Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General [Internet]. Atlanta (GA): Centers for Disease Control and Prevention (US); 2016.


E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General [Internet].
Chapter 1 introduction, conclusions, and historical background relative to e-cigarettes.
- Introduction
Although conventional cigarette smoking has declined markedly over the past several decades among youth and young adults in the United States ( U.S. Department of Health and Human Services [USDHHS] 2012 ), there have been substantial increases in the use of emerging tobacco products among these populations in recent years ( Centers for Disease Control and Prevention [CDC] 2015c ). Among these increases has been a dramatic rise in electronic cigarette (e-cigarette) use among youth and young adults. It is crucial that the progress made in reducing cigarette smoking among youth and young adults not be compromised by the initiation and use of e-cigarettes. This Surgeon General’s report focuses on the history, epidemiology, and health effects of e-cigarette use among youth and young adults; the companies involved with marketing and promoting these products; and existing and proposed public health policies regarding the use of these products by youth and young adults.
E-cigarettes include a diverse group of devices that allow users to inhale an aerosol, which typically contains nicotine, flavorings, and other additives. E-cigarettes vary widely in design and appearance, but generally operate in a similar manner and are composed of similar components ( Figure 1.1 ). A key challenge for surveillance of the products and understanding their patterns of use is the diverse and nonstandard nomenclature for the devices ( Alexander et al. 2016 ). These devices are referred to, by the companies themselves, and by consumers, as “e-cigarettes,” “e-cigs,” “cigalikes,” “e-hookahs,” “mods,” “vape pens,” “vapes,” and “tank systems.” In this report, the term “e-cigarette” is used to represent all of the various products in this rapidly diversifying product category. The terms may differ by geographic region or simply by the prevailing preferences among young users. For example, some refer to all cigarette-shaped products as “e-cigarettes” or as “cigalikes,” and some may refer to the pen-style e-cigarettes as “hookah pens” or “vape pens” ( Richtel 2014 ; Lempert et al. 2016 ).
Diversity of e-cigarette products. Source: Photo by Mandie Mills, CDC.
This report focuses on research conducted among youth and young adults because of the implications of e-cigarette use in this population, particularly the potential for future public health problems. Understanding e-cigarette use among young persons is critical because previous research suggests that about 9 in 10 adult smokers first try conventional cigarettes during adolescence ( USDHHS 2012 ). Similarly, youth e-cigarette experimentation and use could also extend into adulthood; however, e-cigarette use in this population has not been examined in previous reports of the Surgeon General. The first Surgeon General’s report on the health consequences of smoking was published in 1964; of the subsequent reports, those published in 1994 and 2012 focused solely on youth and young adults ( USDHHS 1994 , 2012 ). More recently, the 2012 report documented the evidence regarding tobacco use among youth and young adults, concluding that declines in cigarette smoking had slowed and that decreases in the use of smokeless tobacco had stalled. That report also found that the tobacco industry’s advertising and promotional activities are causal to the onset of smoking in youth and young adults and the continuation of such use as adults ( USDHHS 2012 ). However, the 2012 report was prepared before e-cigarettes were as widely promoted and used in the United States as they are now. Therefore, this 2016 report documents the scientific literature on these new products and their marketing, within the context of youth and young adults. This report also looks to the future by examining the potential impact of e-cigarette use among youth and young adults, while also summarizing the research on current use, health consequences, and marketing as it applies to youth and young adults.
Evidence for this report was gathered from studies that included one or more of three age groups. We defined these age groups to be young adolescents (11–13 years of age), adolescents (14–17 years of age), and young adults (18–24 years of age). Some studies refer to the younger groups more generally as youth. Despite important issues related to e-cigarette use in adult populations, clinical and otherwise (e. g ., their potential for use in conventional smoking cessation), that literature will generally not be included in this report unless it also discusses youth and young adults ( Farsalinos and Polosa 2014 ; Franck et al. 2014 ; Grana et al. 2014 ).
Given the recency of the research that pertains to e-cigarettes, compared with the decades of research on cigarette smoking, the “precautionary principle” is used to guide actions to address e-cigarette use among youth and young adults. This principle supports intervention to avoid possible health risks when the potential risks remain uncertain and have been as yet partially undefined ( Bialous and Sarma 2014 ; Saitta et al. 2014 ; Hagopian et al. 2015 ). Still, the report underscores and draws its conclusions from the known health risks of e-cigarette use in this age group.
Organization of the Report
This chapter presents a brief introduction to this report and includes its major conclusions followed by the conclusions of the chapters, the historical background of e-cigarettes, descriptions of the products, a review of the marketing and promotional activities of e-cigarette companies, and the current status of regulations from the U.S. Food and Drug Administration ( FDA ). Chapter 2 (“Patterns of E-Cigarette Use Among U.S. Youth and Young Adults”) describes the epidemiology of e-cigarette use, including current use (i.e., past 30 day); ever use; co-occurrence of using e-cigarettes with other tobacco products, like cigarettes; and psychosocial factors associated with using e-cigarettes, relying on data from the most recent nationally representative studies available at the time this report was prepared. Chapter 3 (“Health Effects of E-Cigarette Use Among U.S. Youth and Young Adults”) documents the evidence related to the health effects of e-cigarette use, including those that are associated with direct aerosol inhalation by users, the indirect health effects of e-cigarette use, other non-aerosol health effects of e-cigarette use, and secondhand exposure to constituents of the aerosol. Chapter 4 (“Activities of the E-Cigarette Companies”) describes e-cigarette companies’ influences on e-cigarette use and considers manufacturing and price; the impact of price on sales and use; the rapid changes in the industry, particularly the e-cigarette companies; and the marketing and promotion of e-cigarettes. Chapter 5 (“E-Cigarette Policy and Practice Implications”) discusses the implications for policy and practice at the national, state, and local levels. The report ends with a Call to Action to stakeholders—including policymakers, public health practitioners and clinicians, researchers, and the public—to work to prevent harms from e-cigarette use and secondhand aerosol exposure among youth and young adults.
Preparation of this Report
This Surgeon General’s report was prepared by the Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC , which is part of USDHHS . The initial drafts of the chapters were written by 27 experts who were selected for their knowledge of the topics addressed. These contributions are summarized in five chapters that were evaluated by approximately 30 peer reviewers. After peer review, the entire manuscript was sent to more than 20 scientists and other experts, who examined it for its scientific integrity. After each review cycle, the drafts were revised by the report’s scientific editors on the basis of reviewers’ comments. Subsequently, the report was reviewed by various institutes and agencies within USDHHS.
Scientific Basis of the Report
The statements and conclusions throughout this report are documented by the citation of studies published in the scientific literature. Publication lags have prevented an up-to-the-minute inclusion of all recently published articles and data. This overall report primarily cites peer-reviewed journal articles, including reviews that integrate findings from numerous studies and books that were published through December 2015. However, selected studies from 2016 have been added during the review process that provide further support for the conclusions in this report. When a cited study has been accepted for publication, but the publication has not yet occurred because of the delay between acceptance and final publication, the study is referred to as “in press.” This report also refers, on occasion, to unpublished research, such as presentations at a professional meeting, personal communications from a researcher, or information available in various media. These references are employed when acknowledged by the editors and reviewers as being from reliable sources, which add to the emerging literature on a topic.
- Major Conclusions
- E-cigarettes are a rapidly emerging and diversified product class. These devices typically deliver nicotine, flavorings, and other additives to users via an inhaled aerosol. These devices are referred to by a variety of names, including “e-cigs,” “e-hookahs,” “mods,” “vape pens,” “vapes,” and “tank systems.”
- E-cigarette use among youth and young adults has become a public health concern. In 2014, current use of e-cigarettes by young adults 18–24 years of age surpassed that of adults 25 years of age and older.
- E-cigarettes are now the most commonly used tobacco product among youth, surpassing conventional cigarettes in 2014. E-cigarette use is strongly associated with the use of other tobacco products among youth and young adults, including combustible tobacco products.
- The use of products containing nicotine poses dangers to youth, pregnant women, and fetuses. The use of products containing nicotine in any form among youth, including in e-cigarettes, is unsafe.
- E-cigarette aerosol is not harmless. It can contain harmful and potentially harmful constituents, including nicotine. Nicotine exposure during adolescence can cause addiction and can harm the developing adolescent brain.
- E-cigarettes are marketed by promoting flavors and using a wide variety of media channels and approaches that have been used in the past for marketing conventional tobacco products to youth and young adults.
- Action can be taken at the national, state, local, tribal, and territorial levels to address e-cigarette use among youth and young adults. Actions could include incorporating e-cigarettes into smokefree policies, preventing access to e-cigarettes by youth, price and tax policies, retail licensure, regulation of e-cigarette marketing likely to attract youth, and educational initiatives targeting youth and young adults.
- Chapter Conclusions
Chapter 1. Introduction, Conclusions, and Historical Background Relative to E-Cigarettes
- E-cigarettes are devices that typically deliver nicotine, flavorings, and other additives to users via an inhaled aerosol. These devices are referred to by a variety of names, including “e-cigs,” “e-hookahs,” “mods,” “vape pens,” “vapes,” and “tank systems.”
- E-cigarettes represent an evolution in a long history of tobacco products in the United States, including conventional cigarettes.
- In May 2016, the Food and Drug Administration issued the deeming rule, exercising its regulatory authority over e-cigarettes as a tobacco product.
Chapter 2. Patterns of E-Cigarette Use Among U.S. Youth and Young Adults
- Among middle and high school students, both ever and past-30-day e-cigarette use have more than tripled since 2011. Among young adults 18–24 years of age, ever e-cigarette use more than doubled from 2013 to 2014 following a period of relative stability from 2011 to 2013.
- The most recent data available show that the prevalence of past-30-day use of e-cigarettes is similar among high school students (16% in 2015, 13.4% in 2014) and young adults 18–24 years of age (13.6% in 2013–2014) compared to middle school students (5.3% in 2015, 3.9% in 2014) and adults 25 years of age and older (5.7% in 2013–2014).
- Exclusive, past-30-day use of e-cigarettes among 8th-, 10th-, and 12th-grade students (6.8%, 10.4%, and 10.4%, respectively) exceeded exclusive, past-30-day use of conventional cigarettes in 2015 (1.4%, 2.2%, and 5.3%, respectively). In contrast—in 2013–2014 among young adults 18–24 years of age—exclusive, past-30-day use of conventional cigarettes (9.6%) exceeded exclusive, past-30-day use of e-cigarettes (6.1%). For both age groups, dual use of these products is common.
- E-cigarette use is strongly associated with the use of other tobacco products among youth and young adults, particularly the use of combustible tobacco products. For example, in 2015, 58.8% of high school students who were current users of combustible tobacco products were also current users of e-cigarettes.
- Among youth—older students, Hispanics, and Whites are more likely to use e-cigarettes than younger students and Blacks. Among young adults—males, Hispanics, Whites, and those with lower levels of education are more likely to use e-cigarettes than females, Blacks, and those with higher levels of education.
- The most commonly cited reasons for using e-cigarettes among both youth and young adults are curiosity, flavoring/taste, and low perceived harm compared to other tobacco products. The use of e-cigarettes as an aid to quit conventional cigarettes is not reported as a primary reason for use among youth and young adults.
- Flavored e-cigarette use among young adult current users (18–24 years of age) exceeds that of older adult current users (25 years of age and older). Moreover, among youth who have ever tried an e-cigarette, a majority used a flavored product the first time they tried an e-cigarette.
- E-cigarette products can be used as a delivery system for cannabinoids and potentially for other illicit drugs. More specific surveillance measures are needed to assess the use of drugs other than nicotine in e-cigarettes.
Chapter 3. Health Effects of E-Cigarette Use Among U.S. Youth and Young Adults
- Nicotine exposure during adolescence can cause addiction and can harm the developing adolescent brain.
- Nicotine can cross the placenta and has known effects on fetal and postnatal development. Therefore, nicotine delivered by e-cigarettes during pregnancy can result in multiple adverse consequences, including sudden infant death syndrome, and could result in altered corpus callosum, deficits in auditory processing, and obesity.
- E-cigarettes can expose users to several chemicals, including nicotine, carbonyl compounds, and volatile organic compounds, known to have adverse health effects. The health effects and potentially harmful doses of heated and aerosolized constituents of e-cigarette liquids, including solvents, flavorants, and toxicants, are not completely understood.
- E-cigarette aerosol is not harmless “water vapor,” although it generally contains fewer toxicants than combustible tobacco products.
- Ingestion of e-cigarette liquids containing nicotine can cause acute toxicity and possibly death if the contents of refill cartridges or bottles containing nicotine are consumed.
Chapter 4. Activities of the E-Cigarette Companies
- The e-cigarette market has grown and changed rapidly, with notable increases in total sales of e-cigarette products, types of products, consolidation of companies, marketing expenses, and sales channels.
- Prices of e-cigarette products are inversely related to sales volume: as prices have declined, sales have sharply increased.
- E-cigarette products are marketed in a wide variety of channels that have broad reach among youth and young adults, including television, point-of-sale, magazines, promotional activities, radio, and the Internet.
- Themes in e-cigarette marketing, including sexual content and customer satisfaction, are parallel to themes and techniques that have been found to be appealing to youth and young adults in conventional cigarette advertising and promotion.
Chapter 5. E-Cigarette Policy and Practice Implications
- The dynamic nature of the e-cigarette landscape calls for expansion and enhancement of tobacco-related surveillance to include (a) tracking patterns of use in priority populations; (b) monitoring the characteristics of the retail market; (c) examining policies at the national, state, local, tribal, and territorial levels; (d) examining the channels and messaging for marketing e-cigarettes in order to more fully understand the impact future regulations could have; and (e) searching for sentinel health events in youth and young adult e-cigarette users, while longer-term health consequences are tracked.
- Strategic, comprehensive research is critical to identify and characterize the potential health risks from e-cigarette use, particularly among youth and young adults.
- The adoption of public health strategies that are precautionary to protect youth and young adults from adverse effects related to e-cigarettes is justified.
- A broad program of behavioral, communications, and educational research is crucial to assess how youth perceive e-cigarettes and associated marketing messages, and to determine what kinds of tobacco control communication strategies and channels are most effective.
- Health professionals represent an important channel for education about e-cigarettes, particularly for youth and young adults.
