are at risk for poorer physical quality of life and lower self-efficacy: a longitudinal study among men and women with non-small cell lung cancer. Health Qual Life Outcomes. 2017;15:62.
Chen P-H, Chuang J-H, Lu T-P, et al. Non-intubated versus intubated video-assisted thoracic surgery in patients aged 75 years and older: a propensity matching study. Front Surg. 2022;9: 880007.
Li Q, Wei X, Wang Y, et al. Pulmonary mucoepidermoid carcinoma in the Chinese population: a clinical characteristic and prognostic analysis. Front Oncol. 2022;12: 916906.
Parsons DW, Roy A, Yang Y, et al. Diagnostic yield of clinical tumor and germline whole-exome sequencing for children with solid tumors. JAMA Oncol. 2016;2:616–24.
Dwivedi S, Pathak R, Agarwalla R, et al. The intergenerational transmission of tobacco habit: role of parents and the family. J Family Med Prim Care. 2016;5:373–7.
Saari AJ, Kentala J, Mattila KJ. The smoking habit of a close friend or family member–how deep is the impact? A cross-sectional study. BMJ Open. 2014;4: e003218.
Bougeard G, Renaux-Petel M, Flaman J-M, et al. Revisiting Li-Fraumeni Syndrome from TP53 mutation carriers. J Clin Oncol. 2015;33:2345–52.
Oxnard GR, Chen R, Pharr JC, et al. Germline EGFR mutations and familial lung cancer. J Clin Oncol. 2023;41:5274–84.
van der Leest C, Wagner A, Pedrosa RM, et al: Novel EGFR V834L Germline Mutation Associated With Familial Lung Adenocarcinoma. JCO Precis Oncol 2:PO.17.00266, 2018
Ohtsuka K, Ohnishi H, Fujiwara M, et al: Predisposition to Lung Adenocarcinoma in a Family Harboring the Germline EGFR V843I Mutation. JCO Precis Oncol 3:PO.19.00104, 2019
Lu M, Zhang X, Chu Q, et al. Susceptibility genes associated with multiple primary cancers. Cancers. 2023;15:5788.
Passiglia F, Cinquini M, Bertolaccini L, et al. Benefits and harms of lung cancer screening by chest computed tomography: a systematic review and meta-analysis. J Clin Oncol. 2021;39:2574–85.
Triphuridet N, Zhang SS, Nagasaka M, et al. Low-dose computed tomography (LDCT) lung cancer screening in asian female never-smokers is as efficacious in detecting lung cancer as in Asian male ever-smokers: a systematic review and meta-analysis. J Thorac Oncol. 2023;18:698–717.
Download references
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Operative Research Unit of Medical Oncology, Fondazione Policlinico Universitario Campus Bio-Medico, Via Alvaro del Portillo, 200, 00128, Rome, Italy
Fabrizio Citarella, Bruno Vincenzi, Giuseppe Tonini & Alessio Cortellini
Department of Medicine and Surgery, Universitá Campus Bio-Medico Di Roma, Via Alvaro del Portillo, 21, 00128, Rome, Italy
Fabrizio Citarella, Pierfilippo Crucitti, Bruno Vincenzi, Giuseppe Tonini, Carlo Greco, Sara Ramella, Fiorella Gurrieri & Alessio Cortellini
Department of Surgery, Saiseikai Fukuoka General Hospital, Fukuoka, Japan
Kazuki Takada
Department of Cancer Medicine, Gustave Roussy Cancer Campus, Villejuif, France
Priscilla Cascetta
Thoracic Surgery Department, Fondazione Policlinico Universitario Campus Bio-Medico, Via Alvaro del Portillo 200, 00128, Rome, Italy
Pierfilippo Crucitti & Roberta Petti
Operative Research Unit of Medical Genetics, Fondazione Policlinico Universitario Campus Bio-Medico, Via Alvaro del Portillo, 21, 00128, Rome, Italy
Roberta Petti & Fiorella Gurrieri
Università Vita-Salute San Raffaele, Milan, Italy
Francesco M. Venanzi, Alessandra Bulotta, Sara Oresti & Roberto Ferrara
Department of Medical Oncology, IRCCS Ospedale San Raffaele, Milan, Italy
Radiation Oncology, Fondazione Policlinico Universitario Campus Bio-Medico, Via Alvaro del Portillo, 200, 00128, Rome, Italy
Carlo Greco & Sara Ramella
Thoracic Oncology Unit, IRCCS Istituto Romagnolo Per Lo Studio Dei Tumori (IRST) “Dino Amadori”, Meldola, Italy
Lucio Crinò & Angelo Delmonte
Department of Oncology, Medical Oncology 1U, AOU Città della Salute e della Scienza di Torino, University of Turin, 10126, Turin, Italy
Massimo Di Maio
Department of Surgery and Cancer, Hammersmith Hospital Campus, Imperial College London, London, UK
Alessio Cortellini
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the publication according to the ICMJE guidelines for the authorship (study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript, critical revision). All authors read and approved the submitted version of the manuscript (and any substantially modified version that involves the author's contribution to the study). Each author has agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Correspondence to Alessio Cortellini .
Ethics declarations
Ethics approval and consent to participate.
All the study procedures will follow the precepts of Good Clinical Practice and the declaration of Helsinki. The study was approved by the local ethical committees on human experimentation (Comitato Etico Territoriale Lazio AREA 2, registro sperimentazioni 27.23 CET 2 CBM, 12 Oct 2023).
Competing interests
Alessio Cortellini declares speaker’s fees from MSD, AstraZeneca, Pierre-Fabre, EISAI, Sanofi/REGENERON, and Roche (outside of the present work) and advisory board roles/grant for consultancies from MSD, BMS, AstraZeneca, Roche, OncoC4, IQVIA, Pierre-Fabre, EISAI, REGENERON, Sanofi/REGENERON, Ardelis Health, AlphaSight, Access Infinity (outside of the present work). He also declares travel support from MSD and Roche. Sara Ramella declares advisory board roles and grant consultancies from Astra Zeneca, MSD (Merk) and Roche (outside of the present work). All other authors declare no conflicts of interest associated with the present study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary file 1., supplementary file 2., supplementary file 3., supplementary file 4., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Citarella, F., Takada, K., Cascetta, P. et al. Clinical implications of the family history in patients with lung cancer: a systematic review of the literature and a new cross-sectional/prospective study design (FAHIC: lung). J Transl Med 22 , 714 (2024). https://doi.org/10.1186/s12967-024-05538-4
Download citation
Received : 02 July 2024
Accepted : 24 July 2024
Published : 31 July 2024
DOI : https://doi.org/10.1186/s12967-024-05538-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lung cancer
- Family history of cancer
- Germline screening
Journal of Translational Medicine
ISSN: 1479-5876
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu
- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Managing neurodiversity in workplaces: a review and future research agenda for sustainable human resource management.

1. Introduction
2. literature review, 2.1. neurodiversity—origins of the concept and statistics, 2.2. neurodiversity in the labour market, 2.3. managing neurodiversity in workplaces—organizational barriers and needs, 3. materials and methods.
- What are the research directions and gaps in the topic of managing neurodiversity in workplaces mentioned in the literature?
- What are future research directions in the field of managing neurodiversity in workplaces with reference to Methodology, Theory, and Contexts?
5. Discussion and Conclusions
Author contributions, data availability statement, conflicts of interest.
| No. | References | Research Objective | Research Topic/Contexts | Methodology |
|---|---|---|---|---|
| 1 | [ ] | To emphasize the need for CEO adaptability and commitment in the ever-evolving landscape of workplace diversity | CEO leadership and its contribution to diversity management | - |
| 2 | [ ] | To present a multistage theoretical framework for managing neurodiversity | Addressing the gap between recognition and lack of theoretical frameworks and empirical research on workplace neurodiversity | - |
| 3 | [ ] | To understand the lived experiences of dealing with crisis in a remote working environment (based on 11 semi-structured interviews with 9 neurodivergent employees and 2 business professionals) | Lack of research on the impact of the COVID-19 crisis on neurominorities | Qualitative study |
| 4 | [ ] | To review existing research with respect to how autistic individuals fare for the four facets of emotional intelligence | Emotional intelligence in autistic individuals | Descriptive study |
| 5 | [ ] | To compare the experiences of neurodivergent adults undergoing workplace coaching before and during the pandemic | Disability coaching in a pandemic | Quantitative study—sample of 409 coachees from the UK |
| 6 | [ ] | To demystify the themes and assumptions affecting neurodivergent coachee experiences at work | Neurodiversity coaching | - |
| 7 | [ ] | To explore NDVs’ views about how the recruitment process and HR practices impact their employment relationship | Employment experience of the neurodiverse and the military veterans | Quantitative study (232 people with a medically diagnosed condition surveyed and 21 semi-structured interviews conducted) |
| 8 | [ ] | To seek to reframe the pathologized assumption of ADHD in career research and broader society to date. | Paradoxical career strengths and successes of ADHD adults | Qualitative positive-focused exploration |
| 9 | [ ] | To identify additional understudied invisible diversity dimensions | Invisible diversity dimensions in the hospitality industry | Prevailing methodologies in hospitality management |
| 10 | [ ] | To analyze power-laden tensions in traditional and novel brandings of neurodiversity | Neurodiversity branding | Critical discourse analysis |
| 11 | [ ] | To compare two families with disabled and neurodiverse children disproportionately affected by austerity cuts | Access to Special Educational Needs and Disability (SEND) support services in London, England | Qualitative study |
| 12 | [ ] | To examine successful management for autistic employees without applying a priori leadership constructs traditionally found in the literature | Effective management of autistic employees | - |
| 13 | [ ] | To promote effective and inclusive qualitative research that ensures that the specific needs of neurominorities are taken into account throughout the entire research pathway | How to conduct qualitative research with neurominorities | Qualitative research |
| 14 | [ ] | To explore an open, creative workplace developing neurodivergent talent | Neurodivergent individuals perceived as bringing new talent and innovation to the workplace | - |
| 15 | [ ] | To explore how interactions between clinicians, parents, and children lead to the reformulation of autism diagnosis from disorder to valuable social and cognitive differences | How clinician–patient interaction and patient age shape the process and meaning of autism diagnosis | A conversation analytic approach to data analysis/analysis of video recordings |
| 16 | [ ] | To examine the opportunities to create optimal conditions for individuals with autism in the workplace | How to redesign the work environment to enhance the well-being of individuals with autism | Qualitative research (21 in-depth interviews) |
| 17 | [ ] | To examine employee (manager and coworker) attitudes toward autism employment programs | Employee engagement and commitment to two Australian autism employment programs | Survey |
| 18 | [ ] | To examine the ability of corporate law firms to recognize the strengths and develop a type of employment both well suited to autistic strengths and able to make accommodations | Insight into the career paths of autistic professionals in large private practice law firms | - |
| 19 | [ ] | To explore the current inclusive human resource practices being adopted by neurodiversity champion companies | Enabling neurodiversity in the workplace via inclusive human resource practices | In-company interviews |
| 20 | [ ] | To generate a more nuanced understanding of the impact of accommodation on people with schizophrenia | Design considerations for residents with schizophrenia | Qualitative research approach |
| 21 | [ ] | To analyze the links between the neurodiversity of the workforce and digital transformation at the individual, organizational, and industry levels | Neurodiversity of the workforce and digital transformation: the case of inclusion of autistic workers at the workplace | Phenomenology (qualitative approach) |
| 22 | [ ] | To examine the disparate views on the neurodiverse workforce: 1/the benefits 2/the difficulty in finding and maintaining employment and to build a reconciling framework | How internal and external factors influence autistic employee outcomes and firm performance | - |
| 23 | [ ] | To examine neurodiversity as a cognitive strength from which leadership derives | Reconceptualizing leadership from a neurodiverse perspective | Critical disability theory |
| 24 | [ ] | To explore how autism influences the workplace | Autism in the workplace | Constant comparative method |
| 25 | [ ] | To describe how to design environmental conditions (acoustics, lighting, temperature, indoor air quality) that enhance performance by supporting basic physiological needs in the workplace (including designing spaces for neurodiversity) | Humanizing the office | - |
| 26 | [ ] | To explore the relationship between the above-average human capital of highly functioning neurodivergent employees, their subjective well-being in the workplace, and performance outcomes | The well-being of neurodivergent human capital in the workplace | AMO (ability, motivation, and opportunity) framework |
| 27 | [ ] | To identify the source of stereotype threat and the neurodivergent response to it | Stereotype threat anticipation in neurodivergent human capital | Analysis of brochures, learning sets, and posters |
| 28 | [ ] | To examine family relationships within families with neurodiverse kids further complicated by the COVID-19 pandemic | COVID-19 affecting alternative learners and their families | - |
| 29 | [ ] | To examine how and why parents with children with autism perform emotional work | Emotion work of parenting children with autism in Hong Kong | Qualitative data (analysis) |
| 30 | [ ] | To explore the school experience of high-functioning autistic teenagers regarding their academic and social inclusion | High-functioning autistic students speaking about their experience of inclusion in mainstream secondary schools (in France and Quebec) | A pragmatic, content analysis-driven approach |
| 31 | [ ] | To examine how DXC Technology (IT company) managed to develop disability-inclusive recruitment and selection systems along with work designs and environments that are disability friendly | DXC Technology is looking for neurodiverse talent (adults with high-functioning autism) | - |
| 32 | [ ] | To present a model of the unique challenges that workers with ASD face in the modern workplace | Overcoming barriers and integrating a neurodiverse workforce | A literature review on ASD juxtaposed to evidence-based social psychology and management theories |
| 33 | [ ] | To analyze how the introduction of autism into a home and the availability of intervention options change the structure and meaning of a home and reflect parental acceptance of a child’s autistic traits | Parental experiences of autism in Kerala, India, and Atlanta, GA USA | Observations |
| 34 | [ ] | This article examines challenges for human resource management posed by workplace adaptations for individuals with LD (learning disabilities) | Neurodiversity and human resource management | - |
- Honeybourne, V. The Neurodiverse Workplace: An Employer’s Guide to Managing and Working with Neurodivergent Employees, Clients and Customers ; Jessica Kingsley Publishers: London, UK, 2019. [ Google Scholar ]
- Hyland, S.; Connolly, J. Companies Leading in Disability Inclusion Have Outperformed Peers. Accenture Research Finds. Available online: https://newsroom.accenture.com/news/2018/companies-leading-in-disability-inclusion-have-outperformed-peers-accenture-research-finds (accessed on 4 July 2024).
- Jefferies, J.G.; Ahmed, W. Marketing Neurodiversity for Well-Being. J. Consum. Mark. 2022 , 39 , 632–648. [ Google Scholar ] [ CrossRef ]
- Whelpley, C.E.; Perrault, E. Autism at Work: How Internal and External Factors Influence Employee Outcomes and Firm Performance. J. Gen. Manag. 2021 , 46 , 210–219. [ Google Scholar ] [ CrossRef ]
- Vogus, T.J.; Taylor, J.L. Flipping the Script: Bringing an Organizational Perspective to the Study of Autism at Work. Autism 2018 , 22 , 514–516. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Campos-García, I.; Alonso-Muñoz, S.; González-Sánchez, R.; Medina-Salgado, M.-S. Human Resource Management and Sustainability: Bridging the 2030 Agenda. Corp. Soc. Responsib. Environ. Manag. 2024 , 31 , 2033–2053. [ Google Scholar ] [ CrossRef ]
- Ehnert, I.; Harry, W.; Zink, K.J. (Eds.) Sustainability and Human Resource Management. Developing Sustainable Business Organizations ; Springer: Berlin/Heidelberg, Germany, 2014. [ Google Scholar ] [ CrossRef ]
- Sarkis, J.; Sundaram, A. An Examination of Sustainable Human Resource Management Practices in Developing Countries. J. Clean. Prod. 2016 , 114 , 664–673. [ Google Scholar ]
- Flamini, G.; Gnan, L. Sustainable HRM. In Organizing Sustainable Development ; Routledge: London, UK, 2023; pp. 172–186. [ Google Scholar ] [ CrossRef ]
- Singer, J. Odd People in: The Birth of Community Amongst People on the Autism Spectrum: A Personal Exploration of a New Social Movement Based on Neurological Diversity ; University of Technology: Sydney, Australia, 1998. [ Google Scholar ]
- Armstrong, T. The Power of Neurodiversity: Unleashing the Advantages of Your Differently Wired Brain ; Da Capo Press: Philadelphia, PA, USA, 2011. [ Google Scholar ]
- Rothstein, A. Review: Mental Disorder or Neurodiversity? New Atlantis 2012 , 36 , 99–115. [ Google Scholar ]
- Singer, J. Why Can’t You Be Normal for Once in Your Life? From a Problem with No Name to the Emergence of a New Category of Difference. In Disability Discourse ; Corker, M., French, S., Eds.; Open University Press: Buckingham, UK, 1999; pp. 59–67. [ Google Scholar ]
- Hendrickx, S. The Adolescent and Adult Neuro-Diversity Handbook: Asperger’s Syndrome, ADHD, Dyslexia, Dyspraxia, and Related Conditions ; Jessica Kingsley Publishers: London, UK, 2010. [ Google Scholar ]
- McGee, M. Neurodiversity. Contexts 2012 , 11 , 12–13. [ Google Scholar ] [ CrossRef ]
- Maenner, M.J.; Shaw, K.A.; Baio, J.; Washington, A.; Patrick, M.; DiRienzo, K.; Christensen, D.L.; Wiggins, D.L.; Pettygrove, S.; Andrews, J.G.; et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016. CDC MMWR Surveill. Summ. 2020 , 69 , 1–16. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Polskiautyzm.pl. Available online: https://polskiautyzm.pl/ (accessed on 28 June 2024).
- Supreme Audit Office. Available online: https://www.nik.gov.pl/plik/id,23545.pdf (accessed on 28 June 2024).
- Wiater, M. Innowacje Społeczne w Obszarze Neuroróżnorodności. Eduk. Ekon. i Menedżerów 2022 , 64 , 37–49. Available online: https://econjournals.sgh.waw.pl/EEiM/article/view/2989 (accessed on 28 June 2024). [ CrossRef ]
- Whelpley, C.E.; Banks, G.C.; Bochantin, J.E.; Sandoval, R. Tensions on the Spectrum: An Inductive Investigation of Employee and Manager Experiences of Autism. J. Bus. Psychol. 2020 , 36 , 283–297. [ Google Scholar ] [ CrossRef ]
- Morath, E. America’s Hidden Workforce Returns; Disabled Workers Join Job Market at Highest Level in Years Amid Low Unemployment and Stricter Rules for Claiming Benefits. Wall Street Journal. Available online: https://www.wsj.com/articles/americas-hidden-workforce-returns-11548478801 (accessed on 28 June 2024).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders , 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [ Google Scholar ]
- Smith, M.D.; Belcher, R.G.; Juhrs, P.D. A Guide to Successful Employment for Individuals with Autism ; Brookes Publishing Company: Baltimore, MD, USA, 1997. [ Google Scholar ]
- Austin, R.D.; Pisano, G.P. Neurodiversity as a Competitive Advantage. Harv. Bus. Rev. 2017 , 95 , 96–103. [ Google Scholar ]
- Howlin, P.; Goode, S.; Hutton, J.; Rutter, M. Adult Outcome for Children with Autism. J. Child Psychol. Psychiatry 2004 , 45 , 212–229. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Krumm, N.; Turner, T.N.; Baker, C.; Vives, L.; Mohajeri, K.; Witherspoon, K.; Raja, A.; Coe, B.P.; Stessman, H.A.; He, Z.X.; et al. Excess of Rare, Inherited Truncating Mutations in Autism. Nat. Genet. 2015 , 47 , 582–588. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gerhardt, P.F.; Lainer, I. Addressing the Needs of Adolescents and Adults with Autism: A Crisis on the Horizon. J. Contemp. Psychother. 2011 , 41 , 37–45. [ Google Scholar ] [ CrossRef ]
- Polish Economic Institute; JiM Foundation. Raport Praca Autyzm Jim Pik ; Polish Economic Institute: Warsaw, Poland, 2022; p. 4. Available online: https://jim.org/en/raport_praca_autyzm_jim_pik/ (accessed on 28 June 2024).