- Diverse actions, modeled after evidence-based tobacco control strategies, can be taken at the state, local, tribal, and territorial levels to address e-cigarette use among youth and young adults, including incorporating e-cigarettes into smoke-free policies; preventing the access of youth to e-cigarettes; price and tax policies; retail licensure; regulation of e-cigarette marketing that is likely to attract youth and young adults, to the extent feasible under the law; and educational initiatives targeting youth and young adults. Among others, research focused on policy, economics, and the e-cigarette industry will aid in the development and implementation of evidence-based strategies and best practices.
- Historical Background
Understanding the role of e-cigarettes requires understanding the long history of tobacco use in the United States, including the role of nicotine delivery, the multiple examples of “reduced-harm” products and associated health claims, and the impact of using tobacco products on the public’s health. Since the late nineteenth century, when the “modern” cigarette came into use, scientists and public health officials have linked cigarette smoking to a remarkable number of adverse effects, and it is now recognized as the primary cause of premature death in the United States ( USDHHS 2014 ). Correspondingly, for a century, manufacturers, scientists, entrepreneurs, and public health leaders have promoted or recommended product changes that might remove some of the harmful elements in cigarette smoke. E-cigarettes are among the latest products.
E-cigarettes are designed for users to inhale nicotine, flavorings, and other additives through an aerosol. The claims and marketing strategies employed by the e-cigarette companies, and the efforts made by others to develop scientific and regulatory tools to deal with these new products, both contribute to the current discourse on e-cigarettes. Many lessons for assessing the potential (and future) consequences of these products can be learned from examining the relevant experiences of the past century, especially the introduction of novel products (including e-cigarettes as well as other tobacco and nicotine products) and the claims of reduced exposure to toxins made by the industry and elsewhere.
Early Efforts to Modify Cigarettes
In the 1880s and 1890s, entrepreneurs promoted novel products that allegedly blocked nicotine and other constituents of conventional cigarettes believed to be poisonous. Dr. Scott’s Electric Cigarettes, advertised in Harper’s Weekly, claimed not only to light without matches but also to contain a cotton filter that “strains and eliminates the injurious qualities from the smoke,” including nicotine ( Harper’s Weekly 1887 ). Nicotine delivery was essential to the development of the modern cigarette in the twentieth century; early on, this substance was thought to be addicting and thus vital to retaining customers. In 1913, the Camel brand was a new kind of cigarette that introduced high-nicotine content by using burley tobacco, which was generally too harsh to inhale into the lungs, but was made more inhalable through the addition of casings (e. g ., sugars, licorice) ( Tindall 1992 ; Proctor 2011 ). In 1916, American Tobacco introduced its Lucky Strike blended cigarette, and in 1918 Liggett & Myers ( L &M) reformulated its Chesterfield brand to make it more palatable to users. As the market grew, advertisements for major brands routinely included health-related statements and testimonials from physicians. During the 1930s and 1940s, prominent advertising campaigns included claims like “Not a cough in a carload” (Old Gold) ( Federal Trade Commission [FTC] 1964 , p. LBA-5); “We removed from the tobacco harmful corrosive ACRIDS (pungent irritants) present in cigarettes manufactured in the old-fashioned way” (Lucky Strike) ( FTC 1964 , p. LBA-2); and “Smoking Camels stimulates the natural flow of digestive fluids … increases alkalinity” (Camel) ( FTC 1964 , p. LBA-1a). Thus, early modifications to the cigarette were made so that it was more palatable, had a higher nicotine delivery and uptake, and could be marketed as “safe” ( FTC 1964 ; Calfee 1985 ).
Filters, Tar Reduction, and Light and Low-Tar Cigarettes
The landmark 1964 Surgeon General’s report on smoking and health concluded that cigarette smoking contributed substantially to mortality from certain specific diseases, including lung cancer ( U.S. Department of Health, Education, and Welfare 1964 ). Although the 1964 report considered the topic, it found the evidence insufficient to assess the potential health benefits of cigarette filters. Cigarettes with filters became the norm by the 1960s, and marketing them with an overt message about harm reduction became the standard ( National Cancer Institute [NCI] 1996 ). However, the Surgeon General convened another group of experts on June 1, 1966, to review the evidence on the role played by the tar and nicotine content in health. The group concluded that “[t]he preponderance of scientific evidence strongly suggests that the lower the ‘tar’ and nicotine content of cigarette smoke, the less harmful are the effects” ( Horn 1966 , p. 16,168). Subsequent studies have repeatedly failed to demonstrate health benefits of smoking light and low-tar cigarettes versus full-flavor cigarettes ( Herning et al. 1981 ; Russell et al. 1982 ; Benowitz et al. 1983 , NCI 2001 ).
Over the years, the tobacco industry used multiple methods to reduce the machine-tested yields of tar and nicotine in cigarettes as a way to claim “healthier” cigarettes. Beginning in the 1970s, tobacco companies advertised the tar and nicotine levels for their cigarettes, which encouraged smokers to believe, without substantiation, they could reduce their risk of exposure to these constituents ( Cummings et al. 2002 ; Pollay and Dewhirst 2002 ). In 1996, the FTC issued a statement that it would allow cigarette companies to include statements about tar and nicotine content in their advertising as long as they used a standardized machine-testing method ( Peeler 1996 ).
The Role of Nicotine and Nicotine Delivery
Although the public health community understood early on that nicotine was the primary psycho-active ingredient in cigarette smoke, before the 1980s, little was known about the importance of nicotine in the addiction process beyond what the cigarette manufacturers had learned from their own research. Some scientists warned that due to nicotine addiction, a reduction in nicotine yields, along with decreases in tar, could lead smokers to change their smoking behavior, such as by smoking a greater number of cigarettes to maintain their nicotine intake or changing their behavior in more subtle ways, such as varying the depth of inhalation or smoking more of the cigarette ( Jarvis et al. 2001 ; National Cancer Institute 2001 ; Thun and Burns 2001 ). Not until the 1970s and 1980s, as researchers studying other forms of drug abuse began to apply their research methods to cigarette smoking, did it become apparent that nicotine was similar in its addictive capability to other drugs of abuse, such as heroin and cocaine ( USDHHS 1981 , 1988 ). As described in the 1988 Surgeon General’s report and in subsequent research, symptoms associated with nicotine addiction include craving, withdrawal, and unconscious behaviors to ensure consistent intake of nicotine ( USDHHS 1988 ; al’Absi et al. 2002 ; Hughes 2007 ).
Although the tobacco industry has long understood the importance of nicotine to maintain long-term cigarette smokers through addiction, public health officials did not fully appreciate this in a broad sense until the 1988 Surgeon General’s report, The Health Consequences of Smoking: Nicotine Addiction ( USDHHS 1988 ).
FDA and Nicotine Regulation
In 1988 (and again in 1994), the Coalition on Smoking OR Health and other public-interest organizations petitioned FDA to classify low-tar and nicotine products as drugs and to classify Premier, the short-lived “smokeless cigarette product” from R.J. Reynolds, as an alternative nicotine-delivery system ( Stratton et al. 2001 ). The Coalition on Smoking OR Health cited indirect claims made through advertising and marketing as evidence of R. J. Reynolds’s intent to have the product used for the mitigation or prevention of disease ( Slade and Ballin 1993 ). Meanwhile, FDA launched an investigation into the practices of the tobacco industry, including the manipulation of nicotine delivery. FDA asserted its jurisdiction over cigarettes and smokeless tobacco and issued certain rules governing access to and promotion of these products ( Federal Register 1996 ). On March 21, 2000, the U.S. Supreme Court ruled 5-4 that Congress had not yet given FDA the necessary statutory authority to issue any rules pertaining to tobacco products ( Gottleib 2000 ; FDA v. Brown & Williamson Tobacco Corp. 2000 ). The subsequent debate over control of nicotine products, including their potential impact on youth, ultimately led to the passage of the 2009 Family Smoking Prevention and Tobacco Control Act, which gave FDA authority to regulate tobacco products. Thus, discussions about the introduction of novel nicotine-containing tobacco products in the market during the 1980s and 1990s helped shape the current regulation of tobacco and nicotine products.
New products introduced in the 1990s or later included modified tobacco cigarettes (e. g ., Advance, Omni); cigarette-like products, also called cigalikes (e.g., Eclipse, Accord); and smokeless tobacco products (e.g., Ariva, Exalt, Revel, snus). Advance, made by Brown and Williamson, was test-marketed with the slogan “All of the taste … Less of the toxins.” Vector launched a national advertising campaign for its Omni cigarette with the slogan “Reduced carcinogens. Premium taste.” In addition to the question of whether the claims were supported by sufficient evidence, scientists and tobacco control leaders raised concerns about the potential for adverse consequences associated with novel nicotine and tobacco products marketed for harm reduction, such as a reduction in cessation rates or increased experimentation by children ( Warner and Martin 2003 ; Joseph et al. 2004 ; Caraballo et al. 2006 ). Studies have shown that smokers are interested in trying novel “reduced-exposure” products and perceive them to have lower health risks, even when advertising messages do not make explicit health claims ( Hamilton et al. 2004 ; O’Connor et al. 2005 ; Caraballo et al. 2006 ; Choi et al. 2012 ; Pearson et al. 2012 ).
At FDA ’s request, the Institute of Medicine ( IOM [now the National Academy of Medicine]) convened a committee of experts to formulate scientific methods and standards by which potentially reduced-exposure products (PREPs), whether the purported reduction was pharmaceutical or tobacco related, could be assessed. The committee concluded that “[f]or many diseases attributable to tobacco use, reducing risk of disease by reducing exposure to tobacco toxicants is feasible” ( Stratton et al. 2001 , p. 232). However, it also cautioned that “PREPs have not yet been evaluated comprehensively enough (including for a sufficient time) to provide a scientific basis for concluding that they are associated with a reduced risk of dis ease compared to conventional tobacco use” ( Stratton et al. 2001 , p. 232). The committee added that “the major concern for public health is that tobacco users who might otherwise quit will use PREPs instead, or others may initiate smoking, feeling that PREPs are safe. That will lead to less harm reduction for a population (as well as less risk reduction for that individual) than would occur without the PREP , and possibly to an adverse effect on the population” ( Stratton et al. 2001 , p. 235). Subsequently, in 2006, Judge Kessler cited these findings in her decision which demanded the removal of light and low-tar labeling due to the misleading nature of these claims ( United States v. Philip Morris 2006 ).
- The E-Cigarette
Invention of the E-Cigarette
An early approximation of the current e-cigarette appeared in a U.S. patent application submitted in 1963 by Herbert A. Gilbert and was patented in August 1965 (U.S. Patent No. 3,200,819) ( Gilbert 1965 ). The application was for a “smokeless nontobacco cigarette,” with the aim of providing “a safe and harmless means for and method of smoking” by replacing burning tobacco and paper with heated, moist, flavored air. A battery-powered heating element would heat the flavor elements without combustion ( Gilbert 1965 ). The Favor cigarette, introduced in 1986, was another early noncombustible product promoted as an alternative nicotine-containing tobacco product ( United Press International 1986 ; Ling and Glantz 2005 ).
The first device in the recent innovation in e-cigarettes was developed in 2003 by the Chinese pharmacist Hon Lik, a former deputy director of the Institute of Chinese Medicine in Liaoning Province. Lik’s patent application described a kind of electronic atomizing cigarette ( Hon 2013 ). With support from Chinese investors, in 2004 the product was introduced on the Chinese market under the company name Ruyan ( Sanford and Goebel 2014 ). The product gained some attention among Chinese smokers early on as a potential cessation device or an alternative cigarette product.
The e-cigarette was part of the U.S. market by the mid-2000s, and by 2010 additional brands started to appear in the nation’s marketplace, including Ruyan and Janty ( Regan et al. 2013 ). Ruyan gained a U.S. patent for its product with the application stating that the product is “an electronic atomization cigarette that functions as substitutes (sic) for quitting smoking and cigarette substitutes.” (U.S. Patent No. 8,490,628 B2, 2013). In August 2013, Imperial Tobacco Group purchased the intellectual property behind the Ruyan e-cigarette for $75 million. As of 2014 an estimated 90% of the world’s production of e-cigarette technology and products came from mainland China, mainly Guangdong Province and Zhejiang Province ( Barboza 2014 ).
Sales of e-cigarettes in the United States have risen rapidly since 2007. Widespread advertising via television commercials and through print advertisements for popular brands, often featuring celebrities, has contributed to a large increase in e-cigarette use by both adults and youth since 2010 ( Felberbaum 2013 ; King et al. 2013 ; Regan et al. 2013 ). Additionally, marketing through social media, as well as other forms of Internet marketing, has been employed to market these devices ( Huang et al. 2014 ; Kim et al. 2014 ).
In 2013, an estimated 13.1 million middle school and high school students were aware of e-cigarettes ( Wang et al. 2014 ). According to data from the National Youth Tobacco Survey, in 2011 the prevalence of current e-cigarette use (defined as use during at least 1 day in the past 30 days) among high school students was 1.5%; prevalence increased dramatically, however, to 16% by 2015, surpassing the rate of conventional-cigarette use among high school students ( CDC 2016b ; see Chapter 2 ). This equates to 2.4 million high school students and 620,000 middle school students having used an e-cigarette at least one time in the past 30 days in 2015 ( CDC 2016b ).
These trends have led to substantial concern and discussion within public health communities, including state and national public health agencies, professional organizations, and school administrators and teachers. A primary concern is the potential for nicotine addiction among nonsmokers, especially youth and young adults, and that this exposure to nicotine among youth and young adults is harmful. The diversity and novelty of e-cigarette products on the market and ongoing product innovations make assessments of the biological effects of current e-cigarettes under actual conditions of use—such as their long-term harmfulness—difficult to measure. Unanswered questions remain about the risk profile of these devices, their potential use by young people as a first step to other nicotine products, and their total impact on public health. There are diverging opinions about the potential public health impact of these new products. Some public health scientists have highlighted the potential for alternative nicotine products to serve as a substitute for conventional cigarettes and thus a harm reduction tool ( Henningfield et al. 2003 ; Abrams 2014 ). Others have cautioned that the use of alternative nicotine products might become a bridge that may lead to greater tobacco product use—including dual- or multiple-product use—or initiate nicotine addiction among nonsmokers, especially youth ( Cobb et al. 2010 ; Wagener et al. 2012 ; Benowitz and Goniewicz 2013 ; Britton 2013 ; Chapman 2013 ; Etter 2013 ; USDHHS 2014 ). Current evidence is insufficient to reject either of these hypotheses.
E-Cigarette Products
Components and devices.
E-cigarette devices are composed of a battery, a reservoir for holding a solution that typically contains nicotine, a heating element or an atomizer, and a mouthpiece through which the user puffs ( Figure 1.2 ). The device heats a liquid solution (often called e-liquid or e-juice) into an aerosol that is inhaled by the user. E-liquid typically uses propylene glycol and/or glycerin as a solvent for the nicotine and flavoring chemicals
Parts of an e-cigarette device. Source: Photo by Mandie Mills, CDC.
Flavors and E-Cigarettes
The e-liquids in e-cigarettes are most often flavored; a study estimated that 7,700 unique flavors exist ( Zhu et al. 2014 ) and that most of them are fruit or candy flavors ( Figure 1.3 ). A content analysis of the products available via online retail websites documented that tobacco, mint, coffee, and fruit flavors were most common, followed by candy (e. g ., bubble gum), unique flavors (e.g., Belgian waffle), and alcoholic drink flavors (e.g., strawberry daiquiri) ( Grana and Ling 2014 ). Some retail stores are also manufacturers that create custom flavors, which increases the variety of flavors available.
Examples of e-liquid flavors. Source: Photo by Mandie Mills, CDC.
The widespread availability and popularity of flavored e-cigarettes is a key concern regarding the potential public health implications of the products. The concern, among youth, is that the availability of e-cigarettes with sweet flavors will facilitate nicotine addiction and simulated smoking behavior—which will lead to the use of conventional tobacco products ( Kong et al. 2015 ; Krishnan-Sarin et al. 2015 ). Flavors have been used for decades to attract youth to tobacco products and to mask the flavor and harshness of tobacco ( USDHHS 2012 ). Industry documents show that tobacco companies marketed flavored little cigars and cigarillos to youth and to African Americans to facilitate their uptake of cigarettes ( Kostygina et al. 2014 ). Companies also intended flavored smokeless tobacco products to facilitate “graduation” to unflavored products that more easily deliver more nicotine to the user ( USDHHS 2012 ). Various studies have shown that youth are more likely than adults to choose flavored cigarettes and cigars ( CDC 2015b ). Concern over these findings led Congress to include a ban on characterizing flavors for cigarettes, other than tobacco or menthol, in the Tobacco Control Act. A similar concern exists about e-cigarettes, and this concern is supported by studies indicating that youth and young adults who have ever used e-cigarettes begin their use with sweet flavors rather than tobacco flavors ( Kong et al. 2015 ; Krishnan-Sarin et al. 2015 ). Notably, 81.5% of current youth e-cigarette users said they used e-cigarettes “because they come in flavors I like” ( Ambrose et al. 2015 ).
E-Cigarette Devices
First-generation e-cigarettes were often similar in size and shape to conventional cigarettes, with a design that also simulated a traditional cigarette in terms of the colors used (e. g ., a white body with tan mouthpiece). These devices were often called cigalikes, but there were other products designed to simulate a cigar or pipe. Other cigalikes were slightly longer or narrower than a cigarette; they may combine white with tan or may be black or colored brightly. These newer models use a cartridge design for the part of the device that holds the e-liquid, which is either prefilled with the liquid or empty and ready to be filled. The user then squeezes drops of the e-liquid onto a wick (or bit of cotton or polyfil) connected to the heating element and atomizer ( Figure 1.4 ). As e-cigarettes have become more popular, their designs have become more diverse, as have the types of venues where they are sold ( Noel et al. 2011 ; Zhu et al. 2014 ).
E-liquids being poured into an e-cigarette device. Source: Photo by Mandie Mills, CDC.
Second-generation devices include products that are shaped like pens, are comparatively larger and cylindrical, and are often referred to as “tank systems” in a nod to the transparent reservoir that holds larger amounts of e-liquid than previous cartridge-containing models. Third- and fourth-generation devices represent a diverse set of products and, aesthetically, constitute the greatest departure from the traditional cigarette shape, as many are square or rectangular and feature customizable and rebuildable atomizers and batteries. In addition, since the beginning of the availability of e-cigarettes and their component parts, users have been modifying the devices or building their own devices, which are often referred to as “mods.” The differences in design and engineering of the products are key factors in the size, distribution, and amount of aerosol particles and the variability in levels of chemicals and nicotine present in the e-liquid/aerosol and delivered to the user ( Brown and Cheng 2014 ).
E-Cigarette Product Components and Risks
One of the primary features of the more recent generation of devices is that they contain larger batteries and are capable of heating the liquid to a higher temperature, potentially releasing more nicotine, forming additional toxicants, and creating larger clouds of particulate matter ( Bhatnagar et al. 2014 ; Kosmider et al. 2014 ). For instance, one study demonstrated that, at high temperatures (150°C), exceedingly high levels of formaldehyde—a carcinogen (found to be 10 times higher than at ambient temperatures)—are present that are formed through the heating of the e-liquid solvents (propylene glycol and glycerin), although the level of tolerance of actual users to the taste of the aerosol heated to this temperature is debated ( Kosmider et al. 2014 ; CDC 2015a ; Flavor and Extract Manufacturers Association of the United States 2015 ; Pankow et al. 2015 ). There is also concern regarding the safety of inhaling e-cigarette flavorings. Although some manufacturers have claimed their flavorants are generally recognized as safe for food additives (i.e., to be used in preparing foods for eating), little is known about the long-term health effects of inhaling these substances into the lungs ( CDC 2015a ).
Many devices can be readily customized by their users, which is also leading to the concern that these devices are often being used to deliver drugs other than nicotine ( Brown and Cheng 2014 ). Most commonly reported in the news media, on blogs, and by user anecdote is the use of certain types of e-cigarette-related products for delivering different forms of marijuana ( Morean et al. 2015 ; Schauer et al. 2016 ). The tank systems, for example, have been used with liquid tetrahydrocannabinol ( THC ) or hash oil. Some personal vaporizer devices can be used with marijuana plant material or a concentrated resin form of marijuana called “wax.” One study describes the use, in Europe, of e-cigarette devices to smoke marijuana ( Etter 2015 ).
The various e-cigarette products, viewed as a group, lack standardization in terms of design, capacity for safely holding e-liquid, packaging of the e-liquid, and features designed to minimize hazards with use ( Yang et al. 2014 ). All of these design features may have implications for the health impact of e-cigarette use. Notably, from 2010 to 2014, calls to poison control centers in the United States about exposures related to e-cigarettes increased dramatically. According to the American Association of Poison Control Centers (2015) , 271 cases were reported in 2011, but 3,783 calls were reported in 2014. Among all calls, 51% involved exposure among children younger than 5 years of age ( CDC 2014 ). Most poisonings appear to have been caused by exposure to nicotine-containing liquid ( CDC 2014 ). The lack of a requirement for child-resistant packaging for e-liquid containers may have contributed to these poisonings. Since these data were released, one death in the United States has been confirmed in a child who drank e-liquid containing nicotine ( Mohney 2014 ). Additionally, serious adverse reactions, including at least two deaths, have been reported to FDA in cases that could be attributed to the use of e-cigarettes ( FDA 2013 ). This increase in poisonings prompted the Child Nicotine Poisoning Prevention Act of 2015 (2016) , which was enacted in January 2016. This law requires any container of liquid nicotine that is sold, manufactured, distributed, or imported into the United States to be placed in packaging that is difficult to open by children under 5 years of age.
Secondary risks are also of concern regarding e-cigarettes, including passive exposure to nicotine and other chemicals, and adverse events due to device malfunction. Nicotine is a neuroteratogen, and its use by pregnant women exposes a developing fetus to risks that are well documented in the 50th-anniversary Surgeon General’s report on smoking ( USDHHS 2014 ) and include impaired brain development ( England et al. 2015 ) and other serious consequences. Finally, another consequence of the lack of device regulation is the occurrence of battery failures and subsequent explosions. Explosions have typically occurred during charging, resulting in house and car fires, and sometimes causing injuries to those involved. From 2009 to late 2014, 25 incidents of explosions and fires involving e-cigarettes occurred in the United States ( Chen 2013 ; U.S. Fire Administration 2014 ; FDA 2013 ).
- E-Cigarette Companies
E-cigarette companies include manufacturers, wholesalers, importers, retailers, distributors, and some other groups that overlap with these entities ( Barboza 2014 ; Whelan 2015 ). Currently, most of the products are manufactured in Shenzhen, Guangdong Province, China ( Cobb et al. 2010 ; Grana et al. 2014 ; Zhu et al. 2014 ). One study placed the number of brands at 466 in January 2014 and found a net increase of 10.5 brands per month ( Zhu et al. 2014 ). All the major tobacco companies (e. g ., Reynolds American, Altria; Table 1.1 ) and many smaller, independent companies are now in the business. When e-cigarettes first entered the U.S. market, they were sold primarily by independent companies via the Internet and in shopping malls at kiosks where those interested could sample the products. A unique feature of the e-cigarette industry, compared to other tobacco and nicotine products, is the recruitment of visitors to their websites as “affiliates” or distributors to help market the products and, in turn, receive commissions on sales ( Grana and Ling 2014 ; Cobb et al. 2015 ). For example, some companies offer a way for users to earn a commission by advertising the products (e.g., a banner ad is placed on one’s website, and when someone clicks on the link and subsequently purchases a product, the website owner gets a percentage commission). Some companies also offer rewards programs for recruiting new customers or for brand loyalty, with web-site users earning points for free or reduced-price products ( Richardson et al. 2015 ).
Multinational tobacco companies with e-cigarette brands.
E-cigarettes are now in widespread national distribution through convenience stores, tobacco stores, pharmacies, “big box” retail chains such as Costco, online retailers, and shops devoted to e-cigarette products (often called “vape shops”) ( Giovenco et al. 2015 ; Public Health Law Center 2015 ). The “vape shops” offer a place to buy customizable devices and e-liquid solutions in many flavors and sometimes include a café or other elements that promote socializing, essentially making such places like a lounge. With the rapid increase in distribution and marketing in the industry, sales have increased rapidly and were projected to reach $2.5 billion in 2014 and $3.5 billion in 2015, including projections for retail and online channels, as well as “vape shops” ( Wells Fargo Securities 2015 ).
The advertising and marketing of e-cigarette products has engendered skepticism among public health professionals and legislators, who have noted many similarities to the advertising claims and promotional tactics used for decades by the tobacco industry to sell conventional tobacco products ( Campaign for Tobacco-Free Kids 2013 ; CDC 2016a ). Indeed, several of the e-cigarette marketing themes have been reprised from the most memorable cigarette advertising, including those focused on freedom, rebellion, and glamor ( Grana and Ling 2014 ). E-cigarette products are marketed with a variety of unsubstantiated health and cessation messages, with some websites featuring videos of endorsements by physicians (another reprisal of old tobacco industry advertising) ( Grana and Ling 2014 ; Zhu et al. 2014 ). Unlike conventional cigarettes, for which advertising has been prohibited from radio and television since 1971, e-cigarette products are advertised on both radio and television, with many ads featuring celebrities. E-cigarettes also are promoted through sports and music festival sponsorships, in contrast to conventional cigarettes and smokeless tobacco products, which have been prohibited from such sponsorships since the Master Settlement Agreement in 1998. E-cigarettes also appear as product placements in television shows and movies ( Grana et al. 2011 ; Grana and Ling 2014 ).
Another key avenue for e-cigarette promotion is social media, such as Twitter, Facebook, YouTube, and Instagram. As is true in the tobacco industry, the e-cigarette industry organizes users through advocacy groups ( Noel et al. 2011 ; Harris et al. 2014 ; Saitta et al. 2014 ; Caponnetto et al. 2015 ). The extensive marketing and advocacy through various channels broadens exposure to e-cigarette marketing messages and products; such activity may encourage nonsmokers, particularly youth and young adults, to perceive e-cigarette use as socially normative. The plethora of unregulated advertising is of particular concern, as exposure to advertising for tobacco products among youth is associated with cigarette smoking in a dose-response fashion ( USDHHS 2012 ).
- Federal Regulation of E-Cigarettes
A “Two-Pronged” Approach to Comprehensive Tobacco Control
Since the passage of the Tobacco Control Act in 2009, FDA has had the authority to regulate the manufacturing, distribution, and marketing of tobacco products sold in the United States. FDA had immediate jurisdiction over cigarettes, roll-your-own cigarette tobacco, and smokeless tobacco. In May 2016, FDA asserted jurisdiction over products that meet the statutory definition of a tobacco product, including e-cigarettes, except accessories of these products ( Federal Register 2016 ). That regulation is currently under litigation.
The IOM ’s 2007 report, Ending the Tobacco Problem: A Blueprint for the Nation, established a “two-pronged” strategy for comprehensive tobacco control: (1) full implementation of proven, traditional tobacco control measures such as clean indoor air laws, taxation, and countermarketing campaigns; and (2) “strong federal regulation of tobacco products and their marketing and distribution” ( Bonnie et al. 2007 , p. 1).
Included in FDA ’s broad authority are the restriction of marketing and sales to youth, requiring disclosure of ingredients and harmful and potentially harmful constituents, setting product standards (e. g ., requiring the reduction or elimination of ingredients or constituents), requiring premarket approval of new tobacco products and review of modified-risk tobacco products, and requiring health warnings. The standard for FDA to use many of its regulatory authorities is whether such an action is appropriate for the protection of public health ( Federal Food, Drug, and Cosmetic Act , § 907(a)(3)(A)). The public health standard in the Tobacco Control Act also requires FDA to consider the health impact of certain regulatory actions at both the individual and population levels, including their impact on nonusers, and on initiation and cessation ( Federal Food, Drug, and Cosmetic Act , § 907(a)(3)(B)).