- Wiater, M. Wyzwania Związane z Zatrudnianiem Osób Neuroróżnorodnych w Polsce. HRM Zarz. Zasob. Ludzk. 2023 , 154 , 80–92. [ Google Scholar ]
- Fundacja Synapsis. Available online: https://synapsis.org.pl/ (accessed on 28 June 2024).
- Johnson, T.D.; Joshi, A. Dark Clouds or Silver Linings? A Stigma Threat Perspective on the Implications of an Autism Diagnosis for Workplace Well-Being. J. Appl. Psychol. 2016 , 101 , 430–449. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lorenz, T.; Frischling, C.; Cuadros, R.; Heinitz, K. Autism and Overcoming Job Barriers: Comparing Job-Related Barriers and Possible Solutions In and Outside of Autism-Specific Employment. PLoS ONE 2016 , 11 , e0147040. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Neely, B.H.; Hunter, S.T. In a Discussion of Invisible Disabilities, Let Us not Lose Sight of Employees on the Autism Spectrum. Ind. Organ. Psychol. 2014 , 7 , 274–277. [ Google Scholar ] [ CrossRef ]
- Hill, E.L. Linking Clinical and Industrial Psychology: Autism Spectrum Disorder at Work. Ind. Organ. Psychol. 2014 , 7 , 152–155. [ Google Scholar ] [ CrossRef ]
- Richards, J.; Sang, K.; Marks, A.; Gill, S. “I’ve Found It Extremely Draining” Emotional Labour and the Lived Experience of Line Managing Neurodiversity. Pers. Rev. 2019 , 48 , 1903–1923. [ Google Scholar ] [ CrossRef ]
- Ryan, R.M.; Deci, E.L. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. Am. Psychol. 2000 , 55 , 68–78. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Berwick, K.R. Stress Among Student Affairs Administrators: The Relationship of Personal Characteristics and Organizational Variables to Work-Related Stress. J. Coll. Stud. Dev. 1992 , 33 , 11–19. [ Google Scholar ]
- Conley, V.M. Separation: An Internal Aspect of the Staffing Process. Coll. Stud. Aff. J. 2001 , 21 , 57–63. [ Google Scholar ]
- Tull, A. Synergistic Supervision, Job Satisfaction, and Intention to Turnover of New Professionals in Student Affairs. J. Coll. Stud. Dev. 2006 , 4 , 465–480. [ Google Scholar ] [ CrossRef ]
- Snyder, H. Literature Review as a Research Methodology: An Overview and Guidelines. J. Bus. Res. 2019 , 104 , 333–339. [ Google Scholar ] [ CrossRef ]
- Paul, J.; Criado, A.R. The Art of Writing Literature Review: What Do We Know and What Do We Need to Know? Int. Bus. Rev. 2020 , 29 , 1–7. [ Google Scholar ] [ CrossRef ]
- Rollnik-Sadowska, E. Labor Market in Sustainability Transitions: A Systematic Literature Review. Econ. Environ. 2023 , 87 , 4. [ Google Scholar ] [ CrossRef ]
- Ejdys, J.; Szpilko, D. European Green Deal–Research Directions. Syst. Lit. Review. Econ. Environ. 2022 , 81 , 8–38. [ Google Scholar ] [ CrossRef ]
- Barkun, Y.; Rollnik-Sadowska, E.; Glińska, E. The Concept of ‘Talent’ in the Labor Management Perspective-The Bibliometric Analysis of Literature. Int. J. Ind. Eng. Manag. 2020 , 12 , 104–115. [ Google Scholar ] [ CrossRef ]
- Kaššaj, M.; Peráček, T. Synergies and potential of Industry 4.0 and automated vehicles in smart city infrastructure. Appl. Sci. 2024 , 14 , 3575. [ Google Scholar ] [ CrossRef ]
- Krzeminska, A.; Austin, R.; Bruyére, S.; Hedley, D. The Advantages and Challenges of Neurodiversity Employment in Organizations. J. Manag. Organ. 2019 , 25 , 453–463. [ Google Scholar ] [ CrossRef ]
- Morrison, K.E.; DeBrabander, K.M.; Jones, D.R.; Ackerman, R.A.; Sasson, N.J. Social Cognition, Social Skill, and Social Motivation Minimally Predict Social Interaction Outcomes for Autistic and Non-Autistic Adults. Front. Psychol. 2020 , 11 , 1–22. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Stenn, T.; Lalor, A.R.; Coplan, J.; Osterholt, D.A. Managing neurodiversity inclusion in today’s entrepreneurial-styled workplace. In Managing for Social Justice. Harnessing Management Theory and Practice for Collective Good ; Poonamalle, L., Howard, A.D., Joy, S., Eds.; Springer International Publishing: Cham, Switzerland, 2023. [ Google Scholar ]
- Doyle, N.; McDowall, A. Diamond in the Rough? An ‘Empty Review’ of Research into ‘Neurodiversity’ and a Road Map for Developing the Inclusion Agenda. Equal. Divers. Incl. 2022 , 41 , 352–382. [ Google Scholar ] [ CrossRef ]
- Muhammad, R.; Omkar, D.; Duan, X. Leadership Strategies for Effective Diversity Management ; IGI Global: Hershey, PA, USA, 2023. [ Google Scholar ] [ CrossRef ]
- Khan, M.H.; Grabarski, M.K.; Ali, M.; Buckmaster, S. Insights into Creating and Managing an Inclusive Neurodiverse Workplace for Positive Outcomes: A Multistaged Theoretical Framework. Group Organ. Manag. 2023 , 48 , 1339–1386. [ Google Scholar ] [ CrossRef ]
- Szulc, J.M.; McGregor, F.-L.; Cakir, E. Neurodiversity and Remote Work in Times of Crisis: Lessons for HR. Pers. Rev. 2023 , 52 , 1677–1692. [ Google Scholar ] [ CrossRef ]
- Howes, S.S. Emotional Intelligence in Autistic Adults: A Review with Considerations for Employers. Sustainability 2023 , 15 , 7252. [ Google Scholar ] [ CrossRef ]
- Doyle, N.; Bradley, E. Disability Coaching in a Pandemic. J. Work. -Appl. Manag. 2023 , 15 , 135–147. [ Google Scholar ] [ CrossRef ]
- Doyle, N.; McDowall, A. Neurodiversity Coaching: A Psychological Approach to Supporting Neurodivergent Talent and Career Potential , 1st ed.; Routledge: London, UK, 2023. [ Google Scholar ] [ CrossRef ]
- Allen, R.A.; Dickmann, M.; Priscott, T.; White, G.R.T. Exploring Positive and Negative Intersectionality Effects: An Employment Study of Neurodiverse UK Military Veterans. Int. J. Hum. Resour. Manag. 2023 . [ Google Scholar ] [ CrossRef ]
- Crook, T.; McDowall, A. Paradoxical Career Strengths and Successes of ADHD Adults: An Evolving Narrative. J. Work. Manag. 2023 , 16 , 112–126. [ Google Scholar ] [ CrossRef ]
- Waterbury, C.J.; Smith, N. Invisible Diversity in the Hospitality Industry. In The Routledge Handbook of Diversity, Equity, and Inclusion Management in the Hospitality Industry ; Routledge: London, UK, 2023; pp. 128–139. [ Google Scholar ]
- Branton, S.E.; Villamil, A.M.; Reed, J.L. Branding Neurodiversity: A Critical Discourse Analysis of Communicative Capitalism and Change Empowerment Among Neurodiversity Workforce Intermediaries. J. Public Relat. Res. 2023 , 35 , 357–374. [ Google Scholar ] [ CrossRef ]
- Warnock, R. Relational Legacies and Relative Experiences: Austerity, Inequality, and Access to Special Educational Needs and Disability (SEND) Support in London, England. Geogr. J. 2023 , 1–12. [ Google Scholar ] [ CrossRef ]
- Whelpley, C.E.; Woznyj, H.M. Balancing the Teeter Totter: A Dialectical View of Managing Neurodiverse Employees. Hum. Perform. 2023 , 36 , 133–154. [ Google Scholar ] [ CrossRef ]
- Szulc, J.M. Towards More Inclusive Qualitative Research: The Practice of Interviewing Neurominorities. Labour Ind. 2023 , 33 , 179–187. [ Google Scholar ] [ CrossRef ]
- Turowetz, J.; Wiscons, L.Z.; Maynard, D.W. Disorder or Difference? How Clinician-Patient Interaction and Patient Age Shape the Process and Meaning of Autism Diagnosis. Sociol. Heal. Illn. 2023 , 46 , 171–188. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tomczak, M.T. How Can the Work Environment Be Redesigned to Enhance the Well-Being of Individuals with Autism? Empl. Relat. 2022 , 44 , 1467–1484. [ Google Scholar ] [ CrossRef ]
- Spoor, J.R.; Flower, R.L.; Bury, S.M.; Hedley, D. Employee Engagement and Commitment to Two Australian Autism Employment Programs: Associations with Workload and Perceived Supervisor Support. Equal. Divers. Incl. 2022 , 41 , 508–524. [ Google Scholar ] [ CrossRef ]
- Hinder, A.M. Stellar Evolution: Career Paths of Autistic Professionals in Corporate Law Firms. In Emerald Studies in Workplace Neurodiversity ; Generation, A., Hurley-Hanson, A.E., Giannantonio, C.M., Eds.; Emerald Publishing Limited: Leeds, UK, 2022; pp. 65–82. [ Google Scholar ] [ CrossRef ]
- Molloy, A.; O‘Donoghue, A.; Fu, N. Enabling Neurodiversity in the Workplace via Inclusive Human Resource Practices. In Emerald Studies in Workplace Neurodiversity ; Generation, A., Hurley-Hanson, A.E., Giannantonio, C.M., Eds.; Emerald Publishing Limited: Leeds, UK, 2022; pp. 85–109. [ Google Scholar ] [ CrossRef ]
- Karol, E.; Smith, D. Design Considerations for Residents with Impeded Cognitive Functioning: Conversations with People with Schizophrenia. Sustainability 2021 , 13 , 7733. [ Google Scholar ] [ CrossRef ]
- Walkowiak, E. Neurodiversity of the Workforce and Digital Transformation: The Case of Inclusion of Autistic Workers at the Workplace. Technol. Forecast. Soc. Chang. 2021 , 168 , 120739. [ Google Scholar ] [ CrossRef ]
- Roberson, Q.; Quigley, N.R.; Vickers, K.; Bruck, I. Reconceptualizing Leadership from a Neurodiverse Perspective. Group Organ. Manag. 2021 , 46 , 399–423. [ Google Scholar ] [ CrossRef ]
- Oseland, N. Beyond the Workplace Zoo: Humanising the Office , 1st ed.; Routledge: London, UK, 2021. [ Google Scholar ] [ CrossRef ]
- Szulc, J.M.; Davies, J.; Tomczak, M.T.; McGregor, F.-L. AMO Perspectives on the Well-Being of Neurodivergent Human Capital. Empl. Relat. 2021 , 43 , 858–872. [ Google Scholar ] [ CrossRef ]
- Priscott, T.; Allen, R.A. Human Capital Neurodiversity: An Examination of Stereotype Threat Anticipation. Empl. Relat. 2021 , 43 , 1067–1082. [ Google Scholar ] [ CrossRef ]
- Saline, S. Thriving in the New Normal: How COVID-19 Has Affected Alternative Learners and Their Families and Implementing Effective, Creative Therapeutic Interventions. Smith Coll. Stud. Soc. Work. 2021 , 91 , 1–28. [ Google Scholar ] [ CrossRef ]
- Kwok, K.; Kwok, D.K. More than Comfort and Discomfort: Emotion Work of Parenting Children with Autism in Hong Kong. Child. Youth Serv. Rev. 2020 , 118 , 105456. [ Google Scholar ] [ CrossRef ]
- Aubineau, M.; Blicharska, T. High-Functioning Autistic Students Speak about Their Experience of Inclusion in Mainstream Secondary Schools. Sch. Ment. Health 2020 , 12 , 537–555. [ Google Scholar ] [ CrossRef ]
- Carrero, J.; Krzeminska, A.; Härtel, C.E.J. The DXC Technology Work Experience Program: Disability-Inclusive Recruitment and Selection in Action. J. Manag. Organ. 2019 , 25 , 535–542. [ Google Scholar ] [ CrossRef ]
- Patton, E. Autism, Attributions and Accommodations: Overcoming Barriers and Integrating a Neurodiverse Workforce. Pers. Rev. 2019 , 48 , 915–934. [ Google Scholar ] [ CrossRef ]
- Sarrett, J.C. Custodial Homes, Therapeutic Homes, and Parental Acceptance: Parental Experiences of Autism in Kerala, India, and Atlanta, GA USA. Cult. Med. Psychiatry 2015 , 39 , 254–276. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sumner, K.E.; Brown, T.J. Neurodiversity and Human Resource Management: Employer Challenges for Applicants and Employees with Learning Disabilities. Psychol.-Manag. J. 2015 , 18 , 77–85. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Cluster Number | Cluster Name | Key Words |
|---|---|---|
| 1 | Gender-Specific Mental Health and Quality of Life in Autism Spectrum Disorder | Article, autism spectrum disorder, female, human, male, mental health, quality of life, well-being |
| 2 | Inclusive Human Engineering and Neurodiversity in Disability Studies | Disability, human engineering, inclusion, neurodiversity |
| 3 | Psychological Perspectives on Autism and Employment in the Workplace | Autism, employment, psychology, workplace |
| 4 | Advanced Strategies in Human Resource Management: Recruitment and Selection | Human resource management, recruitment, selection |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Rollnik-Sadowska, E.; Grabińska, V. Managing Neurodiversity in Workplaces: A Review and Future Research Agenda for Sustainable Human Resource Management. Sustainability 2024 , 16 , 6594. https://doi.org/10.3390/su16156594
Rollnik-Sadowska E, Grabińska V. Managing Neurodiversity in Workplaces: A Review and Future Research Agenda for Sustainable Human Resource Management. Sustainability . 2024; 16(15):6594. https://doi.org/10.3390/su16156594
Rollnik-Sadowska, Ewa, and Violetta Grabińska. 2024. "Managing Neurodiversity in Workplaces: A Review and Future Research Agenda for Sustainable Human Resource Management" Sustainability 16, no. 15: 6594. https://doi.org/10.3390/su16156594
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Open access
- Published: 25 July 2024
Strategies to strengthen the resilience of primary health care in the COVID-19 pandemic: a scoping review
- Ali Mohammad Mosadeghrad 1 ,
- Mahnaz Afshari 2 ,
- Parvaneh Isfahani 3 ,
- Farahnaz Ezzati 4 ,
- Mahdi Abbasi 4 ,
- Shahrzad Akhavan Farahani 4 ,
- Maryam Zahmatkesh 5 &
- Leila Eslambolchi 4
BMC Health Services Research volume 24 , Article number: 841 ( 2024 ) Cite this article
326 Accesses
Metrics details
Primary Health Care (PHC) systems are pivotal in delivering essential health services during crises, as demonstrated during the COVID-19 pandemic. With varied global strategies to reinforce PHC systems, this scoping review consolidates these efforts, identifying and categorizing key resilience-building strategies.
Adopting Arksey and O'Malley's scoping review framework, this study synthesized literature across five databases and Google Scholar, encompassing studies up to December 31st, 2022. We focused on English and Persian studies that addressed interventions to strengthen PHC amidst COVID-19. Data were analyzed through thematic framework analysis employing MAXQDA 10 software.
Our review encapsulated 167 studies from 48 countries, revealing 194 interventions to strengthen PHC resilience, categorized into governance and leadership, financing, workforce, infrastructures, information systems, and service delivery. Notable strategies included telemedicine, workforce training, psychological support, and enhanced health information systems. The diversity of the interventions reflects a robust global response, emphasizing the adaptability of strategies across different health systems.
Conclusions
The study underscored the need for well-resourced, managed, and adaptable PHC systems, capable of maintaining continuity in health services during emergencies. The identified interventions suggested a roadmap for integrating resilience into PHC, essential for global health security. This collective knowledge offered a strategic framework to enhance PHC systems' readiness for future health challenges, contributing to the overall sustainability and effectiveness of global health systems.
Peer Review reports
The health system is a complex network that encompasses individuals, groups, and organizations engaged in policymaking, financing, resource generation, and service provision. These efforts collectively aim to safeguard and enhance people health, meet their expectations, and provide financial protection [ 1 ]. The World Health Organization's (WHO) framework outlines six foundational building blocks for a robust health system: governance and leadership, financing, workforce, infrastructure along with technologies and medicine, information systems, and service delivery. Strengthening these elements is essential for health systems to realize their objectives of advancing and preserving public health [ 2 ].
Effective governance in health systems encompasses the organization of structures, processes, and authority, ensuring resource stewardship and aligning stakeholders’ behaviors with health goals [ 3 ]. Financial mechanisms are designed to provide health services without imposing financial hardship, achieved through strategic fund collection, management and allocation [ 4 , 5 ]. An equitable, competent, and well-distributed health workforce is crucial in delivering healthcare services and fulfilling health system objectives [ 2 ]. Access to vital medical supplies, technologies, and medicines is a cornerstone of effective health services, while health information systems play a pivotal role in generating, processing, and utilizing health data, informing policy decisions [ 2 , 5 ]. Collectively, these components interact to offer quality health services that are safe, effective, timely, affordable, and patient-centered [ 2 ]
The WHO, at the 1978 Alma-Ata conference, introduced primary health care (PHC) as the fundamental strategy to attain global health equity [ 6 ]. Subsequent declarations, such as the one in Astana in 2018, have reaffirmed the pivotal role of PHC in delivering high-quality health care for all [ 7 ]. PHC represents the first level of contact within the health system, offering comprehensive, accessible, community-based care that is culturally sensitive and supported by appropriate technology [ 8 ]. Essential care through PHC encompasses health education, proper nutrition, access to clean water and sanitation, maternal and child healthcare, immunizations, treatment of common diseases, and the provision of essential drugs [ 6 ]. PHC aims to provide protective, preventive, curative, and rehabilitative services that are as close to the community as possible [ 9 ].
Global health systems, however, have faced significant disruptions from various shocks and crises [ 10 ], with the COVID-19 pandemic being a recent and profound example. The pandemic has stressed health systems worldwide, infecting over 775 million and claiming more than 7.04 million lives as of April 13th, 2024 [ 11 ]. Despite the pandemic highlighting the critical role of hospitals and intensive care, it also revealed the limitations of specialized medicine when not complemented by a robust PHC system [ 12 ].