Importantly, the Tobacco Control Act preserves the authority of state, local, tribal, and territorial governments to enact any policy “in addition to, or more stringent than” requirements established under the Tobacco Control Act “relating to or prohibiting the sale, distribution, possession, exposure to, access to, advertising and promotion of, or use of tobacco products by individuals of any age” ( Federal Food, Drug, and Cosmetic Act , § 916(a)(1)). This preservation of state and local authority ensures the continuation of more local-level, comprehensive tobacco control. However, the statute expressly preempts states and localities from establishing or continuing requirements that are different from or in addition to FDA requirements regarding standards for tobacco products, premarket review, adulteration, misbranding, labeling, registration, good manufacturing practices, or modified-risk tobacco products ( Federal Food, Drug, and Cosmetic Act , § 916(a)(2)(A)). But this express preemption provision does not apply to state and local authority to impose requirements relating to the “sale, distribution, possession, information reporting to the State, exposure to, access to, the advertising and promotion of, or use of, tobacco products by individuals of any age …” ( Federal Food, Drug, and Cosmetic Act , § 916(a)(2)(b)). The interaction of these complex provisions related to federal preemption of state law has been the subject of challenges by the tobacco industry to state and local laws. Thus far, courts have upheld certain local ordinances restricting the sale of flavored tobacco products ( National Association of Tobacco Outlets, Inc. v. City of Providence 2013 ; U.S. Smokeless Tobacco Manufacturing Co. v. City of New York 2013 ).
Legal Basis for Regulating E-Cigarettes as Tobacco Products
In the United States, e-cigarettes can be regulated either as products marketed for therapeutic purposes or as tobacco products. Since the advent of e-cigarettes in the United States around 2007, manufacturers have had the option to apply to FDA ’s Center for Drug Evaluation and Research ( CDER ) or Center for Devices and Radiological Health (CDRH) for approval to market e-cigarettes for therapeutic purposes; as of August 2016, no e-cigarette manufacturers have received approval through this avenue.
In 2008 and early 2009, FDA detained multiple shipments of e-cigarettes from overseas manufacturers and denied them entry into the United States on the grounds that e-cigarettes were unapproved drug-device combination products ( FDA 2011 ). Sottera, Inc., which now does business as NJOY, challenged that determination ( Smoking Everywhere, Inc. and Sottera, Inc., d/b/a NJOY v. U.S. Food and Drug Administration, et al. 2010 ; Bloomberg Business 2015 ). Between the filing of the lawsuit and a decision on the motion for preliminary injunction, Congress passed the Tobacco Control Act and the President signed it into law. The Tobacco Control Act defines the term “tobacco product,” in part, as any product, including component parts or accessories, “made or derived from tobacco” that is not a “drug,” “device,” or “combination product” as defined by the Federal Food, Drug, and Cosmetic Act (21 U.S.C. 321(rr)) ( Family Smoking Prevention and Tobacco Control Act 2009 , § 101(a)). The District Court subsequently granted a preliminary injunction relying on the Supreme Court’s decision in Brown and Williamson (1996) and the recently enacted Tobacco Control Act. FDA appealed the decision and the U.S. Court of Appeals for the D.C. Circuit held that e-cigarettes and, therefore, other products “made or derived from tobacco” are not drug/device combinations unless they are marketed for therapeutic purposes, but can be regulated by FDA as tobacco products under the Tobacco Control Act ( Sottera, Inc. v. Food & Drug Administration 2010 ).
On September 25, 2015, FDA proposed regulations to describe the circumstances in which a product made or derived from tobacco that is intended for human consumption will be subject to regulation as a drug, device, or a combination product. The comment period for this proposed regulation closed on November 24, 2015.
Most e-cigarettes marketed and sold in the United States today contain nicotine made or derived from tobacco. Although some e-cigarettes claim that they contain nicotine not derived from tobacco, or that they contain no nicotine at all ( Lempert et al. 2016 ), there may be reason to doubt some of these claims. Currently, synthetic nicotine and nicotine derived from genetically modified, nontobacco plants are cost-prohibitive for e-cigarette manufacturers, although technological advances could eventually increase the cost-effectiveness of using nicotine that was not derived from tobacco ( Lempert et al. 2016 ). The health effects of passive exposure to e-cigarettes with no nicotine, as well as their actual use and the extent of exposure to these products, have just begun to be studied ( Hall et al. 2014 ; Marini et al. 2014 ; Schweitzer et al. 2015 ) and some states and localities are taking steps to regulate e-cigarettes that do not contain nicotine or tobacco ( Lempert et al. 2016 ).
Deeming Rule
The Tobacco Control Act added a new chapter to the Federal Food, Drug, and Cosmetic Act , which provides FDA with authority over tobacco products. The new chapter applied immediately to all cigarettes, cigarette tobacco, roll-your-own tobacco, and smokeless tobacco; and the law included “any other tobacco products that the Secretary of Health and Human Services by regulation deems to be subject to this chapter” ( Federal Food, Drug, and Cosmetic Act , §901 (b)). Therefore, to regulate e-cigarettes as tobacco products, FDA was required to undertake a rulemaking process to extend its regulatory authority to include e-cigarettes.
- Prohibitions on adulterated and misbranded products;
- Required disclosure of existing health information, including lists of ingredients and documents on health effects;
- Required registration of manufacturers;
- Required disclosure of a list of all tobacco products, including information related to labeling and advertising;
- Premarket review of new tobacco products (i.e., those not on the market on February 15, 2007);
- Restrictions on products marketed with claims about modified risk.
- Minimum age restrictions to prevent sales to minors;
- Requirements to include a nicotine warning; and
- Prohibitions on vending machine sales, unless in a facility that never admits youth.
Future Regulatory Options
- Product standards, including restrictions on flavors;
- Restrictions on promotion, marketing, and advertising, and prohibitions on brand-name sponsorship of events;
- Minimum package sizes;
- Prohibitions on self-service displays;
- Child-resistant packaging and the inclusion of health warnings; and
- Regulation of nicotine levels in products.
Despite this broad authority, FDA is prohibited from certain regulatory actions, even if those actions may be appropriate for the protection of public health. Specifically, FDA generally cannot restrict tobacco use in public places, levy taxes on tobacco products, prohibit sales by a specific category of retail outlet (e. g ., pharmacies), completely eliminate nicotine in tobacco products, require prescriptions for tobacco products unless it is marketed for therapeutic purposes, or establish a federal minimum age of sale for tobacco products above 18 years of age. Thus, even if FDA fully exercises all of its existing authority over e-cigarettes, regulation will still need to be complemented at the state and local levels, including efforts previously shown to be effective for conventional tobacco products, such as comprehensive smokefree laws at the state and local levels, pricing strategies, raising the minimum age of sales to minors to 21, and high-impact countermarketing campaigns. In the current context of rising rates of use by youth, localities and states can also implement policies and programs that minimize the individual- and population-level harms of e-cigarettes (see Chapter 5 ).
This chapter presents the major conclusions of this Surgeon General’s report and the conclusions of each chapter. E-cigarettes are presented within their historical context, with an overview of the components of these devices and the types of products. In 2016, FDA announced its final rule to regulate e-cigarettes under the Family Smoking Prevention and Tobacco Control Act. The chapter outlines options for the regulation of e-cigarettes, particularly as they relate to youth and young adults, based on successful smoking policies. The need to protect youth and young adults from initiating or continuing the use of nicotine-containing products forms a strong basis for the need to regulate e-cigarettes at the local, state, and national levels in the future.
- Abrams DB. Promise and peril of e-cigarettes: can disruptive technology make cigarettes obsolete? JAMA: the Journal of the American Medical Association 2014;311(2):135–6. [ PubMed : 24399548 ]
- al’Absi M, Amunrud T, Wittmers LE. Psychophysiological effects of nicotine abstinence and behavioral challenges in habitual smokers. Pharmacology Biochemistry and Behavior 2002;72(3):707–16. [ PubMed : 12175468 ]
- Alexander JP, Coleman BN, Johnson SE, Tesseman GK, Tworek C, Dickinson DM. Smoke and vapor: exploring the terminology landscape among electronic cigarette users. Tobacco Regulation Science 2016;2(3):201–13. [ PMC free article : PMC4944844 ] [ PubMed : 27430008 ]
- Ambrose BK, Day HR, Rostron B, Conway KP, Borek N, Hyland A, Villanti AC. Flavored tobacco product use among U.S. youth aged 12–17 years, 2013–2014. JAMA: the Journal of the American Medical Association 2015;314(17):1871–3. [ PMC free article : PMC6467270 ] [ PubMed : 26502219 ]
- American Association of Poison Control Centers. Electronic Cigarettes and Liquid Nicotine Data, 2015; < https://aapcc .s3.amazonaws .com/files/library /E-cig__Nicotine_Web_Data_through_3 .2015.pdf >; accessed: April 30, 2015.
- Barboza D. China’s e-cigarette boom lacks oversight for safety. New York Times, December 13, 2014; < http://nyti .ms/1zNA4da >; accessed: October 28, 2015.
- Benowitz NL, Goniewicz ML. The regulatory challenge of electronic cigarettes. JAMA: the Journal of the American Medical Association 2013;310(7):685–6. [ PubMed : 23856948 ]
- Benowitz NL, Hall SM, Herning RI, Jacob III P, Jones RT, Osman AL. Smokers of low-yield cigarettes do not consume less nicotine. New England Journal of Medicine 1983;309(3):139–42. [ PubMed : 6866013 ]
- Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C, Chaloupka F, Piano MR, Robertson RM, McAuley T, Goff D, Benowitz N. Electronic cigarettes: a policy statement from the American Heart Association. Circulation 2014;130(16):1418–36. [ PMC free article : PMC7643636 ] [ PubMed : 25156991 ]
- Bialous SA, Sarma L. Electronic cigarettes and smoking cessation: a quandary? Lancet 2014;383(9915):407–8. [ PubMed : 24485576 ]
- Bloomberg Business. Company overview of Sottera, Inc, 2015; < http://www .bloomberg .com/research/stocks/private/snapshot .asp?privcapId=52089038 >; accessed: June 22, 2015.
- Bonnie RJ, Stratton KR, Wallace RB, editors. Ending the Tobacco Problem: A Blueprint for the Nation . Washington (DC): National Academies Press, 2007.
- Britton J. Electronic cigarettes. Thorax 2013;68(10):904–5. [ PubMed : 23939400 ]
- Brown CJ, Cheng JM. Electronic cigarettes: product characterisation and design considerations. Tobacco Control 2014;23:(Suppl 2): ii4–ii10. [ PMC free article : PMC3995271 ] [ PubMed : 24732162 ]
- Calfee JE. Cigarette Advertising, Health Information and Regulation Before 1970 . Working Paper No. 134. Washington (DC): Bureau of Economics, Federal Trade Commission, 1985.
- Campaign for Tobacco-Free Kids. 7 ways e-cigarette companies are copying big tobacco’s playbook, October 2, 2013; < http://www .tobaccofreekids .org/tobacco_unfiltered /post/2013_10_02_ecigarettes >; accessed: April 20, 2016.
- Caponnetto P, Saitta D, Sweanor D, Polosa R. What to consider when regulating electronic cigarettes: pros, cons and unintended consequences. International Journal on Drug Policy 2015;26(6):554–9. [ PubMed : 25857204 ]
- Caraballo RS, Pederson LL, Gupta N. New tobacco products: do smokers like them? Tobacco Control 2006;15(1):39–44. [ PMC free article : PMC2563627 ] [ PubMed : 16436404 ]
- Centers for Disease Control and Prevention. Notes from the field: calls to poison centers for exposures to electronic cigarettes—United States, September 2010–February 2014. Morbidity and Mortality Weekly Report 2014;63(13):292–3. [ PMC free article : PMC5779356 ] [ PubMed : 24699766 ]
- Centers for Disease Control and Prevention. Electronic Nicotine Delivery Systems: Key Facts, 2015a; < http://www .cdc.gov/tobacco /stateandcommunity /pdfs/ends-key-facts2015.pdf >; accessed: November 3, 2015.
- Centers for Disease Control and Prevention. Flavored tobacco product use among middle and high school students—United States, 2014. Morbidity and Mortality Weekly Report 2015b;64(38):1066–70. [ PubMed : 26421418 ]
- Centers for Disease Control and Prevention. Tobacco use among middle and high school students—United States, 2011–2014. Morbidity and Mortality Weekly Report 2015c;64(14):381–5. [ PMC free article : PMC5779546 ] [ PubMed : 25879896 ]
- Centers for Disease Control and Prevention. E-cigarette ads reach nearly 7 in 10 middle and high-school students, January 5, 2016a; < http://www .cdc.gov/media /releases/2016/p0105-e-cigarettes .html >; accessed: April 20, 2016.
- Centers for Disease Control and Prevention. Tobacco use among middle and high school students—United States, 2011–2015. Morbidity and Mortality Weekly Report 2016b;65(14):361–7. [ PubMed : 27077789 ]
- Chapman S. Should electronic cigarettes be as freely available as tobacco cigarettes? BMJ 2013;346:f3840. [ PubMed : 23771038 ]
- Chen IL. FDA summary of adverse events on electronic cigarettes. Nicotine & Tobacco Research 2013;15(2):615–6. [ PubMed : 22855883 ]
- Child Nicotine Poisoning Prevention Act of 2015 , Public Law 114–116, 130 U.S. Statutes at Large 3 (2016).
- Choi K, Fabian L, Mottey N, Corbett A, Forster J. Young adults’ favorable perceptions of snus, dissolvable tobacco products, and electronic cigarettes: findings from a focus group study. American Journal of Public Health 2012;102(11):2088–93. [ PMC free article : PMC3469759 ] [ PubMed : 22813086 ]
- Cobb NK, Brookover J, Cobb CO. Forensic analysis of online marketing for electronic nicotine delivery systems. Tobacco Control 2015;24(2):128–31. [ PubMed : 24038037 ]
- Cobb NK, Byron MJ, Abrams DB, Shields PG. Novel nicotine delivery systems and public health: the rise of the “e-cigarette”. American Journal of Public Health 2010;100(12):2340–2. [ PMC free article : PMC2978165 ] [ PubMed : 21068414 ]
- Cummings KM, Morley CP, Hyland A. Failed promises of the cigarette industry and its effect on consumer misperceptions about the health risks of smoking. Tobacco Control 2002;11:(Suppl 1):i110–i117. [ PMC free article : PMC1766060 ] [ PubMed : 11893821 ]
- England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA. Nicotine and the developing human: a neglected element in the electronic cigarette debate. American Journal of Preventive Medicine 2015;49:286. [ PMC free article : PMC4594223 ] [ PubMed : 25794473 ]
- Etter JF. Commentary on Dawkins et al. (2013): the current legislation on nicotine causes millions of deaths—it has to change. Addiction 2013;108(6):1126. [ PubMed : 23659845 ]
- Etter JF. Electronic cigarettes and cannabis: an exploratory study. European Addiction Research 2015;21(3):124–30. [ PubMed : 25613866 ]
- Family Smoking Prevention and Tobacco Control Act, Public Law 111–31, 123 U.S. Statutes at Large 1776 (2009).
- Farsalinos KE, Polosa R. Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: a systematic review. Therapeutic Advances in Drug Safety 2014;5(2):67–86. [ PMC free article : PMC4110871 ] [ PubMed : 25083263 ]
- FDA v. Brown & Williamson Tobacco Corp ., 120 S. Ct. 1291 (2000).
- Federal Register . U.S. Department of Health and Human Services, Food and Drug Administration. Deeming Tobacco Products To Be Subject to the Federal Food, Drug, and Cosmetic Act, as Amended by the Family Smoking Prevention and Tobacco Control Act; Restrictions on the Sale and Distribution of Tobacco Products and Required Warning Statements for Tobacco Products. 81 Fed. Reg . 28974 (2016); < https: //federalregister.gov/a/2016-10685 >; accessed: May 16, 2016. [ PubMed : 27192730 ]
- Federal Register . U.S. Department of Health and Human Services, Food and Drug Administration. Regulations restricting the sale and distribution of cigarettes and smokeless tobacco to protect children and adolescents (21 CFR Parts 801, 803, 804, 807, 820, and 897), 61 Fed. Reg . 44396–5318 (1996).
- Federal Trade Commission. A Report on Cigarette Advertising and Output: Staff Report of the Bureau of Economics. Federal Trade Commission. 1964. RJ Reynolds Collection. Bates No. 515698078–515698370. < http://legacy .library .ucsf.edu/tid/ywm92d00 >.
- Felberbaum MF. Old tobacco playbook gets new use by e-cigarettes, 2013; < http://bigstory .ap.org /article/old-tobacco-playbook-gets-new-use-e-cigarettes >; accessed: July 22, 2015.
- Flavor and Extract Manufacturers Association of the United States. The Safety Assessment and Regulatory Authority to Use Flavors—Focus on E-Cigarettes , 2015; < http://www .femaflavor .org/sites/default/files /FEMAGRAS_Ecig_March_3_2015.pdf >; accessed: May 21, 2015.
- Franck C, Budlovsky T, Windle SB, Filion KB, Eisenberg MJ. Electronic cigarettes in North America: history, use, and implications for smoking cessation. Circulation 2014;129(19):1945–52. [ PubMed : 24821825 ]
- Gilbert AH. U.S. Patent No. 3,200,819. 1965. Brown & Williamson Collection. Bates No. 570328916–570328920. < http: //industrydocuments .library.ucsf.edu /tobacco/docs/hzxb0140 >.
- Giovenco DP, Hammond D, Corey CG, Ambrose BK, Delnevo CD. E-cigarette market trends in traditional U.S. retail channels, 2012–2013. Nicotine & Tobacco Research 2015;17(10):1279–83. [ PMC free article : PMC4683368 ] [ PubMed : 25542918 ]
- Gottleib S. Supreme Court rules that FDA cannot regulate tobacco industry. BMJ 2000;320(7239):894. [ PubMed : 10787253 ]
- Grana RA, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation 2014;129(19):1972–86. [ PMC free article : PMC4018182 ] [ PubMed : 24821826 ]
- Grana RA, Glantz SA, Ling PM. Electronic nicotine delivery systems in the hands of Hollywood. Tobacco Control 2011;20(6):425–6. [ PMC free article : PMC3184316 ] [ PubMed : 21659450 ]
- Grana RA, Ling PM. “Smoking revolution:” a content analysis of electronic cigarette retail websites. American Journal of Preventive Medicine 2014;46(4):395–403. [ PMC free article : PMC3989286 ] [ PubMed : 24650842 ]
- Hagopian A, Halperin A, Atwater P, Fradkin N, Gilroy JH, Medeiros E. E-Cigarettes: Evidence and Policy Options for Washington State . Seattle (WA): University of Washington, School of Public Health, Department of Health Services, January 2015; < http://www .governor.wa .gov/sites/default /files/documents/ECigWhitePaper.PDF >; accessed: October 20, 2015.
- Hall BJ, Wells C, Allenby C, Lin MY, Hao I, Marshall L, Rose JE, Levin ED. Differential effects of non-nicotine tobacco constituent compounds on nicotine self-administration in rats. Pharmacology, Biochemistry and Behavior 2014;120:103–8. [ PMC free article : PMC4000725 ] [ PubMed : 24560911 ]
- Hamilton WL, Norton G, Ouellette TK, Rhodes WM, Kling R, Connolly GN. Smokers’ responses to advertisements for regular and light cigarettes and potential reduced-exposure tobacco products. Nicotine & Tobacco Research 2004;6:(Suppl 3):S353–S362. [ PubMed : 15799598 ]
- Harper’s Weekly . A remarkable invention! Dr. Scott’s electric cigarettes [advertisement]. Harper’s Weekly , 1887;Sect 48 (col 1–2); < http://tobacco .harpweek .com/hubpages/CommentaryPage .asp?Commentary=References >; accessed: July 7, 2015.
- Harris JK, Moreland-Russell S, Choucair B, Mansour R, Staub M, Simmons K. Tweeting for and against public health policy: response to the Chicago Department of Public Health’s electronic cigarette Twitter campaign. Journal of Medical Internet Research 2014;16(10):e238. [ PMC free article : PMC4210950 ] [ PubMed : 25320863 ]
- Henningfield JE, Moolchan ET, Zeller M. Regulatory strategies to reduce tobacco addiction in youth. Tobacco Control 2003;12:(Suppl 1):i14–i24. [ PMC free article : PMC1766091 ] [ PubMed : 12773782 ]
- Herning RI, Jones RT, Bachman J, Mines AH. Puff volume increases when low-nicotine cigarettes are smoked. BMJ (Clin Res Ed) 1981;283(6285):187–9. [ PMC free article : PMC1506678 ] [ PubMed : 6789957 ]
- Hon L. U.S. Patent 8393331 B2 Electronic Atomization Cigarette, 2013; < https://docs .google.com /viewer?url=patentimages .storage.googleapis .com/pdfs/US8393331.pdf >; accessed: November 2, 2015.
- Horn D. [Memo from Daniel Horn to Surgeon General William Stewart regarding meeting of June 1, 1966, on tar-nicotine content of cigarettes]. In: Congressional Record—Senate . 1966. British American Tobacco Collection. Bates No. 105618259–105618266. < http://legacy .library .ucsf.edu/tid/ajd94a99 >.
- Huang J, Kornfield R, Szczypka G, Emery SL. A cross-sectional examination of marketing of electronic cigarettes on Twitter. Tobacco Control 2014;23:(Suppl 3):iii26–iii30. [ PMC free article : PMC4078681 ] [ PubMed : 24935894 ]
- Hughes JR. Effects of abstinence from tobacco: valid symptoms and time course. Nicotine & Tobacco Research 2007;9(3):315–27 [ PubMed : 17365764 ]
- Japan Tobacco Inc. JT acquires leading e-cigarette brand E-Lites, 2014; < http://www .jti.com/media /news-releases/jt-acquires-leading-e-cigarette-brand-e-lites >; accessed: July 10, 2015.
- Japan Tobacco Inc. JTI acquires “Ploom” intel-lectual property rights from Ploom, Inc., 2015; < http://www .jti.com/media /news-releases/jti-acquires-ploom-intellectual-property-rights-ploom-inc >; accessed: July 10, 2015.
- Jarvis MJ, Boreham R, Primatesta P, Feyerabend C, Bryant A. Nicotine yield from machine-smoked cigarettes and nicotine intakes in smokers: evidence from a representative population survey. Journal of the National Cancer Institute 2001;93(2):134–8. [ PubMed : 11208883 ]
- Joseph AM, Hennrikus D, Thoele MJ, Krueger R, Hatsukami D. Community tobacco control leaders’ perceptions of harm reduction. Tobacco Control 2004;13(2):108–13. [ PMC free article : PMC1747850 ] [ PubMed : 15175521 ]
- Kim AE, Arnold KY, Makarenko O. E-cigarette advertising expenditures in the U.S., 2011–2012. American Journal of Preventive Medicine 2014;46(4):409–12. [ PubMed : 24650844 ]
- King BA, Alam S, Promoff G, Arrazola R, Dube SR. Awareness and ever use of electronic cigarettes among U.S. adults, 2010–2011. Nicotine & Tobacco Research 2013;15(9):1623–7. [ PMC free article : PMC4570561 ] [ PubMed : 23449421 ]
- Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine & Tobacco Research 2015;17(7):847–54. [ PMC free article : PMC4674436 ] [ PubMed : 25481917 ]
- Kosmider L, Sobczak A, Fik M, Knysak J, Zaciera M, Kurek J, Goniewicz ML. Carbonyl compounds in electronic cigarette vapors: effects of nicotine solvent and battery output voltage. Nicotine & Tobacco Research 2014;16(10):1319–26. [ PMC free article : PMC4838028 ] [ PubMed : 24832759 ]
- Kostygina G, Glantz SA, Ling PM. Tobacco industry use of flavours to recruit new users of little cigars and cigarillos. Tobacco Control 2014. [ PMC free article : PMC4414663 ] [ PubMed : 25354674 ]
- Krishnan-Sarin S, Morean ME, Camenga DR, Cavallo DA, Kong G. E-cigarette use among high school and middle school adolescents in Connecticut. Nicotine & Tobacco Research 2015;17(7):810–8. [ PMC free article : PMC4674435 ] [ PubMed : 25385873 ]
- Lempert LK, Grana R, Glantz SA. The importance of product definitions in U.S. e-cigarette laws and regulations. Tobacco Control 2016;25(e1):e44–e51. [ PMC free article : PMC4466213 ] [ PubMed : 25512432 ]
- Ling PM, Glantz SA. Tobacco industry consumer research on socially acceptable cigarettes Tobacco Control 2005;14(5):e3–e3. [ PMC free article : PMC1748101 ] [ PubMed : 16183968 ]
- Marini S, Buonanno G, Stabile L, Ficco G. Short-term effects of electronic and tobacco cigarettes on exhaled nitric oxide. Toxicology and Applied Pharmacology 2014;278(1):9–15. [ PubMed : 24732441 ]
- Mohney G. First child’s death from liquid nicotine reported as “vaping” gains popularity, 2014; < http://abcnews .go.com /Health/childs-death-liquid-nicotine-reported-vaping-gains-popularity /story?id=27563788 >.
- Morean ME, Kong G, Camenga DR, Cavallo DA, Krishnan-Sarin S. High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics 2015;136(4):611–6. [ PMC free article : PMC4586732 ] [ PubMed : 26347431 ]
- National Association of Tobacco Outlets, Inc. v. City of Providence , 731 F.3d 71, 83 (1st Cir. 2013).
- National Cancer Institute. The FTC Cigarette Test Method for Determining Tar, Nicotine, and Carbon Monoxide Yields of U.S. Cigarettes . Smoking and Tobacco Control Monograph No. 7. Bethesda (MD): U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute, 1996.
- National Cancer Institute. Risks Associated With Smoking Cigarettes With Low Machine-Measured Yields of Tar and Nicotine . Smoking and Tobacco Control Monograph No. 13. Bethesda (MD): U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute, 2001. NIH Publication No. 02-5047.
- Noel JK, Rees VW, Connolly GN. Electronic cigarettes: a new “tobacco” industry? Tobacco Control 2011;20(1):81. [ PubMed : 20930060 ]
- O’Connor RJ, Hyland A, Giovino GA, Fong GT, Cummings KM. Smoker awareness of and beliefs about supposedly less-harmful tobacco products. American Journal of Preventive Medicine 2005;29(2):85–90. [ PubMed : 16005803 ]
- Pankow JF, Strongin RM, Peyton DH. More on hidden formaldehyde in e-cigarette aerosols. New England Journal of Medicine 2015;372(16):1576–7. [ PubMed : 25875273 ]
- Pearson JL, Richardson A, Niaura RS, Vallone DM, Abrams DB. e-Cigarette awareness, use, and harm perceptions in U.S. adults. American Journal of Public Health 2012;102(9):1758–66. [ PMC free article : PMC3474361 ] [ PubMed : 22813087 ]
- Peeler C. Cigarette testing and the Federal Trade Commission: a historical overview. In: The FTC Cigarette Test Method for Determining Nicotine, and Carbon Monoxide Yields for U.S. Cigarettes: Report of the NCI Expert Committee . Tobacco Control Monograph No. 7. Bethesda (MD): U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute, 1996:1–8.
- Philip Morris International. Philip Morris International Inc. (PMI) hosts investor day: revises 2014 full-year reported diluted EPS forecast for estimated restructuring costs in the Netherlands; announces acquisition of U.K.-based e-vapor company; reviews business outlook and strategies, 2014; < http://investors .pmi .com/phoenix.zhtml?c =146476&p=irol-newsArticle&ID=1942860 >; accessed: July 10, 2015.
- Pollay RW, Dewhirst T. The dark side of marketing seemingly “Light” cigarettes: successful images and failed fact. Tobacco Control 2002;11:(Suppl 1):i18–i31. [ PMC free article : PMC1766068 ] [ PubMed : 11893811 ]
- Proctor RN. Golden Holocaust: Origins of the Cigarette Catastrophe and the Case for Abolition . Berkeley (CA): University of California Press, 2011.
- Public Health Law Center. U.S. e-cigarette regulations—50 state review (2015), 2015; < http: //publichealthlawcenter .org/resources /us-e-cigarette-regulations-50-state-review >; accessed: November 3, 2015.
- Regan AK, Promoff G, Dube SR, Arrazola R. Electronic nicotine delivery systems: adult use and awareness of the “e-cigarette” in the U.S.A. Tobacco Control 2013;22(1):19–23. [ PubMed : 22034071 ]
- Richardson A, Ganz O, Vallone D. Tobacco on the web: surveillance and characterisation of online tobacco and e-cigarette advertising. Tobacco Control 2015;24(4):341–7. [ PubMed : 24532710 ]
- Richtel M. E-cigarettes, by other names, lure young and worry experts. New York Times , March 4, 2014; < http://www .nytimes.com /2014/03/05/business /e-cigarettes-under-aliases-elude-the-authorities .html?_r=0 >; accessed: July 27, 2015.