The pandemic brought to light the vulnerabilities of PHC systems, noting a significant decrease in the use of primary care for non-emergency conditions. Routine health services, including immunizations, prenatal care, and chronic disease management, were severely impacted [ 13 ]. The challenges—quarantine restrictions, fears of infection, staffing and resource shortages, suspended non-emergency services, and financial barriers—reduced essential service utilization [ 14 ]. This led to an avoidance of healthcare, further exacerbating health inequalities and emphasizing the need for more resilient PHC systems [ 15 , 16 , 17 ].
Resilient PHC systems are designed to predict, prevent, prepare, absorb, adapt, and transform when facing crises, ensuring the continuity of routine health services [ 18 ]. Investing in the development of such systems can not only enhance crisis response but also foster post-crisis transformation and improvement. This study focuses on identifying global interventions and strategies to cultivate resilient PHC systems, aiding policymakers and managers in making informed decisions in times of crisis.
In 2023, we conducted a scoping review to collect and synthesize evidence from a broad spectrum of studies addressing the COVID-19 pandemic. A scoping review allows for the assessment of literature's volume, nature, and comprehensiveness, and is uniquely inclusive of both peer-reviewed articles and gray literature—such as reports, white papers, and policy documents. Unlike systematic reviews, it typically does not require a quality assessment of the included literature, making it well-suited for rapidly gathering a wide scope of evidence [ 19 ]. Our goal was to uncover the breadth of solutions aimed at bolstering the resilience of the PHC system throughout the COVID-19 crisis. The outcomes of this review are intended to inform the development of a model that ensures the PHC system's ability to continue delivering not just emergency services but also essential care during times of crisis.
We employed Arksey and O'Malley's methodological framework, which consists of six steps: formulating the research question, identifying relevant studies, selecting the pertinent studies, extracting data, synthesizing and reporting the findings, and, where applicable, consulting with stakeholders to inform and validate the results [ 20 ]. This comprehensive approach is designed to capture a wide range of interventions and strategies, with the ultimate aim of crafting a robust PHC system that can withstand the pressures of a global health emergency
Stage 1: identifying the research question
Our scoping review was guided by the central question: "Which strategies and interventions have been implemented to enhance the resilience of primary healthcare systems in response to the COVID-19 pandemic?" This question aimed to capture a comprehensive array of responses to understand the full scope of resilience-building activities within PHC systems.
Stage 2: identifying relevant studies
To ensure a thorough review, we conducted systematic searches across multiple databases, specifically targeting literature up to December 31st, 2022. The databases included PubMed, Web of Science, Scopus, Magiran, and SID. We also leveraged the expansive reach of Google Scholar. Our search strategy incorporated a bilingual approach, utilizing both English and Persian keywords that encompassed "PHC," "resilience," "strategies," and "policies," along with the logical operators AND/OR to refine the search. Additionally, we employed Medical Subject Headings (MeSH) terms to enhance the precision of our search. The results were meticulously organized and managed using the Endnote X8 citation manager, facilitating the systematic selection and review of pertinent literature.
Stage 3: selecting studies
In the third stage, we meticulously vetted our search results to exclude duplicate entries by comparing bibliographic details such as titles, authors, publication dates, and journal names. This task was performed independently by two of our authors, LE and MA, who rigorously screened titles and abstracts. Discrepancies encountered during this process were brought to the attention of a third author, AMM, for resolution through consensus.
Subsequently, full-text articles were evaluated by four team members—LE, MA, PI, and SHZ—to ascertain their relevance to our research question. The selection hinged on identifying articles that discussed strategies aimed at bolstering the resilience of PHC systems amidst the COVID-19 pandemic Table 1 .
We have articulated the specific inclusion and exclusion criteria that guided our selection process in Table 2 , ensuring transparency and replicability of our review methodology
Stage 4: charting the data
Data extraction was conducted by a team of six researchers (LE, MA, PI, MA, FE, and SHZ), utilizing a structured data extraction form. For each selected study, we collated details including the article title, the first author’s name, the year of publication, the country where the study was conducted, the employed research methodology, the sample size, the type of document, and the PHC strengthening strategies described.
In pursuit of maintaining rigorous credibility in our study, we adopted a dual-review process. Each article was independently reviewed by pairs of researchers to mitigate bias and ensure a thorough analysis. Discrepancies between reviewers were addressed through discussion to reach consensus. In instances where consensus could not be reached, the matter was escalated to a third, neutral reviewer. Additionally, to guarantee thoroughness, either LE or MA conducted a final review of the complete data extraction for each study.
Stage 5: collating, summarizing and reporting the results
In this stage, authors LE, MZ, and MA worked independently to synthesize the data derived from the selected studies. Differences in interpretation were collaboratively discussed until a consensus was reached, with AMM providing arbitration where required.
We employed a framework thematic analysis, underpinned by the WHO's health system building blocks model, to structure our findings. This model categorizes health system components into six foundational elements: governance and leadership; health financing; health workforce; medical products, vaccines, and technologies; health information systems; and service delivery [ 2 ]. Using MAXQDA 10 software, we coded the identified PHC strengthening strategies within these six thematic areas.
Summary of search results and study selection
In total, 4315 articles were found by initial search. After removing 397 duplicates, 3918 titles and abstracts were screened and 3606 irrelevant ones were deleted. Finally, 167 articles of 312 reviewed full texts were included in data synthesis (Fig. 1 ). Main characteristics of included studies are presented in Appendix 1.

PRISMA Flowchart of search process and results
Characteristics of studies
These studies were published in 2020 (18.6%), 2021 (36.5%) and 2022 (44.9%). They were conducted in 48 countries, mostly in the US (39 studies), the UK (16 studies), Canada (11 studies), Iran (10 studies) and Brazil (7 studies) as shown in Fig. 2 .

Distribution of reviewed studies by country
Although the majority of the reviewed publications were original articles (55.1 %) and review papers (21 %), other types of documents such as reports, policy briefs, analysis, etc., were also included in this review (Fig. 3 ).
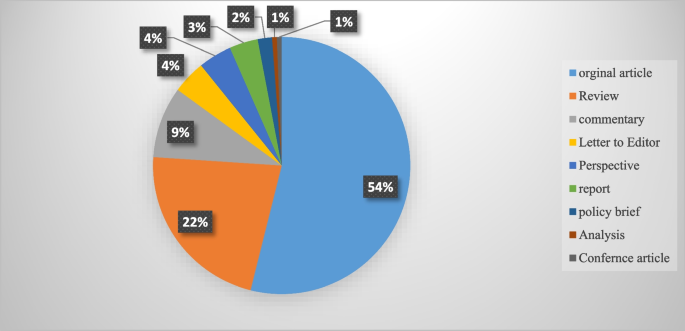
An overview of the publication types
Strengthening interventions to build a resilient PHC system
In total, 194 interventions were identified for strengthening the resilience of PHC systems to respond to the COVID-19 pandemic. They were grouped into six themes of PHC governance and leadership (46 interventions), PHC financing (21 interventions), PHC workforce (37 interventions), PHC infrastructures, equipment, medicines and vaccines (30 interventions), PHC information system (21 interventions) and PHC service delivery (39 interventions). These strategies are shown in Table 3 .
This scoping review aimed to identify and categorize the range of interventions employed globally to strengthen the resilience of primary healthcare (PHC) systems in the face of the COVID-19 pandemic. Our comprehensive search yielded 194 distinct interventions across 48 countries, affirming the significant international efforts to sustain healthcare services during this unprecedented crisis. These interventions have been classified according to the WHO’s six building block model of health systems, providing a framework for analyzing their breadth and depth. This review complements and expands upon the findings from Pradhan et al., who identified 28 interventions specifically within low and middle-income countries, signaling the universality of the challenge and the myriad of innovative responses it has provoked globally [ 178 ].
The review highlights the critical role of governance and leadership in PHC resilience. Effective organizational structure changes, legal reforms, and policy development were crucial in creating adaptive healthcare systems capable of meeting the dynamic challenges posed by the pandemic. These findings resonate with the two strategies of effective leadership and coordination emphasized by Pradhan et al. (2023), and underscore the need for clear vision, evidence-based policy, and active community engagement in governance [ 178 ]. The COVID-19 pandemic posed significant challenges for PHC systems globally. A pivotal response to these challenges was the active involvement of key stakeholders in the decision-making process. This inclusivity spanned across the spectrum of general practitioners, health professionals, health managers, and patients. By engaging these vital contributors, it became possible to address their specific needs and to design and implement people-centered services effectively [ 41 , 42 , 43 ].
The development and implementation of collaborative, evidence-informed policies and national healthcare plans were imperative. Such strategies required robust leadership, bolstered by political commitment, to ensure that the necessary changes could be enacted swiftly and efficiently [ 41 , 45 ]. Leaders within the health system were called upon to foster an environment of good governance. This entailed promoting increased participation from all sectors of the healthcare community, enhancing transparency in decision-making processes, and upholding the principles of legitimacy, accountability, and responsibility within the health system [ 10 ]. The collective aim was to create a more resilient, responsive, and equitable healthcare system in the face of the pandemic's demands.
In the wake of the COVID-19 pandemic, governments were compelled to implement new laws and regulations. These were designed to address a range of issues from professional accreditation and ethical concerns to supporting the families of healthcare workers. Additionally, these legal frameworks facilitated the integration of emerging services such as telemedicine into the healthcare system, ensuring that these services were regulated and standardized [ 38 , 40 , 61 ]. A key aspect of managing the pandemic was the establishment of effective and transparent communication systems for patients, public health authorities, and the healthcare system at large [ 60 , 61 ]. To disseminate vital information regarding the pandemic, vaccination programs, and healthcare services, authorities leveraged various channels. Public media, local online platforms, and neighborhood networks were instrumental in keeping the public informed about the ongoing situation and available services [ 53 , 60 , 86 ]. For health professionals, digital communication tools such as emails and WhatsApp groups, as well as regular meetings, were utilized to distribute clinical guidelines, government directives, and to address any queries they might have had. This ensured that healthcare workers were kept up-to-date with the evolving landscape of the pandemic and could adapt their practices accordingly [ 60 , 144 ].
Healthcare facilities function as complex socio-technical entities, combining multiple specialties and adapting to the ever-changing landscape of healthcare needs and environments [ 179 ]. To navigate this dynamic, policy makers must take into account an array of determinants—political, economic, social, and environmental—that influence health outcomes. Effective management of a health crisis necessitates robust collaboration across various sectors, including government bodies, public health organizations, primary healthcare systems, and hospitals. Such collaboration is not only pivotal during crisis management but also during the development of preparedness plans [ 63 ]. Within the health system, horizontal collaboration among departments and vertical collaboration between the Ministry of Health and other governmental departments are vital. These cooperative efforts are key to reinforce the resilience of the primary healthcare system. Moreover, a strong alliance between national pandemic response teams and primary healthcare authorities is essential to identifying and resolving issues within the PHC system [ 29 ]. On an international scale, collaborations and communications are integral to the procurement of essential medical supplies, such as medicines, equipment, and vaccines. These international partnerships are fundamental to ensuring that health systems remain equipped to face health emergencies [ 63 ].
To ensure the PHC system's preparedness and response capacity was at its best, regular and effective monitoring and evaluation programs were put in place. These included rigorous quarterly stress tests at the district level, which scrutinized the infrastructure and technology to pinpoint the system’s strengths and areas for improvement [ 43 ]. Furthermore, clinical audits were conducted to assess the structure, processes, and outcomes of healthcare programs, thereby enhancing the quality and effectiveness of the services provided [ 63 ]. These evaluation measures were crucial for maintaining a high standard of care and for adapting to the ever-evolving challenges faced by the PHC system.
Financial strategies played a critical role in enabling access to essential health services without imposing undue financial hardship. Various revenue-raising, pooling, and purchasing strategies were implemented to expand PHC financing during the pandemic, illustrating the multifaceted approach needed to sustain healthcare operations under strained circumstances [ 9 , 19 ].
In response to the COVID-19 pandemic, the Indian government took decisive action to bolster the country's healthcare infrastructure. By enhancing the financial capacity of states, the government was able to inject more funds into the Primary Health Care (PHC) system. This influx of resources made it possible to introduce schemes providing free medications and diagnostic services [ 50 ]. The benefits of increased financial resources were also felt beyond India's borders, enabling the compensation of health services in various forms. In Greece, it facilitated the monitoring and treatment of COVID-19 through in-person, home-based, and remote health services provided by physicians in private practice. Similarly, in Iran, the financial boost supported the acquisition of basic and para-clinical services from the private sector [ 21 , 65 ]. These measures reflect a broader international effort to adapt and sustain health services during a global health crisis.
The COVID-19 pandemic presented a formidable challenge to the PHC workforce worldwide. Healthcare workers were subjected to overwhelming workloads and faced significant threats to both their physical and mental well-being. To build resilience in the face of this crisis, a suite of interventions was implemented. These included recruitment strategies, training and development programs, enhanced teamwork, improved protective measures, comprehensive performance appraisals, and appropriate compensation mechanisms, as documented in Table 3 . To address staffing needs within PHC centers, a range of professionals including general practitioners, nurses, community health workers, and technical staff were either newly employed or redeployed from other healthcare facilities [ 63 ]. Expert practitioners were positioned on the frontlines, providing both in-person services and telephone consultations, acting as gatekeepers in the health system [ 49 , 63 ]. Support staff with technological expertise played a crucial role as well, assisting patients in navigating patient portals, utilizing new digital services, and conducting video visits [ 102 ]. Furthermore, the acute shortage of healthcare workers was mitigated by recruiting individuals who were retired, not currently practicing, or in training as students, as well as by enlisting volunteers. This strategy was key to bolstering the workforce and ensuring continuity of care during the pandemic [ 109 ].
During the pandemic, new training programs were developed to prepare healthcare staff for the evolving demands of their roles. These comprehensive courses covered a wide array of critical topics, including the correct use of personal protective equipment (PPE), the operation of ventilators, patient safety protocols, infection prevention, teamwork, problem-solving, self-care techniques, mental health support, strategies for managing stress, navigating and applying reliable web-based information, emergency response tactics, telemedicine, and direct care for COVID-19 patients [ 74 , 95 , 100 , 108 , 110 , 112 , 117 ].
Acknowledging the psychological and professional pressures faced by the primary healthcare workforce, health managers took active measures to safeguard both the physical and mental well-being of their employees during this challenging period [ 124 ]. Efforts to protect physical health included monitoring health status, ensuring vaccination against COVID-19, and providing adequate PPE [ 63 , 72 ]. To address mental health, a variety of interventions were deployed to mitigate anxiety and related issues among frontline workers. In Egypt, for instance, healthcare workers benefited from psychotherapy services and adaptable work schedules to alleviate stress [ 126 ]. Singapore employed complementary strategies, such as yoga, meditation, and the encouragement of religious practices, to promote relaxation among staff [ 133 ]. In the United States, the Wellness Hub application was utilized as a tool for employees to enhance their mental health [ 132 ]. In addition to health and wellness initiatives, there were financial incentives aimed at motivating employees. Payment protocols were revised, and new incentives, including scholarship opportunities and career development programs, were introduced to foster job satisfaction and motivation among healthcare workers [ 63 ].
The resilience of PHC systems during the pandemic hinged on several key improvements. Enhancing health facilities, supplying medicines and diagnostic kits, distributing vaccines, providing medical equipment, and building robust digital infrastructure were all fundamental elements that contributed to the strength of PHC systems, as outlined in Table 3 . Safe and accessible primary healthcare was facilitated through various means. Wheelchair routes were created for patients to ensure their mobility within healthcare facilities. , dedicated COVID-19 clinics were established, mass vaccination centers were opened to expedite immunization, and mobile screening stations were launched to extend testing capabilities [ 23 , 33 , 63 , 140 ].
In Iran, the distribution and availability of basic medicines were managed in collaboration with the Food and Drug Organization, ensuring that essential medications reached those in need [ 89 ]. During the outbreak, personal protective equipment (PPE) was among the most critical supplies. Access to PPE was prioritized, particularly for vulnerable groups and healthcare workers, to provide a layer of safety against the virus [ 63 ]. Vaccines were made available at no cost, with governments taking active measures to monitor their safety and side effects, to enhance their quality, and to secure international approvals. Furthermore, effective communication strategies were employed to keep the public informed about vaccine-related developments [ 32 , 83 ].
These comprehensive efforts underscored the commitment to maintaining a resilient PHC system in the face of a global health every individual in the community could access healthcare services. To facilitate this, free high-speed Wi-Fi hotspots were established, enabling patients to engage in video consultations and utilize a range of e-services without the barrier of internet costs crisis. Significant enhancements were made to the digital infrastructure. This expansion was critical in ensuring that [ 30 , 54 ]. Complementing these measures, a variety of digital health tools were deployed to further modernize care delivery. Countries like Nigeria and Germany, for instance, saw the introduction of portable electrocardiograms and telemedical stethoscopes. These innovations allowed for more comprehensive remote assessments and diagnostics, helping to bridge the gap between traditional in-person consultations and the emerging needs for telemedicine [ 141 , 180 ].
Throughout the COVID-19 pandemic, targeted interventions were implemented to bolster information systems and research efforts, as outlined in Table 3 . Key among these was the advancement of a modern, secure public health information system to ensure access to health data was not only reliable and timely but also transparent and accurate [ 33 , 45 , 49 ]. The "Open Notes" initiative in the United States exemplified this effort, guaranteeing patient access to, and editorial control over, their health records [ 141 ]. Management strategies also promoted the "one-health" approach, facilitating the exchange of health data across various departments and sectors to enhance public health outcomes [ 10 ].
In addition to these information system upgrades, active patient surveillance and early warning systems were instituted in collaboration with public health agencies. These systems played a pivotal role in detecting outbreaks, providing precise reports on the incidents, characterizing the epidemiology of pathogens, tracking their spread, and evaluating the efficacy of control strategies. They were instrumental in pinpointing areas of concern, informing smart lockdowns, and improving contact tracing methods [ 33 , 63 , 72 ]. The reinforcement of these surveillance and warning systems had a profound impact on shaping and implementing a responsive strategy to the health crisis [ 10 ].
To further reinforce the response to the pandemic, enhancing primary healthcare (PHC) research capacity became crucial. This enabled healthcare professionals and policymakers to discern both facilitators and barriers within the system and to devise fitting strategies to address emerging challenges. To this end, formal advisory groups and multidisciplinary expert panels, which included specialists from epidemiology, clinical services, social care, sociology, policy-making, and management, were convened. These groups harnessed the best available evidence to inform decision-making processes [ 30 ]. Consequently, research units were established to carry out regular telephone surveys and to collect data on effective practices, as well as new diagnostic and therapeutic approaches [ 31 , 89 ]. The valuable insights gained from these research endeavors were then disseminated through trusted channels to both the public and policymakers, ensuring informed decisions at all levels [ 36 ].
The COVID-19 pandemic acted as a catalyst for the swift integration of telemedicine into healthcare systems globally. This period saw healthcare providers leverage telecommunication technologies to offer an array of remote services, addressing medical needs such as consultations, diagnosis, monitoring, and prescriptions. This transition was instrumental in ensuring care continuity and mitigating infection risks for both patients and healthcare workers, highlighting an innovative evolution in healthcare delivery [ 170 , 181 ].