- Russell MAH, Sutton SR, Iyer R, Feyerabend C, Vesey CJ. Long-term switching to low-tar low-nicotine cigarettes. British Journal of Addiction 1982;77(2):145–58. [ PubMed : 6810910 ]
- Saitta D, Ferro GA, Polosa R. Achieving appropriate regulations for electronic cigarettes. Therapeutic Advances in Chronic Disease 2014;5(2):50–61. [ PMC free article : PMC3926346 ] [ PubMed : 24587890 ]
- Sanford Z, Goebel L. E-cigarettes: an up to date review and discussion of the controversy. West Virginia Medical Journal 2014;110(4):10–5. [ PubMed : 25322582 ]
- Schauer GL, King BA, Bunnell RE, Promoff G, McAfee TA. Toking, vaping, and eating for health or fun: marijuana use patterns in adults, U.S., 2014. American Journal of Preventive Medicine 2016;50(1):1–8. [ PubMed : 26277652 ]
- Schweitzer KS, Chen SX, Law S, Van Demark M, Poirier C, Justice MJ, Hubbard WC, Kim ES, Lai X, Wang M, et al. Endothelial disruptive proinflammatory effects of nicotine and e-cigarette vapor exposures. American Journal of Physiology: Lung Cellular and Molecular Physiology 2015;309(2):L175–87. [ PMC free article : PMC4504977 ] [ PubMed : 25979079 ]
- Slade J, Ballin S. Who’s minding the tobacco store? It’s time to level the regulatory playing field. In: Houston T, editor. Tobacco Use: An American Crisis. Final Conference Report and Recommendations from America’s Health Community . Washington (DC): American Medical Association, 1993:52–8.
- Smoking Everywhere, Inc. and Sottera, Inc., d/b/a NJOY v. U.S. Food and Drug Administration , et al., 680 F. Supp. 2d 62 (D.C. 2010).
- Sottera, Inc. v. Food and Drug Administration , No. 627 F.3d 891 (D.C. Cir. 2010).
- Stratton K, Shetty P, Wallace R, Bondurant S, editors. Clearing the Smoke: Assessing the Science Base for Tobacco Harm Reduction . Washington (DC): National Academies Press, 2001. [ PubMed : 25057541 ]
- Thun MJ, Burns DM. Health impact of “reduced yield” cigarettes: a critical assessment of the epidemiological evidence. Tobacco Control 2001;10:(Suppl 1):i4–i11. [ PMC free article : PMC1766045 ] [ PubMed : 11740038 ]
- Tindall JE. Cigarette Market History and Interpretation and Consumer Research . 1992. Philip Morris Collection. Bates No. 2057041153–2057041196. < https://www .industrydocumentslibrary .ucsf .edu/tobacco/docs/glbn0130 >.
- U.S. Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service . Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Center for Disease Control, 1964. PHS Publication No. 1103.
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: The Changing Cigarette. A Report of the Surgeon General . Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Office on Smoking and Health, 1981. DHHS Publication No. (PHS) 81-50156.
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: Nicotine Addiction. A Report of the Surgeon General . Atlanta (GA): U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 1988. DHHS Publication No. (CDC) 88-8406.
- U.S. Department of Health and Human Services. Preventing Tobacco Use Among Young People: A Report of the Surgeon General . Atlanta (GA): U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 1994.
- U.S. Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General . Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2012. [ PubMed : 22876391 ]
- U.S. Department of Health and Human Services. Smoking—50 Years of Progress: A Report of the Surgeon General . Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014.
- U.S. Fire Administration. Electronic Cigarette Fires and Explosions , 2014; < https://www .usfa.fema .gov/downloads/pdf/publications /electronic_cigarettes.pdf >; accessed: July 22, 2015.
- U.S. Food and Drug Administration. Stakeholder letter: regulation of e-cigarettes and other tobacco products, 2011; < http://www .fda.gov/NewsEvents /PublicHealthFocus/ucm252360 .htm >; accessed: May 5, 2015.
- U.S. Food and Drug Administration. Deeming tobacco products to be subject to the Federal Food, Drug, and Cosmetic Act , as amended by the Family Smoking Prevention and Tobacco Control Act , 2016; < http://www .fda.gov/TobaccoProducts /Labeling /RulesRegulationsGuidance/ucm394909 .htm >; accessed: May 16, 2016. [ PubMed : 27192730 ]
- U.S. Food and Drug Administration. E-cigarette adverse events, 2013; < http://www .fda.gov/downloads /AboutFDA/CentersOffices /OfficeofMedicalProductsandTobacco /AbouttheCenterforTobaccoProducts /UCM361437.pdf >; accessed: August 23, 2016.
- U.S. Patent No. 8,490,628 B2. Electronic atomization cigarette, 2013; < http://www .google.com/patents/US8490628 >; accessed: July 22, 2015.
- U.S. Smokeless Tobacco Manufacturing Co. v. City of New York , 708 F.3d 428, 434 (2d Cir. 2013).
- United Press International. Company sniffs profits from a smokeless cigarette. Chicago Tribune , May 27, 1986; < http://articles .chicagotribune .com/1986-05-27 /business/8602070938 _1_smokeless-cigarette-tobacco-smoke-nicotine >; accessed: June 22, 2015.
- United States v. Philip Morris , 449 F. Supp. 2d 1 (D.D.C. 2006).
- Vape Ranks. Phillip Morris launches new type of smokeless cigarette, 2014; < http://vaperanks .com /phillip-morris-launches-new-type-of-smokeless-cigarette/ >; accessed: July 10, 2015.
- Wagener TL, Siegel M, Borrelli B. Electronic cigarettes: achieving a balanced perspective. Addiction 2012;107(9):1545–8. [ PubMed : 22471757 ]
- Wang B, King BA, Corey CG, Arrazola RA, Johnson SE. Awareness and use of non-conventional tobacco products among U.S. students, 2012. American Journal of Preventive Medicine 2014;47(2 Suppl 1):S36–S52. [ PMC free article : PMC4519346 ] [ PubMed : 25044194 ]
- Warner KE, Martin EG. The U.S. tobacco control community’s view of the future of tobacco harm reduction. Tobacco Control 2003;12(4):383–90. [ PMC free article : PMC1747785 ] [ PubMed : 14660773 ]
- Wells Fargo Securities. Nielsen: Tobacco “All Channel” Data Cig Pricing Remains Strong; E-Cig $ Sales Growth Re-Accelerates . Equity Research. San Francisco (CA): Wells Fargo Securities, March 31, 2015.
- Whelan R. E-cigarettes maker models supply chain on electronics industry: VMR Products says the Apple Inc. manufacturing strategy will help the company watch its control quality more closely. The Wall Street Journal , June 12, 2015; < http://www .wsj.com/articles /e-cigarettes-maker-models-supply-chain-on-electronics-industry-1434119233 >; accessed: November 3, 2015.
- Yang L, Rudy SF, Cheng JM, Durmowicz EL. Electronic cigarettes: incorporating human factors engineering into risk assessments. Tobacco Control 2014;23:(Suppl 2):ii47–ii53. [ PMC free article : PMC3995290 ] [ PubMed : 24732164 ]
- Zhu SH, Sun JY, Bonnevie E, Cummins SE, Gamst A, Yin L, Lee M. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tobacco Control 2014;23:(Suppl 3):iii3–iii9. [ PMC free article : PMC4078673 ] [ PubMed : 24935895 ]
- Cite this Page National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General [Internet]. Atlanta (GA): Centers for Disease Control and Prevention (US); 2016. Chapter 1, Introduction, Conclusions, and Historical Background Relative to E-Cigarettes.
- PDF version of this title (8.4M)
- Disable Glossary Links
In this Page
Other titles in this collection.
- Publications and Reports of the Surgeon General
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Introduction, Conclusions, and Historical Background Relative to E-Cigarettes - ... Introduction, Conclusions, and Historical Background Relative to E-Cigarettes - E-Cigarette Use Among Youth and Young Adults
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Open access
- Published: 18 May 2021
An updated overview of e-cigarette impact on human health
- Patrice Marques ORCID: orcid.org/0000-0003-0465-1727 1 , 2 ,
- Laura Piqueras ORCID: orcid.org/0000-0001-8010-5168 1 , 2 , 3 &
- Maria-Jesus Sanz ORCID: orcid.org/0000-0002-8885-294X 1 , 2 , 3
Respiratory Research volume 22 , Article number: 151 ( 2021 ) Cite this article
409k Accesses
157 Citations
365 Altmetric
Metrics details
The electronic cigarette ( e-cigarette ), for many considered as a safe alternative to conventional cigarettes, has revolutionised the tobacco industry in the last decades. In e-cigarettes , tobacco combustion is replaced by e-liquid heating, leading some manufacturers to propose that e-cigarettes have less harmful respiratory effects than tobacco consumption. Other innovative features such as the adjustment of nicotine content and the choice of pleasant flavours have won over many users. Nevertheless, the safety of e-cigarette consumption and its potential as a smoking cessation method remain controversial due to limited evidence. Moreover, it has been reported that the heating process itself can lead to the formation of new decomposition compounds of questionable toxicity. Numerous in vivo and in vitro studies have been performed to better understand the impact of these new inhalable compounds on human health. Results of toxicological analyses suggest that e-cigarettes can be safer than conventional cigarettes, although harmful effects from short-term e-cigarette use have been described. Worryingly, the potential long-term effects of e-cigarette consumption have been scarcely investigated. In this review, we take stock of the main findings in this field and their consequences for human health including coronavirus disease 2019 (COVID-19).
Electronic nicotine dispensing systems (ENDS), commonly known as electronic cigarettes or e-cigarettes , have been popularly considered a less harmful alternative to conventional cigarette smoking since they first appeared on the market more than a decade ago. E-cigarettes are electronic devices, essentially consisting of a cartridge, filled with an e-liquid, a heating element/atomiser necessary to heat the e-liquid to create a vapour that can be inhaled through a mouthpiece, and a rechargeable battery (Fig. 1 ) [ 1 , 2 ]. Both the electronic devices and the different e-liquids are easily available in shops or online stores.
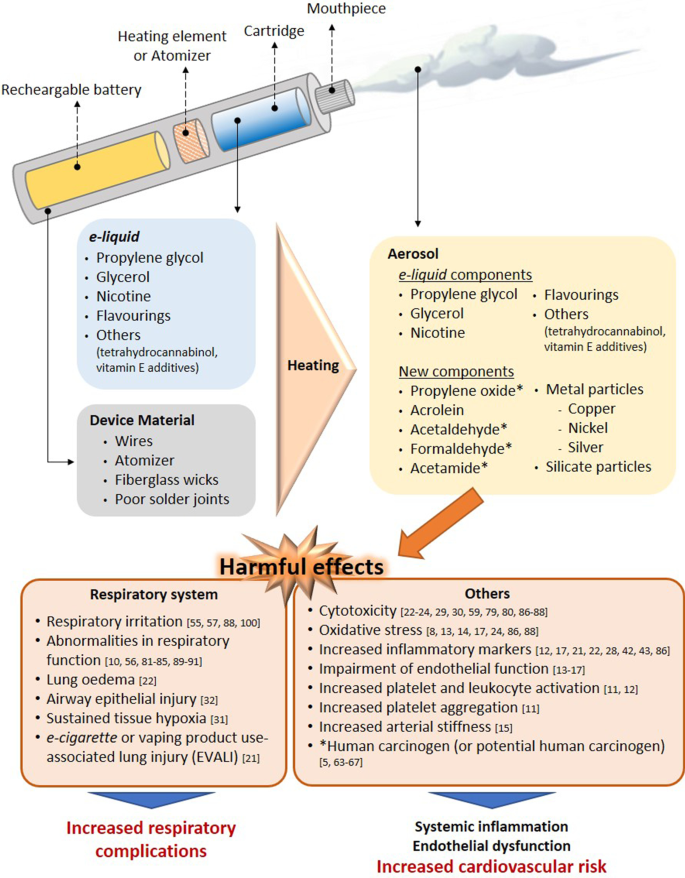
Effect of the heating process on aerosol composition. Main harmful effects documented. Several compounds detected in e-cigarette aerosols are not present in e-liquid s and the device material also seems to contribute to the presence of metal and silicate particles in the aerosols. The heating conditions especially on humectants, flavourings and the low-quality material used have been identified as the generator of the new compounds in aerosols. Some compounds generated from humectants (propylene glycol and glycerol) and flavourings, have been associated with clear airways impact, inflammation, impairment of cardiovascular function and toxicity. In addition, some of them are carcinogens or potential carcinogens
The e-liquid typically contains humectants and flavourings, with or without nicotine; once vapourised by the atomiser, the aerosol (vapour) provides a sensation similar to tobacco smoking, but purportedly without harmful effects [ 3 ]. However, it has been reported that the heating process can lead to the generation of new decomposition compounds that may be hazardous [ 4 , 5 ]. The levels of nicotine, which is the key addictive component of tobacco, can also vary between the commercially available e-liquids, and even nicotine-free options are available. For this particular reason, e-cigarettes are often viewed as a smoking cessation tool, given that those with nicotine can prevent smoking craving, yet this idea has not been fully demonstrated [ 2 , 6 , 7 ].
Because e-cigarettes are combustion-free, and because most of the damaging and well-known effects of tobacco are derived from this reaction, there is a common and widely spread assumption that e-cigarette consumption or “vaping” is safer than conventional cigarette smoking. However, are they risk-free? Is there sufficient toxicological data on all the components employed in e-liquids ? Do we really know the composition of the inhaled vapour during the heating process and its impact on health? Can e-cigarettes be used to curb tobacco use? Do their consumption impact on coronavirus disease 2019 (COVID-19)? In the present review, we have attempted to clarify these questions based on the existing scientific literature, and we have compiled new insights related with the toxicity derived from the use of these devices.
Effect of e-cigarette vapour versus conventional cigarette exposure: in vivo and in vitro effects
Numerous studies have been performed to evaluate the safety/toxicity of e-cigarette use both in vivo and in in vitro cell culture.