Countries adapted to this new model of healthcare with varied applications: Armenia established telephone follow-ups and video consultations for remote patient care, while e-pharmacies and mobile health tools provided immediate access to medical information and services [ 29 ]. In France and the United States, tele-mental health services and online group support became a means to support healthy living during the pandemic [ 147 , 158 ] . New Zealand introduced the Aroha chatbot, an initiative to assist with mental health management [ 139 ].
The implementation and effectiveness of these telehealth services were not limited by economic barriers, as underscored by Pradhan et al. (2023), who noted the key role of telemedicine in low and middle-income countries. These countries embraced the technology to maintain health service operations, proving its global applicability and utility [ 178 ]. The widespread adoption of telemedicine, therefore, represents a significant and perhaps lasting shift in healthcare practice, one that has redefined patient care in the face of a global health crisis and may continue to shape the future of healthcare delivery [ 170 , 178 , 181 ].
The study highlighted PHC strengthening strategies in COVID-19 time . Notably, the adaptations and reforms spanned across governance, financing, workforce management, information system, infrastructural readiness, and service delivery enhancements. These interventions collectively contributed to the robustness of health systems against the sudden surge in demand and the multifaceted challenges imposed by the pandemic and resulted.
Significantly, the findings have broader implications for health policy and system design worldwide. The pandemic has highlighted the critical need for resilient health systems that are capable of not only responding to health emergencies but also maintaining continuity in essential services. The strategies documented in this review serve as a template for countries to fortify their health systems by embedding resilience into their PHC frameworks (Fig. 4 ). Future health crises can be better managed by learning from these evidenced responses, which emphasize the necessity of integrated, well-supported, and dynamically adaptable health care structures.
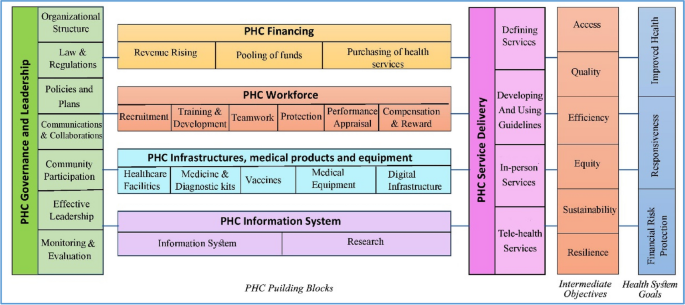
A model for strengthening the resilience of the primary health care system
Looking ahead, realist reviews could play a pivotal role in refining PHC resilience strategies. By understanding the context in which specific interventions succeed or fail, realist reviews can help policymakers and practitioners design more effective health system reforms, as echoed in the need for evidence-based planning in health system governance [ 9 ] . These reviews offer a methodological advantage by focusing on the causality between interventions and outcomes, aligning with the importance of effective health system leadership and management [ 50 , 182 ] . They take into account the underlying mechanisms and contextual factors, thus providing a nuanced understanding that is crucial for tailoring interventions to meet local needs effectively [ 28 , 86 ] , ultimately leading to more sustainable health systems globally. This shift towards a more analytical and context-sensitive approach in evaluating health interventions, as supported by WHO's framework for action [ 2 , 10 ] , will be crucial for developing strategies that are not only effective in theory but also practical and sustainable in diverse real-world settings.
Limitations and future research
In our comprehensive scoping review, we analyzed 167 articles out of a dataset of 4,315, classifying 194 interventions that build resilience in primary healthcare systems across the globe in response to pandemics like COVID-19. While the review's extensive search provides a sweeping overview of various strategies, it may not capture the full diversity of interventions across all regions and economies. Future research should focus on meta-analyses to evaluate the effectiveness of these interventions in greater detail and employ qualitative studies to delve into the specific challenges and successes, thus gaining a more nuanced understanding of the context. As the review includes articles only up to December 31, 2022, it may overlook more recent studies. Regular updates, a broader linguistic range, and the inclusion of a more diverse array of databases are recommended to maintain relevance and expand the breadth of literature, ultimately guiding more focused research that could significantly enhance the resilience of PHC systems worldwide.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
Primary Health Care
World Health Organization
Sustainable Development Goals
Universal Health Coverage
Personal Protective Equipment
General Practitioner
Mosadeghrad AM. A practical model for health policy making and analysis. Payesh. 2022;21(1):7–24 ([in Persian]).
Article Google Scholar
World Health Organization. Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes. WHO’s Framework for Action. Geneva: World Health Organization; 2007.
Google Scholar
Khosravi MF, Mosadeghrad AM, Arab M. Health System Governance Evaluation: A Scoping Review. Iran J Public Health. 2023;52(2):265.
PubMed PubMed Central Google Scholar
Mosadeghrad AM, Abbasi M, Abbasi M, Heidari M. Sustainable health financing methods in developing countries: a scoping review. J of School Public Health Inst Public Health Res. 2023;20(4):358–78 ([in Persian]).
Mosadeghrad AM. Health strengthening plan, a supplement to Iran health transformation plan: letter to the editor. Tehran Univ Med J. 2019;77(8):537–8 ([in Persian]).
World Health Organization. Declaration of alma-ata. Copenhagen: Regional Office for Europe; 1978. p. 1–4.
Rasanathan K, Evans TG. Primary health care, the Declaration of Astana and COVID-19. Bull World Health Organ. 2020;98(11):801.
Article PubMed PubMed Central Google Scholar
World Health Organization, UNICEF. Operational framework for primary health care: transforming vision into action. Geneva: World Health Organization and the United Nations Children’s Fund; 2020.
Mosadeghrad AM, Heydari M, Esfahani P. Primary health care strengthening strategies in Iran: a realistic review. J School Public Health Inst Public Health Res. 2022;19(3):237–58 ([in Persian]).
Sagan A, Webb E, Azzopardi-Muscat N, de la Mata I, McKee M, Figueras J. Health systems resilience during COVID-19: Lessons for building back better. Regional Office for Europe: World Health Organization; 2021.
World Health Organization, Coronavirus (COVID-19) map. Available at https://covid19.who.int/ /. Access date 14/04/2024.
Plagg B, Piccoliori G, Oschmann J, Engl A, Eisendle K. Primary health care and hospital management during COVID-19: lessons from lombardy. Risk Manag Healthc Policy. 2021:3987–92.
World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. World Health Organization; 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1 .
Mosadeghrad AM, Jajarmizadeh A. Continuity of essential health services during the COVID-19 pandemic. Tehran Univ Med J. 2021;79(10):831–2 ([in Persian]).
Splinter MJ, Velek P, Ikram MK, Kieboom BC, Peeters RP, Bindels PJ, Ikram MA, Wolters FJ, Leening MJ, de Schepper EI, Licher S. Prevalence and determinants of healthcare avoidance during the COVID-19 pandemic: A population-based cross-sectional study. PLoS Med. 2021;18(11):e1003854.
Article CAS PubMed PubMed Central Google Scholar
Wangmo S, Sarkar S, Islam T, Rahman MH, Landry M. Maintaining essential health services during the pandemic in Bangladesh: the role of primary health care supported by routine health information system. WHO South East Asia J Public Health. 2021;10(3):93.
Kumpunen S, Webb E, Permanand G, Zheleznyakov E, Edwards N, van Ginneken E, Jakab M. Transformations in the landscape of primary health care during COVID-19: Themes from the European region. Health Policy. 2022;126(5):391–7.
Article PubMed Google Scholar
Ezzati F, Mosadeghrad AM, Jaafaripooyan E. Resiliency of the Iranian healthcare facilities against the Covid-19 pandemic: challenges and solutions. BMC Health Serv Res. 2023;23(207):1–16.
Mosadeghrad AM, Isfahani P, Eslambolchi L, Zahmatkesh M, Afshari M. Strategies to strengthen a climate-resilient health system: a scoping review. Global Health. 2023;19(1):62.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Social Res Methodol. 2005;8(1):19–32.
Akrami F, Riazi-Isfahani S, Mahdavi hezaveh A, Ghanbari Motlagh A, Najmi M, Afkar M, et al. Iran’s Status of NCDs Prevention and Management Services during COVID-19 Pandemic at PHC Level. SJKU. 2021;26(5):50–68.
Etienne CF, Fitzgerald J, Almeida G, Birmingham ME, Brana M, Bascolo E, Cid C, Pescetto C. COVID-19: transformative actions for more equitable, resilient, sustainable societies and health systems in the Americas. BMJ Global Health. 2020;5(8):e003509.
Tabrizi JS, Raeisi A, Namaki S. Primary health care and COVID-19 Pandemic in the Islamic Republic of Iran. Depict Health. 2022;13(Suppl 1):S1-10.
Danhieux K, Buffel V, Pairon A, Benkheil A, Remmen R, Wouters E, Van Olmen J. The impact of COVID-19 on chronic care according to providers: a qualitative study among primary care practices in Belgium. BMC Fam Pract. 2020;21:1–6.
Goodyear-Smith F, Kidd M, Oseni TIA, Nashat N, Mash R, Akman M, Phillips RL, van Weel C. Internationalexamples of primary care COVID-19 preparedness and response: a comparison of four countries. Fam MedCommunity Health. 2022;10(2):e001608.
Kinder K, Bazemore A, Taylor M, Mannie C, Strydom S, George J, Goodyear-Smith F. Integrating primary care and public health to enhance response to a pandemic. Prim Health Care Res Dev. 2021;22:e27.
De Maeseneer J. Prim Health Care Res Dev. 2021;22:e73.
Westfall JM, Liaw W, Griswold K, Stange K, Green LA, Phillips R, Bazemore A, Jaén CR, Hughes LS, DeVoe J, Gullett H. Uniting public health and primary care for healthy communities in the COVID-19 era and beyond. J Am Board Fam Med. 2021;34(Supplement):S203-9.
Johansen AS, Shriwise A, Lopez-Acuna D, Vracko P. Strengthening the primary health care response to COVID-19: an operational tool for policymakers. Prim Health Care ResDev. 2021;22:e81.
Reath J, Lau P, Lo W, Trankle S, Brooks M, Shahab Y, Abbott P. Strengthening learning and research in health equity–opportunities for university departments of primary health care and general practice. Aust J Prim Health. 2022;29(2):131–6.
Ferenčina J, Tomšič V. COVID-19 clinic as a basis of quality primary health care in the light of the pandemic - an observational study. Med Glas (Zenica). 2022;19(1). https://doi.org/10.17392/1437-21 .
Mosadeghrad AH. Promote COVID-19 vaccination uptake: a letter to editor. Tehran Univ Med Sci J. 2022;80(2):159–60.
Chaiban L, Benyaich A, Yaacoub S, Rawi H, Truppa C, Bardus M. Access to primary and secondary health care services for people living with diabetes and lower-limb amputation during the COVID-19 pandemic in Lebanon: a qualitative study. BMC Health Serv Res. 2022;22(1):593.
Džakula A, Banadinović M, Lovrenčić IL, Vajagić M, Dimova A, Rohova M, Minev M, Scintee SG, Vladescu C, Farcasanu D, Robinson S. A comparison of health system responses to COVID-19 in Bulgaria, Croatia and Romania in 2020. Health Policy. 2022;126(5):456–64.
Ghazi Saeedi M, Tanhapour M. Telemedicine System: A Mandatory Requirement in Today’s World. Payavard. 2022;15(5):490–507.
Ferorelli D, Nardelli L, Spagnolo L, Corradi S, Silvestre M, Misceo F, Marrone M, Zotti F, Mandarelli G, Solarino B, Dell’Erba A. Medical legal aspects of telemedicine in Italy: application fields, professional liability and focus on care services during the COVID-19 health emergency. J Prim CareCommun Health. 2020;11:2150132720985055.
CAS Google Scholar
Fulmer T, Reuben DB, Auerbach J, Fick DM, Galambos C, Johnson KS. Actualizing better health and health care for older adults: commentary describes six vital directions to improve the care and quality of life for all older Americans. Health Aff. 2021;40(2):219–25.
Hernández Rincón EH, Pimentel González JP, Aramendiz Narváez MF, Araujo Tabares RA, Roa González JM. Description and analysis of primary care-based COVID-19 interventions in Colombia. Medwave. 2021;21(3):e8147.
Giannopoulou I, Tsobanoglou GO. COVID-19 pandemic: challenges and opportunities for the Greek health care system. Irish J Psychol Med. 2020;37(3):226–30.
Chow C, Goh SK, Tan CS, Wu HK, Shahdadpuri R. Enhancing frontline workforce volunteerism through exploration of motivations and impact during the COVID-19 pandemic. Int J Disaster Risk Reduct. 2021;1(66):102605.
Alboksmaty A, Kumar S, Parekh R, Aylin P. Management and patient safety of complex elderly patients in primary care during the COVID-19 pandemic in the UK—Qualitative assessment. PLoS One. 2021;16(3):e0248387.
Savoy A, Patel H, Shahid U, Offner AD, Singh H, Giardina TD, Meyer AN. Electronic Co-design (ECO-design) Workshop for Increasing Clinician Participation in the Design of Health Services Interventions: Participatory Design Approach. JMIR Hum Fact. 2022;9(3):e37313.
Tumusiime P, Karamagi H, Titi-Ofei R, Amri M, Seydi AB, Kipruto H, Droti B, Zombre S, Yoti Z, Zawaira F, Cabore J. Building health system resilience in the context of primary health care revitalization for attainment of UHC: proceedings from the Fifth Health Sector Directors’ Policy and Planning Meeting for the WHO African Region. BMC Proc. 2020;14:1–8 (BioMed Central).
Atoofi MK, Rezaei N, Kompani F, Shirzad F, Sh D. Requirements of mental health services during the COVID-19 outbreak: a systematic review. Iran J Psychiatry Clin Psychol. 2020;26(3):264–79.
Mosadeghrad AM, Taherkhani T, Shojaei S, Jafari M, Mohammadi S, Emamzadeh A, Akhavan S. Strengthening primary health care system resilience in COVID-19 pandemic: a scoping review. sjsph 2022;20(1):13-24.
Fotokian Z, Mohammadkhah F. Primary health care as a strategy to fight COVID-19 pandemic: letter to the editor. J Isfahan Med School. 2021;39(630):470–4. https://doi.org/10.22122/jims.v39i630.14016 .
Li D, Howe AC, Astier-Peña MP. Primary health care response in the management of pandemics: Learnings from the COVID-19 pandemic. Atención Primaria. 2021;1(53):102226.
Chua AQ, Tan MMJ, Verma M, Han EKL, Hsu LY, Cook AR, et al. BMJ Global Health. 2020;5(9):e003317.
Eisele M, Pohontsch NJ, Scherer M. Strategies in primary care to face the SARS-CoV-2/COVID-19 pandemic: an online survey. Front Med. 2021;2(8):613537.
Lamberti-Castronuovo A, Valente M, Barone-Adesi F, Hubloue I, Ragazzoni L. Primary health care disaster preparedness: a review of the literature and the proposal of a new framework. Int J Dis Risk Reduct. 2022;2:103278.
Piché-Renaud PP, Ji C, Farrar DS, Friedman JN, Science M, Kitai I, Burey S, Feldman M, Morris SK. Impact of the COVID-19 pandemic on the provision of routine childhood immunizations in Ontario Canada. Vaccine. 2021;39(31):4373–82.
Saxenian H, Alkenbrack S, Freitas Attaran M, Barcarolo J, Brenzel L, Brooks A, Ekeman E, Griffiths UK, Rozario S, Vande Maele N, Ranson MK. Sustainable financing for Immunization Agenda 2030. Vaccine. 2024;42 Suppl 1:S73-S81. https://doi.org/10.1016/j.vaccine.2022.11.037 .
Saso A, Skirrow H, Kampmann B. Impact of COVID-19 on immunization services for maternal and infant vaccines: results of a survey conducted by imprint—the immunising pregnant women and infants network. Vaccines. 2020;8(3):556.
Sagan A, Thomas S, McKee M, Karanikolos M, Azzopardi-Muscat N, de la Mata I, Figueras J, World Health Organization. COVID-19 and health systems resilience: lessons going forwards. Eurohealth. 2020;26(2):20–4.
Celuppi IC, Meirelles BH, Lanzoni GM, Geremia DS, Metelski FK. Management in the care of people with HIV in primary health care in times of the new coronavirus. Revista de Saúde Pública. 2022;1(56):13.
Denis JL, Potvin L, Rochon J, Fournier P, Gauvin L. On redesigning public health in Québec: lessons learned from the pandemic. Can J Public Health= Revue Canadienne de Sante Publique. 2020;111(6):912.
PubMed Google Scholar
Wilson G, Windner Z, Dowell A, Toop L, Savage R, Hudson B. Navigating the health system during COVID-19: primary care perspectives on delayed patient care. N Z Med J. 2021;134(1546):17–27 (PMID: 34855730).
Zhang N, Yang S, Jia P. Cultivating resilience during the COVID-19 pandemic: a socioecological perspective. Annu Rev Psychol. 2022;4(73):575–98. https://doi.org/10.1146/annurev-psych-030221-031857 . (Epub 2021 Sep 27 PMID: 34579547).
Al Ghafri T, Al Ajmi F, Al Balushi L, Kurup PM, Al Ghamari A, Al Balushi Z, Al Fahdi F, Al Lawati H, Al Hashmi S, Al Manji A, Al Sharji A. Responses to the pandemic covid-19 in primary health care in oman: muscat experience. Oman Med J. 2021;36(1):e216.
Adler L, Vinker S, Heymann AD, Van Poel E, Willems S, Zacay G. The effect of the COVID-19 pandemic on primary care physicians in Israel, with comparison to an international cohort: a cross-sectional study. Israel J Health Policy Res. 2022;11(1):1.
Haldane V, Zhang Z, Abbas RF, Dodd W, Lau LL, Kidd MR, Rouleau K, Zou G, Chao Z, Upshur RE, Walley J. National primary care responses to COVID-19: a rapid review of the literature. BMJ Open. 2020;10(12):e041622.
Hussein ES, Al-Shenqiti AM, Ramadan RM. Applications of medical digital technologies for noncommunicable diseases for follow-up during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(19):12682.
Desborough J, Dykgraaf SH, Phillips C, Wright M, Maddox R, Davis S, Kidd M. Lessons for the global primary care response to COVID-19: a rapid review of evidence from past epidemics. Fam Pract. 2021;38(6):811–25.
Sandhu HS, Smith RW, Jarvis T, O’Neill M, Di Ruggiero E, Schwartz R, Rosella LC, Allin S, Pinto AD. Early impacts of the COVID-19 pandemic on public health systems and practice in 3 Canadian provinces from the perspective of public health leaders: a qualitative study. J Public Health Manag Pract. 2022;28(6):702–11.
Farsalinos K, Poulas K, Kouretas D, Vantarakis A, Leotsinidis M, Kouvelas D, Docea AO, Kostoff R, Gerotziafas, Antoniou MN, Polosa R. Improved strategies to counter the COVID-19 pandemic: Lockdowns vs. primary and community healthcare. Toxicol Rep. 2021;8:1–9.
Article CAS PubMed Google Scholar
Fitzpatrick K, Sehgal A, Montesanti S, Pianarosa E, Barnabe C, Heyd A, Kleissen T, Crowshoe L. Examining the role of Indigenous primary healthcare across the globe in supporting populations during public health crises. Global Public Health. 2022;24:1–29.
Liaw ST, Kuziemsky C, Schreiber R, Jonnagaddala J, Liyanage H, Chittalia A, Bahniwal R, He JW, Ryan BL, Lizotte DJ, Kueper JK. Primary care informatics response to Covid-19 pandemic: adaptation, progress, and lessons from four countries with high ICT development. Yearbook Med Inform. 2021;30(01):044–55.