One of the first studies in humans involved the analysis of 9 volunteers that consumed e-cigarettes , with or without nicotine, in a ventilated room for 2 h [ 8 ]. Pollutants in indoor air, exhaled nitric oxide (NO) and urinary metabolite profiles were analysed. The results of this acute experiment revealed that e-cigarettes are not emission-free, and ultrafine particles formed from propylene glycol (PG) could be detected in the lungs. The study also suggested that the presence of nicotine in e-cigarettes increased the levels of NO exhaled from consumers and provoked marked airway inflammation; however, no differences were found in the levels of exhaled carbon monoxide (CO), an oxidative stress marker, before and after e-cigarette consumption [ 8 ]. A more recent human study detected significantly higher levels of metabolites of hazardous compounds including benzene, ethylene oxide, acrylonitrile, acrolein and acrylamide in the urine of adolescent dual users ( e-cigarettes and conventional tobacco consumers) than in adolescent e-cigarette -only users (Table 1 ) [ 9 ]. Moreover, the urine levels of metabolites of acrylonitrile, acrolein, propylene oxide, acrylamide and crotonaldehyde, all of which are detrimental for human health, were significantly higher in e-cigarette -only users than in non-smoker controls, reaching up to twice the registered values of those from non-smoker subjects (Table 1 ) [ 9 ]. In line with these observations, dysregulation of lung homeostasis has been documented in non-smokers subjected to acute inhalation of e-cigarette aerosols [ 10 ].
Little is known about the effect of vaping on the immune system. Interestingly, both traditional and e-cigarette consumption by non-smokers was found to provoke short-term effects on platelet function, increasing platelet activation (levels of soluble CD40 ligand and the adhesion molecule P-selectin) and platelet aggregation, although to a lesser extent with e-cigarettes [ 11 ]. As found with platelets, the exposure of neutrophils to e-cigarette aerosol resulted in increased CD11b and CD66b expression being both markers of neutrophil activation [ 12 ]. Additionally, increased oxidative stress, vascular endothelial damage, impaired endothelial function, and changes in vascular tone have all been reported in different human studies on vaping [ 13 , 14 , 15 , 16 , 17 ]. In this context, it is widely accepted that platelet and leukocyte activation as well as endothelial dysfunction are associated with atherogenesis and cardiovascular morbidity [ 18 , 19 ]. In line with these observations the potential association of daily e-cigarettes consumption and the increased risk of myocardial infarction remains controversial but benefits may occur when switching from tobacco to chronic e-cigarette use in blood pressure regulation, endothelial function and vascular stiffness (reviewed in [ 20 ]). Nevertheless, whether or not e-cigarette vaping has cardiovascular consequences requires further investigation.
More recently, in August 2019, the US Centers for Disease Control and Prevention (CDC) declared an outbreak of the e-cigarette or vaping product use-associated lung injury (EVALI) which caused several deaths in young population (reviewed in [ 20 ]). Indeed, computed tomography (CT scan) revealed local inflammation that impaired gas exchange caused by aerosolised oils from e-cigarettes [ 21 ]. However, most of the reported cases of lung injury were associated with use of e-cigarettes for tetrahydrocannabinol (THC) consumption as well as vitamin E additives [ 20 ] and not necessarily attributable to other e-cigarette components.
On the other hand, in a comparative study of mice subjected to either lab air, e-cigarette aerosol or cigarette smoke (CS) for 3 days (6 h-exposure per day), those exposed to e-cigarette aerosols showed significant increases in interleukin (IL)-6 but normal lung parenchyma with no evidence of apoptotic activity or elevations in IL-1β or tumour necrosis factor-α (TNFα) [ 22 ]. By contrast, animals exposed to CS showed lung inflammatory cell infiltration and elevations in inflammatory marker expression such as IL-6, IL-1β and TNFα [ 22 ]. Beyond airway disease, exposure to aerosols from e-liquids with or without nicotine has also been also associated with neurotoxicity in an early-life murine model [ 23 ].
Results from in vitro studies are in general agreement with the limited number of in vivo studies. For example, in an analysis using primary human umbilical vein endothelial cells (HUVEC) exposed to 11 commercially-available vapours, 5 were found to be acutely cytotoxic, and only 3 of those contained nicotine [ 24 ]. In addition, 5 of the 11 vapours tested (including 4 that were cytotoxic) reduced HUVEC proliferation and one of them increased the production of intracellular reactive oxygen species (ROS) [ 24 ]. Three of the most cytotoxic vapours—with effects similar to those of conventional high-nicotine CS extracts—also caused comparable morphological changes [ 24 ]. Endothelial cell migration is an important mechanism of vascular repair than can be disrupted in smokers due to endothelial dysfunction [ 25 , 26 ]. In a comparative study of CS and e-cigarette aerosols, Taylor et al . found that exposure of HUVEC to e-cigarette aqueous extracts for 20 h did not affect migration in a scratch wound assay [ 27 ], whereas equivalent cells exposed to CS extract showed a significant inhibition in migration that was concentration dependent [ 27 ].
In cultured human airway epithelial cells, both e-cigarette aerosol and CS extract induced IL-8/CXCL8 (neutrophil chemoattractant) release [ 28 ]. In contrast, while CS extract reduced epithelial barrier integrity (determined by the translocation of dextran from the apical to the basolateral side of the cell layer), e-cigarette aerosol did not, suggesting that only CS extract negatively affected host defence [ 28 ]. Moreover, Higham et al . also found that e-cigarette aerosol caused IL-8/CXCL8 and matrix metallopeptidase 9 (MMP-9) release together with enhanced activity of elastase from neutrophils [ 12 ] which might facilitate neutrophil migration to the site of inflammation [ 12 ].
In a comparative study, repeated exposure of human gingival fibroblasts to CS condensate or to nicotine-rich or nicotine-free e-vapour condensates led to alterations in morphology, suppression of proliferation and induction of apoptosis, with changes in all three parameters greater in cells exposed to CS condensate [ 29 ]. Likewise, both e-cigarette aerosol and CS extract increased cell death in adenocarcinomic human alveolar basal epithelial cells (A549 cells), and again the effect was more damaging with CS extract than with e-cigarette aerosol (detrimental effects found at 2 mg/mL of CS extract vs. 64 mg/mL of e-cigarette extract) [ 22 ], which is in agreement with another study examining battery output voltage and cytotoxicity [ 30 ].
All this evidence would suggest that e-cigarettes are potentially less harmful than conventional cigarettes (Fig. 2 ) [ 11 , 14 , 22 , 24 , 27 , 28 , 29 ]. Importantly, however, most of these studies have investigated only short-term effects [ 10 , 14 , 15 , 22 , 27 , 28 , 29 , 31 , 32 ], and the long-term effects of e-cigarette consumption on human health are still unclear and require further study.
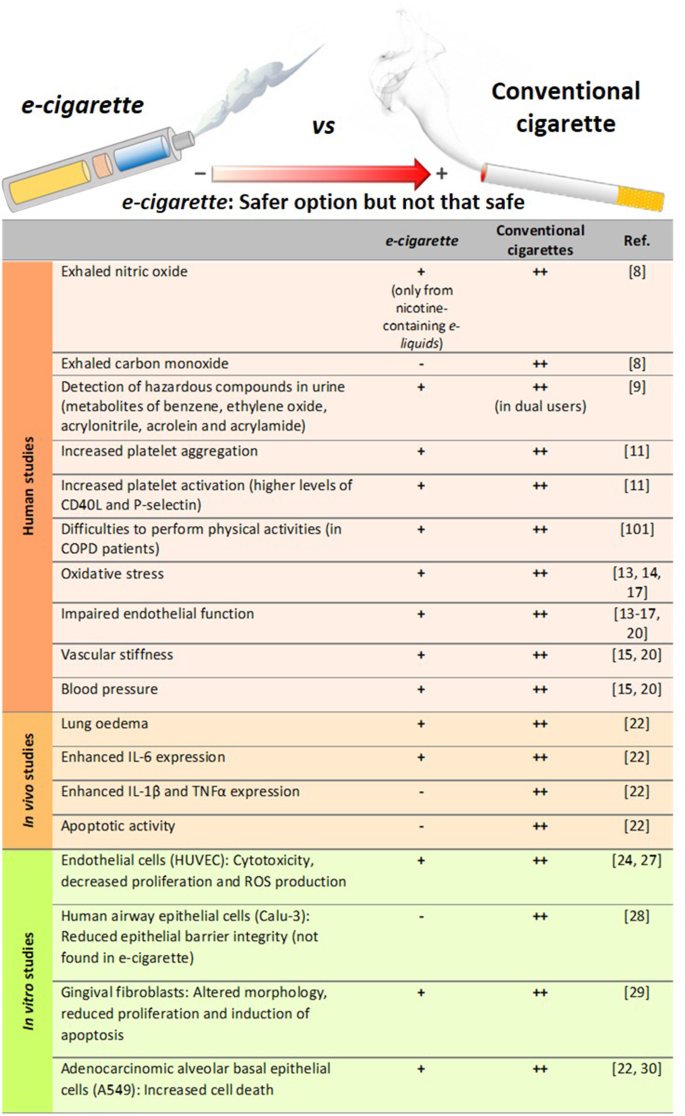
Comparison of the degree of harmful effects documented from e-cigarette and conventional cigarette consumption. Human studies, in vivo mice exposure and in vitro studies. All of these effects from e-cigarettes were documented to be lower than those exerted by conventional cigarettes, which may suggest that e-cigarette consumption could be a safer option than conventional tobacco smoking but not a clear safe choice
Consequences of nicotine content
Beyond flavour, one of the major issues in the e-liquid market is the range of nicotine content available. Depending on the manufacturer, the concentration of this alkaloid can be presented as low , medium or high , or expressed as mg/mL or as a percentage (% v/v). The concentrations range from 0 (0%, nicotine-free option) to 20 mg/mL (2.0%)—the maximum nicotine threshold according to directive 2014/40/EU of the European Parliament and the European Union Council [ 33 , 34 ]. Despite this normative, however, some commercial e-liquids have nicotine concentrations close to 54 mg/mL [ 35 ], much higher than the limits established by the European Union.
The mislabelling of nicotine content in e-liquids has been previously addressed [ 8 , 34 ]. For instance, gas chromatography with a flame ionisation detector (GC-FID) revealed inconsistencies in the nicotine content with respect to the manufacturer´s declaration (average of 22 ± 0.8 mg/mL vs. 18 mg/mL) [ 8 ], which equates to a content ~ 22% higher than that indicated in the product label. Of note, several studies have detected nicotine in those e-liquids labelled as nicotine-free [ 5 , 35 , 36 ]. One study detected the presence of nicotine (0.11–6.90 mg/mL) in 5 of 23 nicotine-free labelled e-liquids by nuclear magnetic resonance spectroscopy [ 35 ], and another study found nicotine (average 8.9 mg/mL) in 13.6% (17/125) of the nicotine-free e-liquids as analysed by high performance liquid chromatography (HPLC) [ 36 ]. Among the 17 samples tested in this latter study 14 were identified to be counterfeit or suspected counterfeit. A third study detected nicotine in 7 of 10 nicotine-free refills, although the concentrations were lower than those identified in the previous analyses (0.1–15 µg/mL) [ 5 ]. Not only is there evidence of mislabelling of nicotine content among refills labelled as nicotine-free, but there also seems to be a history of poor labelling accuracy in nicotine-containing e-liquids [ 37 , 38 ].
A comparison of the serum levels of nicotine from e-cigarette or conventional cigarette consumption has been recently reported [ 39 ]. Participants took one vape from an e-cigarette , with at least 12 mg/mL of nicotine, or inhaled a conventional cigarette, every 20 s for 10 min. Blood samples were collected 1, 2, 4, 6, 8, 10, 12 and 15 min after the first puff, and nicotine serum levels were measured by liquid chromatography-mass spectrometry (LC–MS). The results revealed higher serum levels of nicotine in the conventional CS group than in the e-cigarette group (25.9 ± 16.7 ng/mL vs. 11.5 ± 9.8 ng/mL). However, e-cigarettes containing 20 mg/mL of nicotine are more equivalent to normal cigarettes, based on the delivery of approximately 1 mg of nicotine every 5 min [ 40 ].
In this line, a study compared the acute impact of CS vs. e-cigarette vaping with equivalent nicotine content in healthy smokers and non-smokers. Both increased markers of oxidative stress and decreased NO bioavailability, flow-mediated dilation, and vitamin E levels showing no significant differences between tobacco and e-cigarette exposure (reviewed in [ 20 ]). Inasmuch, short-term e-cigarette use in healthy smokers resulted in marked impairment of endothelial function and an increase in arterial stiffness (reviewed in [ 20 ]). Similar effects on endothelial dysfunction and arterial stiffness were found in animals when they were exposed to e-cigarette vapor either for several days or chronically (reviewed in [ 20 ]). In contrast, other studies found acute microvascular endothelial dysfunction, increased oxidative stress and arterial stiffness in smokers after exposure to e-cigarettes with nicotine, but not after e-cigarettes without nicotine (reviewed in [ 20 ]). In women smokers, a study found a significant difference in stiffness after smoking just one tobacco cigarette, but not after use of e-cigarettes (reviewed in [ 20 ]).
It is well known that nicotine is extremely addictive and has a multitude of harmful effects. Nicotine has significant biologic activity and adversely affects several physiological systems including the cardiovascular, respiratory, immunological and reproductive systems, and can also compromise lung and kidney function [ 41 ]. Recently, a sub-chronic whole-body exposure of e-liquid (2 h/day, 5 days/week, 30 days) containing PG alone or PG with nicotine (25 mg/mL) to wild type (WT) animals or knockout (KO) mice in α7 nicotinic acetylcholine receptor (nAChRα7-KO) revealed a partly nAChRα7-dependent lung inflammation [ 42 ]. While sub-chronic exposure to PG/nicotine promote nAChRα7-dependent increased levels of different cytokines and chemokines in the bronchoalveolar lavage fluid (BALF) such as IL-1α, IL-2, IL-9, interferon γ (IFNγ), granulocyte-macrophage colony-stimulating factor (GM-CSF), monocyte chemoattractant protein-1 (MCP-1/CCL2) and regulated on activation, normal T cell expressed and secreted (RANTES/CCL5), the enhanced levels of IL-1β, IL-5 and TNFα were nAChRα7 independent. In general, most of the cytokines detected in BALF were significantly increased in WT mice exposed to PG with nicotine compared to PG alone or air control [ 42 ]. Some of these effects were found to be through nicotine activation of NF-κB signalling albeit in females but not in males. In addition, PG with nicotine caused increased macrophage and CD4 + /CD8 + T-lymphocytes cell counts in BALF compared to air control, but these effects were ameliorated when animals were sub-chronically exposed to PG alone [ 42 ].