Djalante R, Shaw R, DeWit A. Progress in disaster. Science. 2020;6:100080.
Fatima R, Akhtar N, Yaqoob A, Harries AD, Khan MS. Building better tuberculosis control systems in a post-COVID world: learning from Pakistan during the COVID-19 pandemic. Int J Infect Dis. 2021;1(113):S88-90.
Shin WY, Kim C, Lee SY, Lee W, Kim JH. Role of primary care and challenges for public–private cooperation during the coronavirus disease 2019 pandemic: An expert Delphi study in South Korea. Yonsei Med J. 2021;62(7):660.
Thompson RN, et al. Key questions for modelling COVID-19exit strategies. Proc R Soc B. 2020;287:20201405. https://doi.org/10.1098/rspb.2020.1405 .
Baral P. Health systems and services during COVID-19: lessons and evidence from previous crises: a rapid scoping review to inform the United Nations research roadmap for the COVID-19 recovery. Int J Health Serv. 2021;51(4):474–93.
Daou M, Helou S, El Helou J, El Hachem C, El Helou E. Ensuring care continuity in extreme crises: A participatory action research approach. InMEDINFO 2021: One World, One Health–Global Partnership for Digital Innovation 2022 (pp. 937-941). IOS Press.
Besigye IK, Namatovu J, Mulowooza M. Coronavirus disease-2019 epidemic response in Uganda: the need to strengthen and engage primary healthcare. Afr J Prim Health Care Fam Med. 2020;12(1):1–3.
Silva MJ, Santos P. The impact of health literacy on knowledge and attitudes towards preventive strategies against COVID-19: a cross-sectional study. Int J Environ Res Public Health. 2021;18(10):5421. https://doi.org/10.3390/ijerph18105421 . (PMID:34069438;PMCID:PMC8159089).
Sultana A, Bhattacharya S, Hossain MM. COVID-19 and primary care: a critical need for strengthening emergency preparedness across health systems. J Fam Med Primary Care. 2021;10(1):584–5.
Xu RH, Shi LS, Xia Y, Wang D. Associations among eHealth literacy, social support, individual resilience, and emotional status in primary care providers during the outbreak of the SARS-CoV-2 Delta variant. Digit Health. 2022;25(8):20552076221089788. https://doi.org/10.1177/20552076221089789 . (PMID:35355807;PMCID:PMC8958311).
Bajgain BB, Jackson J, Aghajafari F, Bolo C, Santana MJ. Immigrant Healthcare Experiences and Impacts During COVID-19: A Cross-Sectional Study in Alberta Canada. J Patient Exp. 2022;9:23743735221112708.
Kim AY, Choi WS. Considerations on the implementation of the telemedicine system encountered with stakeholders’ resistance in COVID-19 pandemic. Telemed e-Health. 2021;27(5):475–80.
Tayade MC. Strategies to tackle by primary care physicians to mental health issues in India in COVId-19 pandemic. J Fam Med Prim Care. 2020;9(11):5814–5.
Thomas C. Resilient health and care: Learning the lessons of Covid-19 in the English NHS, IPPR. 2020. http://www.ippr.org/research/publications/resilient-health-and-care .
Saab MM, O’Driscoll M, FitzGerald S, Sahm LJ, Leahy-Warren P, Noonan B, Kilty C, Lyons N, Burns HE, Kennedy U, Lyng Á. Primary healthcare professionals’ perspectives on patient help-seeking for lung cancer warning signs and symptoms: a qualitative study. BMC Prim Care. 2022;23(1):1–5.
Ma L, Han X, Ma Y, Yang Y, Xu Y, Liu D, Yang W, Feng L. Decreased influenza vaccination coverage among Chinese healthcare workers during the COVID-19 pandemic. Infect Dis Pov. 2022;11(05):63–73.
Ismail SA, Lam ST, Bell S, Fouad FM, Blanchet K, Borghi J. Strengthening vaccination delivery system resilience in the context of protracted humanitarian crisis: a realist-informed systematic review. BMC Health Serv Res. 2022;22(1):1–21.
Litke N, Weis A, Koetsenruijter J, Fehrer V, Koeppen M, Kuemmel S, Szecsenyi J, Wensing M. Building resilience in German primary care practices: a qualitative study. BMC Prim Care. 2022;23(1):1–4.
Den Broeder L, South J, Rothoff A, Bagnall AM, Azarhoosh F, Van Der Linden G, Bharadwa M, Wagemakers A. Community engagement in deprived neighbourhoods during the COVID-19 crisis: perspectives for more resilient and healthier communities. Health promotion international. 2022;37(2):daab098.
Sundararaman T, Muraleedharan VR, Ranjan A. Pandemic resilience and health systems preparedness: lessons from COVID-19 for the twenty-first century. J Soc Econ Dev. 2021;23(Suppl 2):1–11. https://doi.org/10.1007/s40847-020-00133-x . (Epub ahead of print. PMID: 34720480; PMCID: PMC7786882).
Ferreira NN, Garibaldi PM, Moraes GR, Moura JC, Klein TM, Machado LE, Scofoni LF, Haddad SK, Calado RT, Covas DT, Fonseca BA. The impact of an enhanced health surveillance system for COVID-19 management in Serrana, Brazil. Public Health Pract. 2022;1(4):100301.
Harzheim E, Martins C, Wollmann L, Pedebos LA, Faller LD, Marques MD, Minei TS, Cunha CR, Telles LF, Moura LJ, Leal MH. Federal actions to support and strengthen local efforts to combat COVID-19: Primary Health Care (PHC) in the driver’s seat. Ciência Saúde Coletiva. 2020;5(25):2493–7.
Smaggus A, Long J, Ellis LA, Clay-Williams R, Braithwaite J. Government actions and their relation to resilience in healthcare during the COVID-19 pandemic in New South Wales, Australia and Ontario, Canada. Int J Health Policy Manag. 2022;11(9):1682–94. https://doi.org/10.34172/ijhpm.2021.67 .
Tselebis A, Pachi A. Primary mental health care in a New Era. Healthcare (Basel). 2022;10(10):2025. https://doi.org/10.3390/healthcare10102025 . (PMID:36292472;PMCID:PMC9601948).
Rieckert A, Schuit E, Bleijenberg N, Ten Cate D, de Lange W, de Man-van Ginkel JM, Mathijssen E, Smit LC, Stalpers D, Schoonhoven L, Veldhuizen JD, Trappenburg JC. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open. 2021;11(1):e043718. https://doi.org/10.1136/bmjopen-2020-043718 .
Basu P, Alhomoud S, Taghavi K, Carvalho AL, Lucas E, Baussano I. Cancer screening in the coronavirus pandemic era: adjusting to a new situation. JCO Global Oncol. 2021;7(1):416–24.
Rieckert A, Schuit E, Bleijenberg N, et al. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open. 2021;11:e043718. https://doi.org/10.1136/bmjopen-2020-043718 .
Shaikh BT. Strengthening health system building blocks: configuring post-COVID-19 scenario in Pakistan. Prim Health Care Res Dev. 2021;22:e9 Cambridge University Press.
Franzosa E, Gorbenko K, Brody AA, Leff B, Ritchie CS, Kinosian B, Ornstein KA, Federman AD. “At home, with care”: lessons from New York City home-based primary care practices managing COVID-19. J Am Geriatr Soc. 2021;69(2):300–6.
Adhikari B, Mishra SR, Schwarz R. Transforming Nepal’s primary health care delivery system in global health era: addressing historical and current implementation challenges. Global Health. 2022;18(1):1–2.
Mas Bermejo P, Sánchez Valdés L, Somarriba López L, Valdivia Onega NC, Vidal Ledo MJ, Alfonso Sánchez I, et al. Equity and the Cuban National Health System's response to COVID-19. Rev Panam Salud Publica. 2021;45:e80. https://doi.org/10.26633/RPSP.2021.80 .
Gong F, Hu G, Lin H, Sun X, Wang W. Integrated Healthcare Systems Response Strategies Based on the Luohu Model During the COVID-19 Epidemic in Shenzhen, China. Int J Integr Care. 2021;21(1):1. https://doi.org/10.5334/ijic.5628 .
Gomez T, Anaya YB, Shih KJ, Tarn DM. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J Am Board Fam Med. 2021;34(Supplement):S61-70.
Teng K, Russo F, Kanuch S, Caron A. Virtual Care Adoption-Challenges and Opportunities From the Lens of Academic Primary Care Practitioners. J Public Health Manag Pract. 2022;28(6):599–602. https://doi.org/10.1097/PHH.0000000000001548 . (Epub 2022 Aug 27. PMID: 36037465; PMCID: PMC9555588).
Anaya YB, Mota AB, Hernandez GD, Osorio A, Hayes-Bautista DE. Post-pandemic telehealth policy for primary care: an equity perspective. J Am Board Fam Med. 2022;35(3):588–92.
Florea M, Lazea C, Gaga R, Sur G, Lotrean L, Puia A, Stanescu AM, Lupsor-Platon M, Florea H, Sur ML. Lights and shadows of the perception of the use of telemedicine by Romanian family doctors during the COVID-19 pandemic. Int J Gen Med. 2021;14:1575.
Selick A, Durbin J, Hamdani Y, Rayner J, Lunsky Y. Accessibility of Virtual Primary Care for Adults With Intellectual and Developmental Disabilities During the COVID-19 Pandemic: Qualitative Study. JMIR Form Res 2022;6(8):e38916. https://formative.jmir.org/2022/8/e38916 . https://doi.org/10.2196/38916 .
Frost R, Nimmons D, Davies N. Using remote interventions in promoting the health of frail older persons following the COVID-19 lockdown: challenges and solutions. J Am Med Direct Assoc. 2020;21(7):992.
Suija K, Mard LA, Laidoja R, et al. Experiences and expectation with the use of health data: a qualitative interview study in primary care. BMC Prim Care. 2022;23:159. https://doi.org/10.1186/s12875-022-01764-1 .
Sullivan EE, McKinstry D, Adamson J, Hunt L, Phillips RS, Linzer M. Burnout Among Missouri Primary Care Clinicians in 2021: Roadmap for Recovery? Mo Med. 2022;119(4):397–400 (PMID: 36118800; PMCID: PMC9462904).
Tang C, Chen X, Guan C, Fang P. Attitudes and Response Capacities for Public Health Emergencies of Healthcare Workers in Primary Healthcare Institutions: A Cross-Sectional Investigation Conducted in Wuhan, China, in 2020. Int Environ Res Public Health. 2022;19(19):12204. https://doi.org/10.3390/ijerph191912204 .
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, Chua A, Verma M, Shrestha P, Singh S, Perez T. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964–80.
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, Chua A, Verma M, Shrestha P, Singh S, Perez T, Tan SM, Bartos M, Mabuchi S, Bonk M, McNab C, Werner GK, Panjabi R, Nordström A, Legido-Quigley H. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964-80. https://doi.org/10.1038/s41591-021-01381-y .
Berger Z, De Jesus VA, Assoumou SA, Greenhalgh T. Long COVID and health inequities: the role of primary care. Milbank Q. 2021;99(2):519.
Haldane V, Dodd W, Kipp A, Ferrolino H, Wilson K, Servano D, Lau LL, Wei X. Extending health systems resilience into communities: a qualitative study with community-based actors providing health services during the COVID-19 pandemic in the Philippines. BMC Health Serv Res. 2022;22(1):1–2.
Haun JN, Cotner BA, Melillo C, Panaite V, Messina W, Patel-Teague S, Zilka B. Proactive integrated virtual healthcare resource use in primary care. BMC Health Serv Res. 2021;21(1):1–4.
Kelly F, Uys M, Bezuidenhout D, Mullane SL, Bristol C. Improving Healthcare Worker Resilience and Well-Being During COVID-19 Using a Self-Directed E-Learning Intervention. Front Psychol. 2021;12:748133. https://doi.org/10.3389/fpsyg.2021.748133 .
Thekkur P, Fernando M, Nair D, Kumar AMV, Satyanarayana S, Chandraratne N, Chandrasiri A, Attygalle DE, Higashi H, Bandara J, Berger SD, Harries AD. Primary Health Care System Strengthening Project in Sri Lanka: Status and Challenges with Human Resources, Information Systems, Drugs and Laboratory Services. Healthcare. 2022;10(11):2251. https://doi.org/10.3390/healthcare10112251 .
Balogun M, Banke-Thomas A, Gwacham-Anisiobi U, Yesufu V, Ubani O, Afolabi BB. Actions and AdaptationsImplemented for Maternal, Newborn and Child Health Service Provision During the Early Phase of the COVID-19 Pandemic in Lagos, Nigeria: Qualitative Study of Health Facility Leaders. Ann Glob Health. 2022;88(1):13. https://doi.org/10.5334/aogh.3529 .
Llamas S, MP AP, Felipe P. Patient safety training and a safe teaching in primary care. Aten Primaria. 2021;53 Suppl 1(Suppl 1):102199.
Eze-Emiri C, Patrick F, Igwe E, Owhonda G. Retrospective study of COVID-19 outcomes among healthcare workers in Rivers State, Nigeria. BMJ Open. 2022;12(11):e061826.
Golechha M, Bohra T, Patel M, Khetrapal S. Healthcare worker resilience during the COVID-19 pandemic: a qualitative study of primary care providers in India. World Med Health Policy. 2022;14(1):6–18.
Gómez-Restrepo C, Cepeda M, Torrey WC, Suarez-Obando F, Uribe-Restrepo JM, Park S, Acosta MP, Camblor PM, Castro SM, Aguilera-Cruz J, González L. Perceived access to general and mental healthcare in primary care in Colombia during COVID-19: A cross-sectional study. Frontiers in Public Health. 2022;10:896318.
Nejat N, Borzabadi Farahani Z. COVID-19 pandemic: opportunities for continuing nursing professional development. J Med Educ Dev. 2022;14(44):1–2.
DeVoe JE, Cheng A, Krist A. JAMA Health Forum. 2020;1(4):e200423.
Hoeft TJ, Hessler D, Francis D, Gottlieb LM. Applying lessons from behavioral health integration to social care integration in primary care. Ann Fam Med. 2021;19(4):356–61.
Silsand L, Severinsen GH, Berntsen G. Preservation of Person-Centered care through videoconferencing for patient follow-up during the COVID-19 pandemic: case study of a multidisciplinary care team. JMIR Format Res. 2021;5(3):e25220.
Sullivan E, Phillips R.S. Sustaining primary care teams in the midst of a pandemic. Isr J Health Policy Res. 2020; 9. 77. https://doi.org/10.1186/s13584-020-00434-w .
Abd El Kader AI, Faramawy MA. COVID-19 anxiety and organizational commitment among front line nurses: Perceived role of nurse managers' caring behavior. Nurs Pract Today. 2022;9(1):X.
Croghan IT, Chesak SS, Adusumalli J, Fischer KM, Beck EW, Patel SR, Ghosh K, Schroeder DR, Bhagra A. Stress, resilience, and coping of healthcare workers during the COVID-19 pandemic. J Prim Care Commun Health. 2021;12:21501327211008450.
Aragonès E, del Cura-González I, Hernández-Rivas L, Polentinos-Castro E, Fernández-San-Martín MI, López-Rodríguez JA, Molina-Aragonés JM, Amigo F, Alayo I, Mortier P, Ferrer M. Psychological impact of the COVID-19 pandemic on primary care workers: a cross-sectional study. Br J Gen Pract. 2022;72(720):e501-10.
Franck E, Goossens E, Haegdorens F, Geuens N, Portzky M, Tytens T, Dilles T, Beeckman K, Timmermans O, Slootmans S, Van Rompaey B. Role of resilience in healthcare workers’ distress and somatization during the COVID-19 pandemic: a cross-sectional study across Flanders Belgium. Nurs Open. 2022;9(2):1181–9.
DeTore NR, Sylvia L, Park ER, Burke A, Levison JH, Shannon A, et al. J Psychiatr Res. 2022;146:228–33.
Shi LS, Xu RH, Xia Y, Chen DX, Wang D. The impact of COVID-19-related work stress on the mental health of primary healthcare workers: the mediating effects of social support and resilience. Front Psychol. 2022;21(12):800183. https://doi.org/10.3389/fpsyg.2021.800183 . (PMID:35126252;PMCID:PMC8814425).
Golden EA, Zweig M, Danieletto M, Landell K, Nadkarni G, Bottinger E, Katz L, Somarriba R, Sharma V, Katz CL, Marin DB. A resilience-building app to support the mental health of health care workers in the COVID-19 era: Design process, distribution, and evaluation. JMIR Format Res. 2021;5(5):e26590.
Chan AY, Ting C, Chan LG, Hildon ZJ. “The emotions were like a roller-coaster”: a qualitative analysis of e-diary data on healthcare worker resilience and adaptation during the COVID-19 outbreak in Singapore. Hum Resour Health. 2022;20(1):60.
Ashley C, James S, Williams A, Calma K, Mcinnes S, Mursa R, Stephen C, Halcomb E. The psychological well-being of primary healthcare nurses during COVID-19: a qualitative study. J Adv Nurs. 2021;77(9):3820–8.
Carmona LE, Nielfa MD, Alvarado AL. The Covid-19 pandemic seen from the frontline. Int Braz J Urol. 2020;27(46):181–94.
Delobelle PA, Abbas M, Datay I, De Sa A, Levitt N, Schouw D, Reid S. Non-communicable disease care and management in two sites of the Cape Town Metro during the first wave of COVID-19: A rapid appraisal. Afr J Prim Health Care Fam Med. 2022;14(1):e1-e7. https://doi.org/10.4102/phcfm.v14i1.3215 .
Luciani S, Agurto I, Caixeta R, Hennis A. Prioritizing noncommunicable diseases in the Americas region in the era of COVID-19. Rev Panam Salud Publica. 2022;46:e83. https://doi.org/10.26633/RPSP.2022.83 .
Cabral IE, Pestana-Santos M, Ciuffo LL, Nunes YDR, Lomba MLLF. Child health vulnerabilities during the COVID-19 pandemic in Brazil and Portugal. Rev Lat Am Enfermagem. 2021;29:e3422. https://doi.org/10.1590/1518-8345.4805.3422 . (Published 2021 Jul 2).
Ludin N, Holt-Quick C, Hopkins S, Stasiak K, Hetrick S, Warren J, Cargo T. A Chatbot to support young people during the COVID-19 Pandemic in New Zealand: evaluation of the real-world rollout of an open trial. J Med Internet Res. 2022;24(11):e38743.
Breton M, Deville-Stoetzel N, Gaboury I, Smithman MA, Kaczorowski J, Lussier MT, Haggerty J, Motulsky A, Nugus P, Layani G, Paré G. Telehealth in primary healthcare: a portrait of its rapid implementation during the COVID-19 pandemic. Healthcare Policy. 2021;17(1):73.
Knop M, Mueller M, Niehaves B. Investigating the use of telemedicine for digitally mediated delegation in team-based primary care: mixed methods study. J Med Internet Res. 2021;23(8):e28151.
Zamiela C, Hossain NUI, Jaradat R. Enablers of resilience in the healthcare supply chain: A case study of U.S healthcare industry during COVID-19 pandemic. Res Transport Econ. 2022;93:101174. https://doi.org/10.1016/j.retrec.2021.101174 . Epub 2021 Dec 24. PMCID: PMC9675944.
Lukong AM, Jafaru Y. Covid-19 pandemic challenges, coping strategies and resilience among healthcare workers: a multiple linear regression analysis. Afr J Health Nurs Midwifery. 2021;4:16–27.
Hearnshaw S, Serban S, Mohammed I, Zubair A, Jaswal D, Grant S. A local dental network approach to the COVID-19 pandemic: innovation through collaboration. Prim Dental J. 2021;10(1):33–9.
Haase CB, Bearman M, Brodersen J, Hoeyer K, Risor T. ‘You should see a doctor’, said the robot: Reflections on a digital diagnostic device in a pandemic age. Scand J Public Health. 2021;49(1):33–6.
Otu A, Okuzu O, Ebenso B, Effa E, Nihalani N, Olayinka A, Yaya S. Introduction of mobilehealth tools to support COVID-19 training and surveillance in Ogun State Nigeria. Frontiers in Sustainable Cities. 2021;3:638278:1-9.
Ibragimov K, Palma M, Keane G, Ousley J, Crowe M, Carreño C, Casas G, Mills C, Llosa A. Shifting to Tele-Mental Health in humanitarian and crisis settings: an evaluation of Médecins Sans Frontières experience during the COVID-19 pandemic. Conflict Health. 2022;16(1):1–5.
Wherton J, Greenhalgh T, Hughes G, Shaw SE. The role of information infrastructures in scaling up video consultations during COVID-19: mixed methods case study into opportunity, disruption, and exposure. J Med Internet Res. 2022;24(11):e42431. https://doi.org/10.2196/42431 . (PMID:36282978;PMCID:PMC9651004).
Jonnagaddala J, Godinho MA, Liaw ST. From telehealth to virtual primary care in Australia? a rapid scoping review. Int J Med Inform. 2021;1(151):104470.
Tanemura N, Chiba T. The usefulness of a checklist approach-based confirmation scheme in identifying unreliable COVID-19-related health information: a case study in Japan. Humanit Soc Sci Commun. 2022;9(1):270. https://doi.org/10.1057/s41599-022-01293-3 . (Epub 2022 Aug 15. PMID: 35990766; PMCID: PMC9376898).
Zaroushani V. Occupational safety and health and response to COVID-19 using the fourth industrial revolution technologies. J Health Saf Work. 2020;10(4):329–48.
Binagwaho A, Hirwe D, Mathewos K. Health System Resilience: Withstanding Shocks and Maintaining Progress. Glob Health Sci Pract. 2022;10(Suppl 1):e2200076. https://doi.org/10.9745/GHSP-D-22-00076 .
Freed SL, Thiele D, Gardner M, Myers E. COVID-19 evaluation and testing strategies in a federally qualified health center. Am J Public Health. 2022;112(S3):S284-7.
Levy P, McGlynn E, Hill AB, Zhang L, Korzeniewski SJ, Foster B, Criswell J, O’Brien C, Dawood K, Baird L, Shanley CJ. From pandemic response to portable population health: a formative evaluation of the Detroit mobile health unit program. Plos One. 2021;16(11):e0256908.
Corwin C, Sinnwell E, Culp K. A mobile primary care clinic mitigates an early COVID-19 outbreak among migrant farmworkers in Iowa. J Agromed. 2021;26(3):346–51.
Mills WR, Buccola JM, Sender S, Lichtefeld J, Romano N, Reynolds K, Price M, Phipps J, White L, Howard S. Home-based primary care led-outbreak mitigation in assisted living facilities in the first 100 days of coronavirus disease 2019. J Am Med Direct Assoc. 2020;21(7):951–3.
Sigurdsson EL, Blondal AB, Jonsson JS, Tomasdottir MO, Hrafnkelsson H, Linnet K, Sigurdsson JA. How primary healthcare in Iceland swiftly changed its strategy in response to the COVID-19 pandemic. BMJ Open. 2020;10(12):e043151. https://doi.org/10.1136/bmjopen-2020-043151 . (PMID:33293329;PMCID:PMC7722808).
Mirsky JB, Thorndike AN. Virtual group visits: hope for improving chronic disease management in primary care during and after the COVID-19 pandemic. Am J Health Promot. 2021;35(7):904–7.
Lauriola P, Martín-Olmedo P, Leonardi GS, Bouland C, Verheij R, Dückers ML, Van Tongeren M, Laghi F, Van Den Hazel P, Gokdemir O, Segredo E. On the importance of primary and community healthcare in relation to global health and environmental threats: lessons from the COVID-19 crisis. BMJ Global Health. 2021;6(3):e004111.
Stengel S, Roth C, Breckner A, et al. Resilience of the primary health care system – German primary care practitioners’ perspectives during the early COVID-19 pandemic. BMC Prim Care. 2022;23:203. https://doi.org/10.1186/s12875-022-01786-9 .
Adu PA, Stallwood L, Adebola SO, Abah T, Okpani AI. The direct and indirect impact of COVID-19 pandemic on maternal and child health services in Africa: a scoping review. Global Health Res Policy. 2022;7(1):1–4.
Segal M, Giuffrida P, Possanza L, Bucciferro D. The critical role of health information technology in the safe integration of behavioral health and primary care to improve patient care. J Behav Health Serv Res. 2022;49(2):221–30. https://doi.org/10.1007/s11414-021-09774-0 . (Epub 2021 Oct 19. PMID: 34668115; PMCID: PMC8525847).
Gallardo-Rincón H, Gascon JL, Martínez-Juárez LA, Montoya A, Saucedo-Martínez R, Rosales RM, Tapia-Conyer R. MIDO COVID: A digital public health strategy designed to tackle chronic disease and the COVID-19 pandemic in Mexico. Plos One. 2022;17(11):e0277014.
Shah SS, Safa A, Johal K, et al. A prospective observational real world feasibility study assessing the role of app-based remote patient monitoring in reducing primary care clinician workload during the COVID pandemic. BMC Fam Pract. 2021;22:248. https://doi.org/10.1186/s12875-021-01594-7 .
Lu M, Liao X. Access to care through telehealth among US Medicare beneficiaries in the wake of the COVID-pandemic. Front Public Health. 2022;10:946944.
Reges O, Feldhamer I, Wolff Sagy Y, Lavie G. Factors associated with using telemedicine in the primary care clinics during the COVID-19 pandemic in Israel. Int J Environ Res Public Health. 2022;19(20):13207.
Neves AL, Li E, Gupta PP, Fontana G, Darzi A. Virtual primary care in high-income countries during the COVID-19 pandemic: Policy responses and lessons for the future. Eur J Gen Pract. 2021;27(1):241–7.
Fadul N, Regan N, Kaddoura L, Swindells S. A midwestern academic HIV clinic operation during the COVID-19 pandemic: implementation strategy and preliminary outcomes. J International Assoc Provid AIDS Care (JIAPAC). 2021;2(20):23259582211041424.
Gray C, Ambady L, Chao S PharmD, Smith W MPH, Yoon J. Virtual Management of Chronic Conditions During the COVID-19 Pandemic: Insights From Primary Care Providers and Clinical Pharmacists. Mil Med. 2023;188(7-8):e2615-e2620. https://doi.org/10.1093/milmed/usac277 .
Hincapié MA, Gallego JC, Gempeler A, Piñeros JA, Nasner D, Escobar MF. Implementation and usefulness of telemedicine during the COVID-19 pandemic: a scoping review. J Prim Care Commun Health. 2020;11:2150132720980612.
Calvo-Paniagua J, Díaz-Arribas MJ, Valera-Calero JA, et al. A tele-health primary care rehabilitation program improves self-perceived exertion in COVID-19 survivors experiencing Post-COVID fatigue and dyspnea: A quasi-experimental study. PLoS One. 2022;17(8):e0271802. https://doi.org/10.1371/journal.pone.0271802 . (Published 2022 Aug 4).
Chen K, Davoodi NM, Strauss DH, Li M, Jiménez FN, Guthrie KM, et al. J Appl Gerontol. 2022;41(11):2282–95.
Murphy M, Scott LJ, Salisbury C, Turner A, Scott A, Denholm R, Lewis R, Iyer G, Macleod J, Horwood J. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gen Pract. 2021;71(704):e166-77.
Maria AR, Serra H, Heleno B. Teleconsultations and their implications for health care: a qualitative study on patients’ and physicians’ perceptions. Int J Med Inform. 2022;1(162):104751.
Liddy C, Singh J, Mitchell R, Guglani S, Keely E. How one eConsult service is addressing emerging COVID-19 questions. J Am Board Fam Med. 2022;35(3):601–4.
Schow DC, Thomson A, Trusty WT, Buchi-Fotre L. Use of a research as intervention approach to explore telebehavioral health services during the COVID-19 pandemic in Southeastern Idaho. J Prim Care Commun Health. 2022;13:21501319211073000.
Bruns BE, Lorenzo-Castro SA, Hale GM. Controlling blood pressure during a pandemic: The impact of telepharmacy for primary care patients. J Pharm Pract. 2022;27:08971900221136629.
Pradhan NA, Samnani AA, Abbas K, Rizvi N. Resilience of primary healthcare system across low-and middle-income countries during COVID-19 pandemic: a scoping review. Health Res Policy Syst. 2023;21(1):98.
Esfahani P, Mosadeghrad AM, Akbarisari A. The success of strategic planning in health care organizations of Iran. Int J Health Care Qual Assur. 2018;31(6):563–74.
Otu A, Okuzu O, Ebenso B, Effa E, Nihalani N, Olayinka A, Yaya S. Introduction of mobile health tools to support COVID-19 training and surveillance in Ogun State Nigeria. Front Sustain Cities. 2021;5(3):638278.
Ndayishimiye C, Lopes H, Middleton J. A systematic scoping review of digital health technologies during COVID-19: a new normal in primary health care delivery. Health Technol. 2023;13(2):273–84.
Ghiasipour M, Mosadeghrad AM, Arab M, Jaafaripooyan E. Leadership challenges in health care organizations: The case of Iranian hospitals. Med J Islam Repub Iran. 2017;31(1):560–7.
Download references
Acknowledgments
We would like to thank Dr. Arshad Altaf for his invaluable comments on the earlier drafts of this work.
Funding for this project was provided by the World Health Organization Eastern Mediterranean Region.
Author information
Authors and affiliations.
Health policy and management, Health Economics and Management Department, Tehran University of Medical Sciences, Tehran, Iran
Ali Mohammad Mosadeghrad
Health policy, School of Nursing and Midwifery, Saveh University of Medical Sciences, Saveh, Iran
Mahnaz Afshari
Health management, School of Public Health, Zabol University of Medical Sciences, Zabol, Iran
Parvaneh Isfahani
Health services management, Health Economics and Management Department, Tehran University of Medical Sciences, Tehran, Iran
Farahnaz Ezzati, Mahdi Abbasi, Shahrzad Akhavan Farahani & Leila Eslambolchi
Health Management, School of Business and Management, Royal Holloway University of London, London, UK
Maryam Zahmatkesh
You can also search for this author in PubMed Google Scholar
Contributions
LE, MA, MZ and AMM participated in the design of the study. LE, AMM, MA, MZ, PI, FE, MA and SHA undertook the literature review process. All authors drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Leila Eslambolchi .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Tehran University of Medical Science (Approval ID: IR.TUMS.SPH.REC.1401.0979).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mosadeghrad, A.M., Afshari, M., Isfahani, P. et al. Strategies to strengthen the resilience of primary health care in the COVID-19 pandemic: a scoping review. BMC Health Serv Res 24 , 841 (2024). https://doi.org/10.1186/s12913-024-11278-4
Download citation
Received : 14 January 2024
Accepted : 03 July 2024
Published : 25 July 2024
DOI : https://doi.org/10.1186/s12913-024-11278-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Primary health care system
- Strengthening strategies
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 30 July 2024
Escape room design in training crew resource management in acute care: a scoping review
- Gerald J. Jaspers 3 ,
- Simone Borsci 1 , 2 ,
- Johannes G. van der Hoeven 3 ,
- Wietske Kuijer-Siebelink 4 , 5 &
- Joris Lemson 3
BMC Medical Education volume 24 , Article number: 819 ( 2024 ) Cite this article
13 Accesses
Metrics details
Effective teamwork is crucial to providing safe and high-quality patient care, especially in acute care. Crew Resource Management (CRM) principles are often used for training teamwork in these situations, with escape rooms forming a promising new tool. However, little is known about escape room design characteristics and their effect on learning outcomes. We investigated the current status of design characteristics and their effect on learning outcomes for escape room-based CRM/teamwork training for acute care professionals. We also aimed to identify gaps in literature to guide further research.
Multiple databases were searched for studies describing the design and effect of escape rooms aimed training CRM/teamwork in acute care professionals and in situations that share characteristics. A standardized process was used for screening and selection. An evidence table that included study characteristics, design characteristics and effect of the escape room on learning outcomes was used to extract data. Learning outcomes were graded according to IPE expanded typology of Kirkpatrick’s levels of learning outcome and Medical Education Research Study Quality Instrument (MERSQI) scores were calculated to assess methodology.
Fourteen studies were included. Common design characteristics were a team size of 4–6 participants, a 40-minute time limit, linear puzzle organization and use of briefing and structured debriefing. Information on alignment was only available in five studies and reporting on several other educational and escape room design characteristics was low. Twelve studies evaluated the effect of the escape room on teamwork: nine evaluated reaction (Kirkpatrick level 1; n = 9), two evaluated learning (Kirkpatrick level 2) and one evaluated both. Overall effect on teamwork was overtly positive, with little difference between studies. Together with a mean MERSQI score of 7.0, this precluded connecting specific design characteristics to the effect on learning outcomes.
Conclusions
There is insufficient evidence if and how design characteristics affect learning outcomes in escape rooms aimed at training CRM/teamwork in acute care professionals. Alignment of teamwork with learning goals is insufficiently reported. More complete reporting of escape rooms aimed at training CRM/teamwork in acute care professionals is needed, with a research focus on maximizing learning potential through design.
Peer Review reports
Effective teamwork is crucial to providing safe and high-quality patient care, especially in acute care settings where stakes are high and time-sensitive decisions and actions are required. In the past two decades, there has been a growing interest in training teamwork in these settings and its effectiveness [ 1 , 2 ]. Crew (or Crisis) Resource Management (CRM) principles are frequently used for structuring, improving and training teamwork and communication in these settings [ 1 ]. CRM identifies factors in, and threats to effective teamwork and offers tools to improve teamwork and communication and prevent error. Substantial evidence shows that training improves CRM skills in health care professionals on multiple learning outcome levels and might lead to safer care [ 3 ]. To achieve these outcomes effective training is necessary [ 3 , 4 , 5 , 6 , 7 ]. CRM training varies considerably and can include a wide range of interventions, like lectures, table-top games, simulation, etc. [ 4 ]. Practice-based interventions, like simulation, are often included in CRM training. CRM skills are trained by applying in simulation and this was found to be more effective than other instructional methods [ 8 , 9 , 10 ].
Other practice-based interventions might also be able to fulfill this role. A new, innovative and practice-based training tool in CRM/teamwork training is the use of escape rooms. Escape rooms are, as defined by Nicholson [ 11 ] ‘live-action team-based games where players discover clues, solve puzzles, and accomplish tasks in one or more rooms in order to accomplish a specific goal (usually escaping from the room) in a limited amount of time’. They offer great potential for teamwork training in acute care as they are, by definition, time-limited team-based activities that both force and facilitate teamwork, with the need to coordinate tasks and communicate [ 11 ]. Their use in healthcare, as well as in education in general, has increased significantly in recent years [ 12 , 13 ]. The high learning potential is also reflected in that they are often enjoyed by participants and, albeit limited, in healthcare students have shown an increase in skills, knowledge, and attitudes [ 12 ].
Educational intervention design characteristics may affect learning outcomes. Several considerations have been proposed for the design requirement for developing educational escape rooms in healthcare settings in general [ 14 , 15 ] and also for teamwork [ 16 ], but such considerations are often based on theory and practice experience, and not on a synthesis of the available evidence. There seems to be consensus that alignment of the learning goals with the escape room is an important requirement. Recent reviews in escape rooms in healthcare students [ 12 ] and higher education (including medical escape rooms) [ 17 ] underscores this, but also identify a lack of evidence on the impact design characteristics have on learning outcomes [ 12 ]. Little to no guidelines are available regarding how escape rooms that aim at improving CRM/teamwork for the acute care setting should be designed, or how to maximize learning outcomes through design in this setting. Therefore, the question driving our review was: what are the design requirements that should be taken into account in the design of such escape rooms.
In the present study, we aim to identify common design characteristics, relate these to learning outcomes and thereby identifying a set of evidence-based design requirements for escape rooms to train CRM/teamwork in acute care. To achieve these goals, we performed a scoping review of the literature regarding design characteristics and their effect on learning outcomes in escape rooms used for crew resource management and/or teamwork training for healthcare professionals in acute care settings.
Research questions
To guide the development of physical escape rooms aimed at improving crew resource management/teamwork in healthcare personnel in acute care settings, the present review investigated the answer to the following questions:
Which common design characteristics can be derived from peer-reviewed literature?
What common design characteristics can be derived from similar situations:
Escape rooms assessing students instead of healthcare personnel.
Virtual escape rooms instead of physical escape rooms.
Escape rooms used for training CRM in situations with similar characteristics to acute care: time-limited, high stakes, high-pressure, high safety (i.e., aviation, military, etc.)
When connecting design characteristics to learning outcomes, which design requirements can be identified that maximize learning outcomes?
What are the major gaps in the evidence on design requirements for optimizing learning outcomes?
To best meet these broad objectives, and analyze a range of different study designs, we used a scoping review design. The review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-analysis Protocols extension for scoping reviews (PRISMA-ScR) [ 18 , 19 ].
Eligibility criteria
Inclusion criteria were drafted to match the primary aim: studies describing the design of physical escape rooms to train crew resource management in healthcare professionals working in acute care . As CRM is about teamwork, all studies on escape rooms aimed at teamwork, or related terms were included. Escape rooms can have other learning goals (i.e., knowledge or skills) besides teamwork that influences design. To be included, training CRM/teamwork had to be one of the main aims. If studies had a different focus than describing design, they were included if sufficient detail on design was provided. This was defined as at least a puzzle scheme and description of the puzzle organization.
To enrich the data, we also looked at studies describing escape rooms in situations that share characteristics. To balance between precision on the one hand, and not miss relevant publications on the other, studies that differed on one aspect of the primary aim were included. This was defined as studies describing acute care escape rooms, but only fulfilling 2 of the 3 other criteria: (i) virtual instead of a physical escape room; (ii) students instead of healthcare professionals; (iii) Settings with similar characteristics to acute care: time-limited, high stakes, high-pressure, high safety (for example aviation, military). These studies were grouped as ‘virtual’, ‘students’, and ‘setting’ and are mentioned throughout the review as such.
Only studies that were full-text, empirical and published in a peer-reviewed journal were included. There was no limitation on study type or design (i.e. qualitative, qualitative) but we excluded letters to the editor, conference papers/abstract, etc. because of insufficient detail. Finally, we included studies that did not describe design, but measured effectiveness/evaluation of an escape room of which the design was described in an included article. These studies were used for the analysis of the effect of the design criteria on learning outcomes.
Databases and search strategy
For full information on the selection of databases and the search strategy, we refer to additional file 1 . An extensive range of databases were searched (CINAHL, EMBASE, ERIC, MEDLINE (PubMed), PsycINFO, Scopus, and Web of Science). To cross-check no relevant articles were missed, three additional sources were used: (1) Forward and backward citation tracking of articles eligible for inclusion, (2) Elicit [ 20 ] (an AI tool that uses language models to find relevant papers), (3) Google Scholar [ 21 ].
The search strategy was drafted by one author (GJ) and iteratively refined through team discussion. A librarian, experienced in systematic searches, evaluated and further refined the search strategy.
The search focused on two keywords: escape room and Crew Resource Management/teamwork. Both keywords were maximally broadened. For escape room, we added all alternative and related terms. For crew resource management/teamwork, we also included related and alternative terms. Additionally, we added CRM-elements like situational awareness, communication, leadership, task allocation, and decision-making. Databases were checked for relevant MeSH (or equivalent) terms and additionally, all terms were used in a title, abstract, and keyword search. No language restrictions were applied, but the search was limited to studies published after the year 2000, as the first well-documented escape room was not described until 2007 [ 11 ]. The search was completed in June 2023. Results were imported into EndNote (EndNote™, version 20, Clavirate, Philadelphia, U.S.). After removing duplicates the results were exported to Rayyan [ 22 ] for screening.
Title and abstract of all articles were independently screened for eligibility by two authors (GJ and JL). Any discrepancies were solved through discussion. In the second stage, two authors (GJ and JL) screened the full texts of all included articles against the eligibility criteria; any discrepancies were resolved in discussion with a third author (SB).
Data items and charting process
Using an iterative process, a set of data items to extract was defined. First three categories were determined in which to categorize and structure the data and reporting:
Study characteristics.
Educational and escape room design characteristics.
Effect on learning.
Specific data extraction items in these categories were identified through studying reviews and frameworks: educational escape room design [ 14 , 15 , 16 , 17 , 23 , 24 , 25 , 26 ], healthcare CRM training/simulation [ 4 , 27 , 28 ], and interprofessional education [ 29 ]. All authors critically reviewed the data-items, added or deleted items and through iterative discussion, a final selection was made. In Additional file 2 the full list of data-items can be found as column headings.
In ‘study characteristics’, data were collected on subjects, setting and aim of the study and escape room and was used to provide an overview of the included studies. In the ‘educational and escape room design characteristics’, data that guided the design were extracted. Alignment of learning goals with the escape room is considered essential in design [ 16 , 17 ]. We used this data item to extract data on explicit information how alignment was achieved. However, all design characteristics relate to alignment. These separate characteristics were identified using the process mentioned above. For example, for the educational underpinning items like learning theory and CRM/teamwork model, briefing and debriefing technique were extracted. As teams in acute care often consist of members with different roles and from different backgrounds, the interprofessional educational (IPE) characteristics [ 29 ] interdependence (the need for a contribution from the expertise of all team-members [ 29 ]) and embodiment (also called immersion; the feeling of being immersed in a situation that feels authentic and that is similar to working in their profession) were included. Also data on the escape room design characteristics were extracted, such as team size, puzzle organization (open, linear/sequential, path-based, pyramid or complex (for more info and graphical representation see reference [ 11 ]) and facilitator role.
In the ‘effect on learning’ category, data were collected on the effect of the escape room on teamwork. To define design requirements, this data was used link the design characteristics to their effect on learning outcomes. As our focus is on CRM/teamwork, only data on the effect of the escape room on teamwork were extracted and data on, for example, knowledge or skills was not extracted. The level of the evaluation on the effect on CRM/teamwork was determined using Reeves’ [ 30 ] IPE expanded typology of Kirkpatrick’s [ 31 ] classic model of the levels of learning outcomes: reaction (level 1); modification of attitudes/perceptions (level 2a); acquisition of knowledge/skills (level 2b); behavioral change (level 3); outcome on a patient or organizational level (level 4).
To appraise the methodological quality of the teamwork evaluation, Medical Education Research Study Quality Instrument (MERSQI) scores were calculated [ 32 ]. As this was used to qualitatively assess the strength of the link between design characteristics and their effect, MERSQI scores were not calculated for the whole study, but only for the assessment of the effect on CRM/teamwork. The MERSQI [ 32 ] is considered a useful and reliable tool for appraising the methodological quality of medical education research with good interrater reliability [ 33 ]. The MERSQI has 6 domains (10 items) from study design to study outcome. Each domain has a maximum of 3 points that can be scored, and totals range from 5 up to 18 points. The 6 domains allow interpretation to focus on normative domain-specific scores, rather than on overall scores [ 33 ] and to better identify specific gaps in methodology. To maximize the available data, all studies were included in the analysis of effect and no cut-off scores were used to exclude studies based on their MERSQI score. The MERSQI scores were calculated by the first author (GJ). Additionally, three authors (JL, SB and WK) independently calculated a MERSQI score for 1 of the studies to check scoring quality and consistency. In case of doubt on the scoring in the other studies, this was solved by discussion in the full team of authors.
An Excel (Microsoft ® Excel ® for Microsoft 365 MSO, Redmond, Washington, U.S) data charting form was developed for data extraction and calculating MERSQI scores. The form was evaluated for consistency and completeness by extracting data from 3 included articles by 1 author (GJ), with double-checking by all other authors. After final amendments, 1 author (GJ) extracted the data.
Synthesis of results
The three previously mentioned categories (study characteristics - educational and escape room design characteristics – effect on learning) were used as headings to summarize data. Data from studies in the virtual, student and setting group were included in the analyses and synthesis of the data was used to answer the research questions.
Selection of sources of evidence
In Fig. 1 a PRISMA flowchart [ 19 ] depicts the search results and screening process. Fourteen studies were included in the analysis, of which four were included in the ‘student’ group and two in the ‘virtual’, group. No studies were found for the ‘settings’ group. Of the fourteen studies, twelve described the design of an escape room. While the other two studies (both in the ‘student’ group) were evaluation studies of one of the escape rooms in the ‘student’ group.

PRISMA flowchart of screening process [ 19 ]. *before the full text screening studies were divided into the different strands. If during full-text screening a study better fitted into one of the other strands, the study was transferred there
Qualitative Synthesis
The full data extraction form, including all extracted data can be found in the Additional file 2 . The overall characteristics of the included studies are presented in Table 1 . The two studies that only evaluated the effect of the escape room are displayed in relation with the study describing the escape room design (ID 10 A-B [ 34 , 35 ]). In the 11 studies that evaluated the escape room, 419 participants were included (mean 45). In 50% of the studies ( n = 6/12) the escape room was aimed at teamwork in Emergency Medicine. Aims of both the studies and the escape rooms differed significantly. Excluding both evaluation studies, two-third of the studies ( n = 8/12) primarily described design [ 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ], while the others [ 44 , 45 , 46 , 47 ] had evaluation as their primary aim. Teamwork was not the sole aim of all escape rooms, as eight studies also aimed at knowledge and/or skills. This heterogeneity complicated the extraction of design criteria, their underpinning and relating them to their effect on CRM/teamwork.
Educational and escape room design characteristics
The underlying pedagogical or didactical principles and/or learning theories were only noted in four of the twelve studies. Specifically, Kutzin [ 38 ] provided an elaborate underpinning using interdisciplinary game theory for the development of his physical escape room aimed at teamwork. Rosenkrantz [ 39 ] Sanders [ 40 ] and Kutzin (virtual) [ 42 ] gave a short explanation for using the concept of edutainment in the development of their escape rooms. Four studies provided a theoretical CRM/teamwork framework with which the escape room was developed. Kutzin [ 38 ], Sanders [ 40 ] and Kutzin (virtual) [ 42 ] used the TeamSTEPPS framework and Rosenkrantz used the ‘Anesthesiologists Non-Technical Skills in Denmark (ANTSdk)’. Of the other eight studies, Turner [ 43 ] and Daniel [ 47 ] mentioned a number of non-technical skills like task-switching, leadership and shared mental model as a learning goal. The escape room learning goal of improving communication and/or teamwork was not further specified in all other studies.
Table 2 shows the summarized data that was extracted on escape room design. Full data on all studies can be found in Additional file 2 . Teams were given median 38 min (range 15–60) to escape. Teams ranged from 5 to 10 participants, with 4–6 being the most common team size (50%; n = 6/12); in three (25%) studies team size was not mentioned [ 36 , 37 , 40 ].
It is noteworthy that data on the alignment of the escape room with the teamwork learning objectives could only be extracted from five studies, with only Turner [ 43 ] providing specifics on each teamwork item. Alignment with skills and knowledge training was either explicitly stated and/or could be inferred from the puzzle theme or description (data not included). However, how the need for teamwork was ensured or facilitated was often not mentioned, other than that escape rooms were collaborative by nature.
With regard to the organization of the puzzles, the linear path (also called sequential) was most common ( n = 7/12), with 1 study combining the open and linear path [ 40 ].
Seven of the twelve studies noted a structured debriefing with the use of guidelines and known debriefing tools. Two studies did not mention whether debriefing was used and one study specifically mentions there was no debriefing. The two remaining studies mentioned a short debrief mainly aimed at the answers to the puzzles.
For interprofessional education we extracted data on the interdependence and embodiment (immersion). Interdependence was not specifically mentioned in the included studies. However, in four studies data were found that indicated some degree of interdependence. Sanders [ 40 ] mentioned presenting multiple puzzles at once, so different team members could be engaged and work simultaneously on different puzzles. Additionally, the team was led to certain points where they had to work together as a full team. The virtual escape room by Kutzin (virtual) [ 42 ] had several puzzles that ‘required participants to work on different screens with a need to communicate’. Additionally in the escape rooms developed by Podlog [ 44 ] and Gomez-Urquiza [ 46 ], the puzzle scheme allowed for participants to work on several puzzles simultaneously.
Details on immersion could be extracted from five studies and was often accomplished by using attributes and props that were also found in daily practice, and/or that were related to the escape room theme. Additionally darkening of the room was used by Rosenkrantz [ 39 ] and Sanders [ 40 ]. Sanders [ 40 ] and Abensur Vuillaume [ 36 ] mentioned using their escape room introduction to set the theme.
Escape rooms can be used as stand-alone activities, but are also often integrated into a course, curriculum, or used in combination with other teaching modalities. Three studies used the escape room as a stand-alone activity [ 37 , 39 , 46 ], two studies did not mention other teaching modalities [ 36 , 42 ], while the others used one or more other teaching modalities. Sanders, for example, used the escape room as part of an annual competition among pediatric Emergency Medicine faculty and fellows [ 40 ], while Kutzin [ 38 ] and Holland [ 45 ] used the escape room as part of an obligatory course. Morrell used a broad range of other teaching modalities: lectures, activities, case studies, videos, assigned readings, and simulation [ 41 ]. The escape room by Daniel had ALS simulations before and after the escape room [ 47 ]. Both Podlog [ 44 ] and Turner [ 43 ] tried to increase knowledge retention by giving a didactic summary and lecture respectively.
Effect on learning
Effectiveness was investigated in 13 studies. The data from Rosenkrantz [ 39 ] was split into acute care personnel and students as different methods were used to study the effect of their escape room in these 2 groups. See Table 1 for the measures used per study. Most studies ( n = 10) studied reaction (level 1) to the escape room using surveys ( n = 9), or informal feedback ( n = 1). Specific phrasing and number of questions differed, with 3 out of 9 survey studies not providing the specific questions [ 37 , 42 , 44 ]. In general participants were asked whether they enjoyed the escape room and thought it was effective in training teamwork.
Holland [ 45 ], besides using a survey, and both studies by Morrell [ 34 , 35 ] used focus group analysis to study modification of attitudes/perceptions (level 2a). Rosenkrantz [ 39 ], besides using a survey, rated videos of the fastest and slowest student group on the use of non-technical skills, which constituted studying acquisition of knowledge/skills (level 2b).
All the included studies showed a positive effect on teamwork of the escape room on the levels of effect they scored on. In the ten studies scoring Kirkpatrick level 1 > 80% of participants scored positive on enjoyment and engagement. Participants also generally felt that teamwork was trained by the escape room with mean Likert scores > 80% of the maximum, and teamwork and communication were often mentioned in response to open-ended questions directed at what participants felt they had learned. In the analysis on learning outcomes from focus groups (Kirkpatrick level 2a), teamwork also emerged as a theme in all 3 studies. Rosenkrantz [ 39 ] noted in the assessment of videos of students (Kirkpatrick level 2b) that time to finish the escape room was not related to whether there was a team leader. Video observers in the same study rated gathering information, exchanging information and reassessing decisions as the most used non-technical skills.
Additional file 3 shows the MERSQI scores of all the included studies. The median MERSQI score is 7.0 (range 6.0–12.0), which is lower than the mean of 9.6 in the original paper where MERSQI was first described [ 32 ]. Notably ‘validity evidence for evaluation instrument scores’ were rather low, with only 5 studies scoring 1.0 out of 3.0 points. This relates to the fact that researchers mostly used surveys that were developed for their study.
In this scoping review of fourteen studies addressing the design and effect of escape rooms used for training CRM/teamwork for healthcare professionals in acute care, we identified several commonly used design requirements, but noticed a lack of reporting on alignment and insufficient data to connect design requirements to learning outcomes. Below, these results are discussed per research question.
Design characteristics
Common design characteristics were derived from the whole group of included studies, given the small number of studies. Team size (4–6 participants) was in line with commonly used team sizes in healthcare and other fields [ 12 , 17 ]. The time limit of about 40 min was slightly shorter compared to the 60 min found in earlier reviews on escape rooms [ 12 , 17 ]. We found Puzzle organization most often to be linear, though complex and open puzzle organization were explicitly used to evoke teamwork. Some form of briefing and use of a facilitators (inside or outside the escape room) to moderate progress and provide hints were also used in all studies. Debriefing was often structured, coupling teamwork factors to what happened during the escape room and often relating this to the clinical situation. This suggests that debriefing was used to critically reflect on CRM/teamwork and promote learning. This parallels to simulation, where debriefing is considered a key factor in learning [ 48 ].
Little information was given on the alignment of the escape room with the teamwork learning goals. This may be due to the study types, which commonly focused on the effect of the escape room, instead of on how design moderated or optimized teamwork learning outcomes. However, even in those studies focused on design [ 36 , 39 , 40 , 41 ], little was reported on how design characteristics were used to achieve the desired teamwork learning outcomes. This was also reflected in the other data-items which were often not reported or could only be extracted indirectly.
Design characteristics and learning outcomes: deriving design requirements
In an attempt to connect design characteristics to their effect on learning outcomes, we reviewed the outcome measures and effect of the included escape rooms. These outcomes reflected the potential escape rooms yield for teamwork training, as reactions (level 1) to the escape room were overtly positive in all studies. This was further strengthened by the effects, be it in small numbers, seen on modification of attitudes/perceptions (level 2a) and studying acquisition of knowledge/skills (level 2b). However, looking at the quality of this evidence, there is no evidence on higher Kirkpatrick levels and study sizes are rather small. Additionally MERSQI scores on determining CRM/teamwork learning outcomes were rather low (median 7.0; mean 7.8), compared to for example the 9.6 mean in the original paper where MERSQI was first described [ 32 ]. Within the MERSQI the low ‘validity evidence for evaluation instrument scores’ further underscores the lack of valid effect measures. Combined with the considerable study heterogeneity, this precluded any conclusions on the effect design characteristics had on learning outcomes and the deriving of design requirements.
Gaps and looking forward
From our results we see 2 main gaps in the design of escape rooms aimed at CRM/teamwork in acute care professionals: (i) a lack of data on the effect of design requirements on learning outcome and (ii) a lack of (reporting on) alignment between learning goals and design of these escape rooms.
Escape rooms are collaborative by nature, with teams communicating and working on puzzles together. This suggests teamwork and attests to the potential escape rooms have. The overtly positive effects that were seen in the included studies confirmed this, and is in line with data from reviews covering a broad range of educational fields [ 17 , 24 ], including healthcare students [ 12 ]. In acute care this positive effect was also seen in two studies on the effect of a commercial escape room on teamwork [ 49 , 50 ]. Especially Valdes et al. [ 49 ], who showed that key CRM aspects improved in acute care simulation after participation in an escape room, attest to the potential escape rooms have for CRM/teamwork in acute care. However, which design characteristics maximize this potential remains unknown. None of the studies described or examined which characteristics were key in reaching the desired learning outcomes. As an example, we found the linear puzzle organization (in which one puzzle leads to the other) to be the most common. In their systematic review Veldkamp et al. [ 17 ], however stated that team-based medical escape rooms do not align well with a linear puzzle organization and suggested using other organizations. Whether different puzzle organizations really lead to higher learning outcomes, is debatable as they have not been compared directly. However, we do agree with their conclusion that studying the effect of different design characteristics on learning outcomes is necessary to maximize learning outcomes. A first step is systematic reporting on these design characteristics in all studies using escape rooms to train CRM/teamwork learning in healthcare. Reporting the data items we extracted, which are in line with a range of escape room development frameworks [ 14 , 15 , 16 ], would be a good way to start. Future research should not only focus on the effect escape rooms have, but also on the mechanisms by which this effect is reached, comparing different design characteristics and extracting which are pivotal and therefore should be considered as design requirements. By identifying these requirements, an evidence-based foundation can be laid for developing and executing these escape rooms.
The need for effective design requirements relates to the other major gap we identified: the need for better (reporting on) alignment between learning goals and escape room design. As is also acknowledged by others [ 16 , 51 ], we agree that better alignment should be sought, investigated and reported [ 17 ]. Cohen et al. [ 16 ] provide design considerations for escape rooms aimed at teamwork and advice using the Input-Moderator-Output-Input model by Ilgen [ 52 ] to identify and measure a variety of factors that best predict team outcomes and others advocate the use of Educational Design Research (EDR) [ 53 ]. Both could be used to initiate iterative cycles of individual puzzle or complete escape room development, leading not only to better reporting of alignment, but also to more effective design and the development of design requirements.
Strengths and limitations
Educational escape rooms are a relatively young and growing field. The fact that this field is young, translated into a limitation for our review. Only a relatively small number of studies with modest population size and limited methodological quality fitted our criteria. We therefore included studies on virtual acute care escape rooms and acute care escape rooms in students, which allowed us to enrich this dataset. By clearly marking these groups, it is easily deducible where the data came from.
Less than half of the studies had description of design as their primary aim, limiting the data that could be extracted. However, looking from an educational perspective, this review offers an excellent new starting point in the iterative cycle of development. A final limitation is that the search was conducted in June 2023 and research published since is not included.
Despite the above limitations, to our knowledge, the present study is the first to provide a comprehensive analysis of escape room design aimed at enhancing CRM/teamwork in acute care professionals.
In conclusion we found that escape rooms that aim at improving CRM/teamwork in acute care professionals often have 4–6 participants, a 40-minute time limit, linear puzzle organization, use briefing and a structured debriefing is considered important for learning. Reporting on alignment of CRM/teamwork learning goals and escape room design is insufficient and there is insufficient evidence on how and whether design characteristics optimize learning outcomes. There is a need for more complete reporting of future escape rooms aimed at training teamwork in acute care professionals and research on maximizing the learning potential of these escape rooms through design.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files (additional file 2).
Abbreviations
Advanced Life Support
Basic Life Support
Cardio-Pulmonary Resuscitation
Crew Resource Management
Electrocardiogram
Educational Design Research
Emergency Medicine
EMS Emergency Medical Services
Escape Room
Family Medicine
Intensive Care Unit
Medical Education Research Study Quality Instrument
Medical Students.
Nursing Students
- Non-technical skills
Operating Room
Promoting Excellence and Reflective Learning in Simulation
Postpartum Hemorrhage
Buljac-Samardzic M, Doekhie KD, van Wijngaarden JDH. Interventions to improve team effectiveness within health care: a systematic review of the past decade. Hum Resour Health. 2020;18(1).
Hughes AM, Gregory ME, Joseph DL, Sonesh SC, Marlow SL, Lacerenza CN, et al. Saving lives: a meta-analysis of team training in healthcare. J Appl Psychol. 2016;101(9):1266–304.
Article Google Scholar
Buljac-Samardzic M, Dekker-van Doorn CM, Maynard MT. What do we really know about Crew Resource Management in Healthcare? An Umbrella Review on Crew Resource Management and its effectiveness. J Patient Saf. 2021;17(8):e929–58.
Gross B, Rusin L, Kiesewetter J, Zottmann JM, Fischer MR, Pruckner S, Zech A. Crew resource management training in healthcare: a systematic review of intervention design, training conditions and evaluation. Bmj Open. 2019;9(2):e025247.
O’Dea A, O’Connor P, Keogh I. A meta-analysis of the effectiveness of crew resource management training in acute care domains (90, pg 698, 2014). Postgrad Med J. 2014;90(1070):708.
Google Scholar
O’Connor P, Campbell J, Newon J, Melton J, Salas E, Wilson KA. Crew Resource Management Training effectiveness: a Meta-analysis and some critical needs. Int J Aviat Psychol. 2008;18(4):353–68.
Haerkens MH, Kox M, Lemson J, Houterman S, van der Hoeven JG, Pickkers P. Crew Resource Management in the Intensive Care Unit: a prospective 3-year cohort study. Acta Anaesthesiol Scand. 2015;59(10):1319–29.
Cook DA, Brydges R, Hamstra SJ, Zendejas B, Szostek JH, Wang AT, et al. Comparative effectiveness of technology-enhanced simulation versus other instructional methods: a systematic review and meta-analysis. Simul Healthc. 2012;7(5):308–20.
Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9):978–88.
Fung L, Boet S, Bould MD, Qosa H, Perrier L, Tricco A, et al. Impact of crisis resource management simulation-based training for interprofessional and interdisciplinary teams: a systematic review. J Interprof Care. 2015;29(5):433–44.
Nicholson S. Peeking behind the locked door: A survey of escape room facilities. 2015.
Quek LH, Tan AJQ, Sim MJJ, Ignacio J, Harder N, Lamb A, et al. Educational escape rooms for healthcare students: a systematic review. Nurse Educ Today. 2023;132:106004.
Lathwesen C, Belova N. Escape rooms in STEM teaching and learning-prospective field or declining Trend? A literature review. Educ Sci. 2021;11(6).
Dittman JM, Amendola MF, Ramraj R, Haynes S, Lange P. The COMET framework: a novel approach to design an escape room workshop for interprofessional objectives. J Interprof Care. 2022;36(1):161–4.
Doherty SM, Griggs AC, Lazzara EH, Keebler JR, Gewertz BL, Cohen TN. Planning an escape: considerations for the development of Applied escape rooms. Simulation & Gaming; 2023.
Cohen TN, Griggs AC, Keebler JR, Lazzara EH, Doherty SM, Kanji FF, Gewertz BL. Using escape rooms for conducting Team Research: understanding Development, considerations, and challenges. Simul Gaming. 2020;51(4):443–60.
Veldkamp A, van de Grint L, Knippels M, van Joolingen WR. Escape education: a systematic review on escape rooms in education. Educ Res Rev-Neth. 2020;31:17.
McGowan J, Straus S, Moher D, Langlois EV, O’Brien KK, Horsley T, et al. Reporting scoping reviews-PRISMA ScR extension. J Clin Epidemiol. 2020;123:177–9.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Elicit. [Available from: https://elicit.com/.
Google S. [ https://scholar.google.com/ .
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev-London. 2016;5.
Clarke S, Peel DJ, Arnab S, Morini L, Keegan H, Wood O. escapED: a Framework for creating Educational escape rooms and interactive games for Higher/Further education. Int J Serious Games. 2017;4(3):73–86.
Fotaris P, Mastoras T. Escape rooms for learning: a systematic review. Proc Eur Conf Game. 2019:235–43.
Veldkamp A, van de Grint L, Knippels MCPJ, van Joolingen WR. Escape education: a systematic review on escape rooms in education. Educ Res Rev-Neth. 2020;31.
Veldkamp A, Daemen J, Teekens S, Koelewijn S, Knippels MCPJ, van Joolingen WR. Escape boxes: bringing escape room experience into the classroom. Brit J Educ Technol. 2020;51(4):1220–39.
Comm IS. INACSL standards of best practice: Simulation(SM) Simulation Design. Clin Simul Nurs. 2016;12:S5–12.
Comm IS. INACSL standards of best practice: Simulation(SM) Simulation-enhanced Interprofessional Education (Sim-IPE). Clin Simul Nurs. 2016;12:S34–8.
Maddock B, Darzins P, Kent F. Realist review of interprofessional education for health care students: what works for whom and why. J Interprof Care. 2022.
Reeves S, Boet S, Zierler B, Kitto S. Interprofessional Education and Practice Guide 3: evaluating interprofessional education. J Interprof Care. 2015;29(4):305–12.
Kirkpatrick DL, Kirkpatrick J. Evaluating training programs: the four levels. Berrett. Berkley, USA: Koehler; 1998.
Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM. Association between funding and quality of published medical education research. JAMA. 2007;298(9):1002–9.
Cook DA, Reed DA. Appraising the quality of medical education research methods: the Medical Education Research Study Quality Instrument and the Newcastle-Ottawa Scale-Education. Acad Med. 2015;90(8):1067–76.
Morrell BLM, Eukel HN. Escape the generational gap: a Cardiovascular escape room for nursing education. J Nurs Educ. 2020;59(2):111–5.
Morrell BLM, Eukel HN, Santurri LE. Soft skills and implications for future professional practice: qualitative findings of a nursing education escape room. Nurse Educ Today. 2020;93.
Abensur Vuillaume L, Laudren G, Bosio A, Thévenot P, Pelaccia T, Chauvin A. A didactic escape game for Emergency Medicine aimed at learning to work as a team and making diagnoses: methodology for Game Development. JMIR Serious Games. 2021;9(3):e27291.
Borck JC, Meyer DDNPCAA, Gettrust LDNPA-BC, Novalija JC. Escape the OR: a novel teaching strategy to promote interprofessional learning and teamwork. Nurs Manag. 2022;53(2):28–35.
Kutzin JM. Escape the room: innovative approaches to Interprofessional Education. J Nurs Educ. 2019;58(8):474–80.
Rosenkrantz O, Jensen TW, Sarmasoglu S, Madsen S, Eberhard K, Ersboll AK, Dieckmann P. Priming healthcare students on the importance of non-technical skills in healthcare: how to setup a medical escape room game experience. Med Teach. 2019;41(11):1285–92.
Sanders JE, Kutzin J, Strother CG. Escape the Simulation Room. Simul Gaming. 2021;52(1):62–71.
Morrell B, Eukel HN. Shocking escape: a cardiac escape room for undergraduate nursing students. Simul Gaming. 2021;52(1):72–8.
Kutzin JM, Sanders JE, Strother CG. Transitioning escape rooms to a virtual environment. Simul Gaming. 2021;52(6):796–806.
Turner A, Tichter AM, Pillow MT. Let’s escape Didactics: virtual escape room as a didactic modality in Residency. J Educ Teach Emerg Med. 2021;6(2):Sg46–56.
Podlog M, Husain A, Greenstein J, Sanghvi S. Escape the trauma room. AEM Educ Train. 2020;4(2):158–60.
Holland T, Kuhnly JE, McKelvey M, Prast J, Walter L. Evaluation of a Postpartum Hemorrhage escape room: a Multisite Study. Simul Gaming. 2023:24.
Gomez-Urquiza JL, Requena-Palomares I, Gorjon-Peramato E, Gomez-Salgado J, Canadas-De La Fuente GA, Albendin-Garcia L. Emergency and critical care professionals’ opinion on escape room as a health sciences evaluation game: A cross-sectional descriptive study. Med (United States). 2022;101(25) (no pagination).
Daniel L, Valko J, McAtee TJ. Using an escape room modality to teach mock code essentials. J Contin Educ Nurs. 2021;52(3):118–22.
Cheng A, Eppich W, Grant V, Sherbino J, Zendejas B, Cook DA. Debriefing for technology-enhanced simulation: a systematic review and meta-analysis. Med Educ. 2014;48(7):657–66.
Valdes B, Mckay M, Sanko JS. The impact of an escape Room Simulation to improve nursing teamwork, Leadership and Communication skills: a Pilot Project. Simul Gaming. 2021;52(1):54–61.
Zhang XC, Lee H, Rodriguez C, Rudner J, Chan TM, Papanagnou D. Trapped as a Group, escape as a team: applying gamification to Incorporate Team-building skills through an ‘Escape room’ experience. Cureus. 2018;10(3):9.
Fotaris P, Mastoras T. Room2Educ8: a Framework for creating Educational escape rooms based on design thinking principles. Educ Sci. 2022;12(11).
Ilgen DR, Hollenbeck JR, Johnson M, Jundt D. Teams in organizations: from input-process-output models to IMOI models. Annu Rev Psychol. 2005;56:517–43.
Chen WC, Reeves TC. Twelve tips for conducting educational design research in medical education. Med Teach. 2020;42(9):980–6.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Human Factors and Cognitive Ergonomics, Research Coordinator Human Factors-CODE team DSI institute & Faculty Behavioral, Management and Social Sciences (BMS), Data and Education (CODE) Group, University of Twente, Drienerlolaan 5, Cognition, Enschede, NB, 7522, The Netherlands
Simone Borsci
Department of Surgery and Cancer, NIHR London IVD, Imperial College of London, London, UK
Department of Intensive Care, Radboud University Medical Center, Geert Groote Plein Zuid 10, Nijmegen, 6525GA, The Netherlands
Gerald J. Jaspers, Johannes G. van der Hoeven & Joris Lemson
Research on Learning and Education, Radboudumc Health Academy, Radboud University Medical Center, Geert Groote Plein Zuid 10, Nijmegen, 6525GA, The Netherlands
Wietske Kuijer-Siebelink
School of Education, HAN University of Applied Sciences, Nijmegen, The Netherlands
You can also search for this author in PubMed Google Scholar
Contributions
G.J. designed the study-protocol, drafted the search, screened studies, extracted data and drafted the manuscript. S.B. and J.L. revised the study-protocol, checked screening of studies and data extraction and revised the manuscript. H.H. revised the manuscript. W.K. revised the study-protocol, checked data extraction and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Gerald J. Jaspers .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12909_2024_5753_MOESM1_ESM.docx
Supplementary Material 1: Selection of databases and search strategy. Additional information on the selection of databases, the used additional resources and the full search strings for all databases.
12909_2024_5753_MOESM2_ESM.xlsx
Supplementary Material 2: Data extraction form. The full data extraction form (Table 1), including all data and data-items that were extracted (data-items are headings of the different columns). Calculated MERSQI score (Table 2).
12909_2024_5753_MOESM3_ESM.docx
Supplementary Material 3: Table with MERSQI scores. A Table with the full MERSQI scores, including scores on all separate items.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jaspers, G., Borsci, S., van der Hoeven, J. et al. Escape room design in training crew resource management in acute care: a scoping review. BMC Med Educ 24 , 819 (2024). https://doi.org/10.1186/s12909-024-05753-z
Download citation
Received : 29 January 2024
Accepted : 08 July 2024
Published : 30 July 2024
DOI : https://doi.org/10.1186/s12909-024-05753-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Crisis resource management
- Escape game
- Puzzle room
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays).
Examples of literature reviews. Step 1 - Search for relevant literature. Step 2 - Evaluate and select sources. Step 3 - Identify themes, debates, and gaps. Step 4 - Outline your literature review's structure. Step 5 - Write your literature review.
What are the goals of creating a Literature Review? A literature could be written to accomplish different aims: To develop a theory or evaluate an existing theory; To summarize the historical or existing state of a research topic; Identify a problem in a field of research ; Baumeister, R. F., & Leary, M. R. (1997). Writing narrative literature ...
A literature review is a critical analysis and synthesis of existing research on a particular topic. It provides an overview of the current state of knowledge, identifies gaps, and highlights key findings in the literature. 1 The purpose of a literature review is to situate your own research within the context of existing scholarship, demonstrating your understanding of the topic and showing ...
What are the goals of summaries? • To understand the historical context and current state of the literature • To begin to identify themes, trends, patterns ... When a literature review emphasizes explanation of what you believe the knowledge stemming from previous literature means (formative evaluation) it compares and contrasts the various ...
The purpose of a literature review. The four main objectives of a literature review are:. Studying the references of your research area; Summarizing the main arguments; Identifying current gaps, stances, and issues; Presenting all of the above in a text; Ultimately, the main goal of a literature review is to provide the researcher with sufficient knowledge about the topic in question so that ...
A literature review may consist of simply a summary of key sources, but in the social sciences, a literature review usually has an organizational pattern and combines both summary and synthesis, often within specific conceptual categories.A summary is a recap of the important information of the source, but a synthesis is a re-organization, or a reshuffling, of that information in a way that ...
Goals of a Literature Review. provide an overview of the scholarly literature on a chosen topic including the major theories, issues, works, and debates in the field; synthesize all this information into an organized summary; critique current knowledge of a topic; identify aspects of the topic that need further investigation
Mapping the gap. The purpose of the literature review section of a manuscript is not to report what is known about your topic. The purpose is to identify what remains unknown—what academic writing scholar Janet Giltrow has called the 'knowledge deficit'—thus establishing the need for your research study [].In an earlier Writer's Craft instalment, the Problem-Gap-Hook heuristic was ...
What are the goals of creating a Literature Review? To develop a theory or evaluate an existing theory; To summarize the historical or existing state of a research topic; Identify a problem in a field of research - Baumeister, R.F. & Leary, M.R. (1997). "Writing narrative literature reviews," Review of General Psychology, 1(3), 311-320.
A formal literature review is an evidence-based, in-depth analysis of a subject. There are many reasons for writing one and these will influence the length and style of your review, but in essence a literature review is a critical appraisal of the current collective knowledge on a subject. Rather than just being an exhaustive list of all that ...
These sections serve to establish a scholarly basis for the research or discussion within the paper. In a standard 8000-word journal article, the literature review section typically spans between 750 and 1250 words. The first few sentences or the first paragraph within this section often serve as an introduction.
A literature review is an integrated analysis-- not just a summary-- of scholarly writings and other relevant evidence related directly to your research question.That is, it represents a synthesis of the evidence that provides background information on your topic and shows a association between the evidence and your research question.
Most literature reviews are embedded in articles, books, and dissertations. In most research articles, there are set as a specific section, usually titled, "literature review", so they are hard to miss.But, sometimes, they are part of the narrative of the introduction of a book or article. This section is easily recognized since the author is engaging with other academics and experts by ...
As mentioned previously, there are a number of existing guidelines for literature reviews. Depending on the methodology needed to achieve the purpose of the review, all types can be helpful and appropriate to reach a specific goal (for examples, please see Table 1).These approaches can be qualitative, quantitative, or have a mixed design depending on the phase of the review.
2. MOTIVATE YOUR RESEARCH in addition to providing useful information about your topic, your literature review must tell a story about how your project relates to existing literature. popular literature review narratives include: ¡ plugging a gap / filling a hole within an incomplete literature ¡ building a bridge between two "siloed" literatures, putting literatures "in conversation"
Literature reviews establish the foundation of academic inquires. However, in the planning field, we lack rigorous systematic reviews. In this article, through a systematic search on the methodology of literature review, we categorize a typology of literature reviews, discuss steps in conducting a systematic literature review, and provide suggestions on how to enhance rigor in literature ...
Here is a step-by-step approach to drafting your literature review: Define Your Goal If you are writing an argument paper, create a thesis statement with a clear position. If you are evaluating scientific theories, develop a hypothesis to examine. If you are providing a self-contained review of writings on a topic, state your project's purpose.
A literature or narrative review is a comprehensive review and analysis of the published literature on a specific topic or research question. The literature that is reviewed contains: books, articles, academic articles, conference proceedings, association papers, and dissertations. It contains the most pertinent studies and points to important ...
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question. It is often written as part of a thesis, dissertation, or research paper, in order to situate your work in relation to existing knowledge.
The literature review is a vital part of medical education research and should occur throughout the research process to help researchers design a strong study and effectively communicate study results and importance. To achieve these goals, researchers are advised to plan and execute the literature review carefully.
Keeping these goals in mind throughout your project will help you stay organized and focused. A literature review helps the author: Understand the scope, history, and present state of knowledge in a specific topic; Understand application of research concepts such as statistical tests and methodological choices
Immunization directly impacts health (SDG3) and brings a contribution to 14 out of the 17 Sustainable Development Goals (SDGs), such as ending poverty, reducing hunger, and reducing inequalities. Therefore, immunization is recognized to play a central role in reaching the SDGs, especially in low- and middle-income countries (LMICs). Despite continuous interventions to strengthen immunization ...
We employed a Systematic Literature Review as our chosen research methodology to achieve this goal. The selection of a systematic literature review is underpinned by its distinctive ability to provide a replicable, transparent, and reliable assessment of the existing body of knowledge on a specific subject, as advocated by Janssen and Sauer .
Book Review: Linguistics and English Literature: An Introduction (Cambridge Introductions to the English Language) Urszula Kizelbach View all authors and affiliations Based on : Adamson H. D., Linguistics and English Literature: An Introduction (Cambridge Introductions to the English Language) , Cambridge: Cambridge University Press, 2019 ...
Compared to other malignancies, few studies have investigated the role of family history of cancer (FHC) in patients with lung cancer, yielding largely heterogeneous results. We performed a systematic literature review in accordance with PRISMA guidelines, searching the PubMed and Scopus databases from their inception to November 25, 2023, to identify studies reporting on the role of FHC in ...
Digital transformation has emerged as a significant driver of innovation globally, with Gulf Cooperation Council (GCC) nations actively participating in this evolution. This systematic review provides a comprehensive assessment of the digital transformation in the GCC's oil and gas sector over the past decade. Through a rigorous bibliometric analysis of 505 documents sourced from the SCOPUS ...
This review article explores the scientific literature on managing neurodiversity in workplaces, aiming to identify emerging research directions, gaps, and methods used. A systematic literature review in the hybrid form was implemented, combining bibliometric analysis and structured review. A review of selected social sciences publications from the SCOPUS database was conducted.
In 2023, we conducted a scoping review to collect and synthesize evidence from a broad spectrum of studies addressing the COVID-19 pandemic. A scoping review allows for the assessment of literature's volume, nature, and comprehensiveness, and is uniquely inclusive of both peer-reviewed articles and gray literature—such as reports, white papers, and policy documents.
To achieve these goals, we performed a scoping review of the literature regarding design characteristics and their effect on learning outcomes in escape rooms used for crew resource management and/or teamwork training for healthcare professionals in acute care settings. ... A literature review. Educ Sci. 2021;11(6). Dittman JM, Amendola MF ...