Of note, another study indicated that although RANTES/CCL5 and CCR1 mRNA were upregulated in flavour/nicotine-containing e-cigarette users, vaping flavour and nicotine-less e-cigarettes did not significantly dysregulate cytokine and inflammasome activation [ 43 ].
In addition to its toxicological effects on foetus development, nicotine can disrupt brain development in adolescents and young adults [ 44 , 45 , 46 ]. Several studies have also suggested that nicotine is potentially carcinogenic (reviewed in [ 41 ]), but more work is needed to prove its carcinogenicity independently of the combustion products of tobacco [ 47 ]. In this latter regard, no differences were encountered in the frequency of tumour appearance in rats subjected to long-term (2 years) inhalation of nicotine when compared with control rats [ 48 ]. Despite the lack of carcinogenicity evidence, it has been reported that nicotine promotes tumour cell survival by decreasing apoptosis and increasing proliferation [ 49 ], indicating that it may work as a “tumour enhancer”. In a very recent study, chronic administration of nicotine to mice (1 mg/kg every 3 days for a 60-day period) enhanced brain metastasis by skewing the polarity of M2 microglia, which increases metastatic tumour growth [ 50 ]. Assuming that a conventional cigarette contains 0.172–1.702 mg of nicotine [ 51 ], the daily nicotine dose administered to these animals corresponds to 40–400 cigarettes for a 70 kg-adult, which is a dose of an extremely heavy smoker. We would argue that further studies with chronic administration of low doses of nicotine are required to clearly evaluate its impact on carcinogenicity.
In the aforementioned study exposing human gingival fibroblasts to CS condensate or to nicotine-rich or nicotine-free e-vapour condensates [ 29 ], the detrimental effects were greater in cells exposed to nicotine-rich condensate than to nicotine-free condensate, suggesting that the possible injurious effects of nicotine should be considered when purchasing e-refills . It is also noteworthy that among the 3 most cytotoxic vapours for HUVEC evaluated in the Putzhammer et al . study, 2 were nicotine-free, which suggests that nicotine is not the only hazardous component in e-cigarettes [ 24 ] .
The lethal dose of nicotine for an adult is estimated at 30–60 mg [ 52 ]. Given that nicotine easily diffuses from the dermis to the bloodstream, acute nicotine exposure by e-liquid spilling (5 mL of a 20 mg/mL nicotine-containing refill is equivalent to 100 mg of nicotine) can easily be toxic or even deadly [ 8 ]. Thus, devices with rechargeable refills are another issue of concern with e-cigarettes , especially when e-liquids are not sold in child-safe containers, increasing the risk of spilling, swallowing or breathing.
These data overall indicate that the harmful effects of nicotine should not be underestimated. Despite the established regulations, some inaccuracies in nicotine content labelling remain in different brands of e-liquids . Consequently, stricter regulation and a higher quality control in the e-liquid industry are required.
Effect of humectants and their heating-related products
In this particular aspect, again the composition of the e-liquid varies significantly among different commercial brands [ 4 , 35 ]. The most common and major components of e-liquids are PG or 1,2-propanediol, and glycerol or glycerine (propane-1,2,3-triol). Both types of compounds are used as humectants to prevent the e-liquid from drying out [ 2 , 53 ] and are classified by the Food and Drug Administration (FDA) as “Generally Recognised as Safe” [ 54 ]. In fact, they are widely used as alimentary and pharmaceutical products [ 2 ]. In an analysis of 54 commercially available e-liquids , PG and glycerol were detected in almost all samples at concentrations ranging from 0.4% to 98% (average 57%) and from 0.3% to 95% (average 37%), respectively [ 35 ].
With regards to toxicity, little is known about the effects of humectants when they are heated and chronically inhaled. Studies have indicated that PG can induce respiratory irritation and increase the probability of asthma development [ 55 , 56 ], and both PG and glycerol from e-cigarettes might reach concentrations sufficiently high to potentially cause irritation of the airways [ 57 ]. Indeed, the latter study established that one e-cigarette puff results in a PG exposure of 430–603 mg/m 3 , which is higher than the levels reported to cause airway irritation (average 309 mg/m 3 ) based on a human study [ 55 ]. The same study established that one e-cigarette puff results in a glycerol exposure of 348–495 mg/m 3 [ 57 ], which is close to the levels reported to cause airway irritation in rats (662 mg/m 3 ) [ 58 ].
Airway epithelial injury induced by acute vaping of PG and glycerol aerosols (50:50 vol/vol), with or without nicotine, has been reported in two randomised clinical trials in young tobacco smokers [ 32 ]. In vitro, aerosols from glycerol only-containing refills showed cytotoxicity in A549 and human embryonic stem cells, even at a low battery output voltage [ 59 ]. PG was also found to affect early neurodevelopment in a zebrafish model [ 60 ]. Another important issue is that, under heating conditions PG can produce acetaldehyde or formaldehyde (119.2 or 143.7 ng/puff at 20 W, respectively, on average), while glycerol can also generate acrolein (53.0, 1000.0 or 5.9 ng/puff at 20 W, respectively, on average), all carbonyls with a well-documented toxicity [ 61 ]. Although, assuming 15 puffs per e-cigarette unit, carbonyls produced by PG or glycerol heating would be below the maximum levels found in a conventional cigarette combustion (Table 2 ) [ 51 , 62 ]. Nevertheless, further studies are required to properly test the deleterious effects of all these compounds at physiological doses resembling those to which individuals are chronically exposed.
Although PG and glycerol are the major components of e-liquids other components have been detected. When the aerosols of 4 commercially available e-liquids chosen from a top 10 list of “ Best E-Cigarettes of 2014” , were analysed by gas chromatography-mass spectrometry (GC–MS) after heating, numerous compounds were detected, with nearly half of them not previously identified [ 4 ], thus suggesting that the heating process per se generates new compounds of unknown consequence. Of note, the analysis identified formaldehyde, acetaldehyde and acrolein [ 4 ], 3 carbonyl compounds with known high toxicity [ 63 , 64 , 65 , 66 , 67 ]. While no information was given regarding formaldehyde and acetaldehyde concentrations, the authors calculated that one puff could result in an acrolein exposure of 0.003–0.015 μg/mL [ 4 ]. Assuming 40 mL per puff and 15 puffs per e-cigarette unit (according to several manufacturers) [ 4 ], each e-cigarette unit would generate approximately 1.8–9 μg of acrolein, which is less than the levels of acrolein emitted by a conventional tobacco cigarette (18.3–98.2 μg) [ 51 ]. However, given that e-cigarette units of vaping are not well established, users may puff intermittently throughout the whole day. Thus, assuming 400 to 500 puffs per cartridge, users could be exposed to up to 300 μg of acrolein.
In a similar study, acrolein was found in 11 of 12 aerosols tested, with a similar content range (approximately 0.07–4.19 μg per e-cigarette unit) [ 68 ]. In the same study, both formaldehyde and acetaldehyde were detected in all of the aerosols tested, with contents of 0.2–5.61 μg and 0.11–1.36 μg, respectively, per e-cigarette unit [ 68 ]. It is important to point out that the levels of these toxic products in e-cigarette aerosols are significantly lower than those found in CS: 9 times lower for formaldehyde, 450 times lower for acetaldehyde and 15 times lower for acrolein (Table 2 ) [ 62 , 68 ].
Other compounds that have been detected in aerosols include acetamide, a potential human carcinogen [ 5 ], and some aldehydes [ 69 ], although their levels were minimal. Interestingly, the existence of harmful concentrations of diethylene glycol, a known cytotoxic agent, in e-liquid aerosols is contentious with some studies detecting its presence [ 4 , 68 , 70 , 71 , 72 ], and others finding low subtoxic concentrations [ 73 , 74 ]. Similar observations were reported for the content ethylene glycol. In this regard, either it was detected at concentrations that did not exceed the authorised limit [ 73 ], or it was absent from the aerosols produced [ 4 , 71 , 72 ]. Only one study revealed its presence at high concentration in a very low number of samples [ 5 ]. Nevertheless, its presence above 1 mg/g is not allowed by the FDA [ 73 ]. Figure 1 lists the main compounds detected in aerosols derived from humectant heating and their potential damaging effects. It would seem that future studies should analyse the possible toxic effects of humectants and related products at concentrations similar to those that e-cigarette vapers are exposed to reach conclusive results.
Impact of flavouring compounds
The range of e-liquid flavours available to consumers is extensive and is used to attract both current smokers and new e-cigarette users, which is a growing public health concern [ 6 ]. In fact, over 5 million middle- and high-school students were current users of e-cigarettes in 2019 [ 75 ], and appealing flavours have been identified as the primary reason for e-cigarette consumption in 81% of young users [ 76 ]. Since 2016, the FDA regulates the flavours used in the e-cigarette market and has recently published an enforcement policy on unauthorised flavours, including fruit and mint flavours, which are more appealing to young users [ 77 ]. However, the long-term effects of all flavour chemicals used by this industry (which are more than 15,000) remain unknown and they are not usually included in the product label [ 78 ]. Furthermore, there is no safety guarantee since they may harbour potential toxic or irritating properties [ 5 ].
With regards to the multitude of available flavours, some have demonstrated cytotoxicity [ 59 , 79 ]. Bahl et al. evaluated the toxicity of 36 different e-liquids and 29 different flavours on human embryonic stem cells, mouse neural stem cells and human pulmonary fibroblasts using a metabolic activity assay. In general, those e-liquids that were bubblegum-, butterscotch- and caramel-flavoured did not show any overt cytotoxicity even at the highest dose tested. By contrast, those e-liquids with Freedom Smoke Menthol Arctic and Global Smoke Caramel flavours had marked cytotoxic effects on pulmonary fibroblasts and those with Cinnamon Ceylon flavour were the most cytotoxic in all cell lines [ 79 ]. A further study from the same group [ 80 ] revealed that high cytotoxicity is a recurrent feature of cinnamon-flavoured e-liquids. In this line, results from GC–MS and HPLC analyses indicated that cinnamaldehyde (CAD) and 2-methoxycinnamaldehyde, but not dipropylene glycol or vanillin, were mainly responsible for the high cytotoxicity of cinnamon-flavoured e-liquids [ 80 ]. Other flavouring-related compounds that are associated with respiratory complications [ 81 , 82 , 83 ], such as diacetyl, 2,3-pentanedione or acetoin, were found in 47 out of 51 aerosols of flavoured e-liquids tested [ 84 ] . Allen et al . calculated an average of 239 μg of diacetyl per cartridge [ 84 ]. Assuming again 400 puffs per cartridge and 40 mL per puff, is it is possible to estimate an average of 0.015 ppm of diacetyl per puff, which could compromise normal lung function in the long-term [ 85 ].
The cytotoxic and pro-inflammatory effects of different e-cigarette flavouring chemicals were also tested on two human monocytic cell lines—mono mac 6 (MM6) and U937 [ 86 ]. Among the flavouring chemicals tested, CAD was found to be the most toxic and O-vanillin and pentanedione also showed significant cytotoxicity; by contrast, acetoin, diacetyl, maltol, and coumarin did not show any toxicity at the concentrations assayed (10–1000 µM). Of interest, a higher toxicity was evident when combinations of different flavours or mixed equal proportions of e-liquids from 10 differently flavoured e-liquids were tested, suggesting that vaping a single flavour is less toxic than inhaling mixed flavours [ 86 ]. Also, all the tested flavours produced significant levels of ROS in a cell-free ROS production assay. Finally, diacetyl, pentanedione, O-vanillin, maltol, coumarin, and CAD induced significant IL-8 secretion from MM6 and U937 monocytes [ 86 ]. It should be borne in mind, however, that the concentrations assayed were in the supra-physiological range and it is likely that, once inhaled, these concentrations are not reached in the airway space. Indeed, one of the limitations of the study was that human cells are not exposed to e-liquids per se, but rather to the aerosols where the concentrations are lower [ 86 ]. In this line, the maximum concentration tested (1000 µM) would correspond to approximately 80 to 150 ppm, which is far higher than the levels found in aerosols of some of these compounds [ 84 ]. Moreover, on a day-to-day basis, lungs of e-cigarette users are not constantly exposed to these chemicals for 24 h at these concentrations. Similar limitations were found when five of seven flavourings were found to cause cytotoxicity in human bronchial epithelial cells [ 87 ].
Recently, a commonly commercialized crème brûlée -flavoured aerosol was found to contain high concentrations of benzoic acid (86.9 μg/puff), a well-established respiratory irritant [ 88 ]. When human lung epithelial cells (BEAS-2B and H292) were exposed to this aerosol for 1 h, a marked cytotoxicity was observed in BEAS-2B but not in H292 cells, 24 h later. However, increased ROS production was registered in H292 cells [ 88 ].
Therefore, to fully understand the effects of these compounds, it is relevant the cell cultures selected for performing these assays, as well as the use of in vivo models that mimic the real-life situation of chronic e-cigarette vapers to clarify their impact on human health.
The e-cigarette device
While the bulk of studies related to the impact of e-cigarette use on human health has focused on the e-liquid components and the resulting aerosols produced after heating, a few studies have addressed the material of the electronic device and its potential consequences—specifically, the potential presence of metals such as copper, nickel or silver particles in e-liquids and aerosols originating from the filaments and wires and the atomiser [ 89 , 90 , 91 ].
Other important components in the aerosols include silicate particles from the fiberglass wicks or silicone [ 89 , 90 , 91 ]. Many of these products are known to cause abnormalities in respiratory function and respiratory diseases [ 89 , 90 , 91 ], but more in-depth studies are required. Interestingly, the battery output voltage also seems to have an impact on the cytotoxicity of the aerosol vapours, with e-liquids from a higher battery output voltage showing more toxicity to A549 cells [ 30 ].
A recent study compared the acute effects of e-cigarette vapor (with PG/vegetable glycerine plus tobacco flavouring but without nicotine) generated from stainless‐steel atomizer (SS) heating element or from a nickel‐chromium alloy (NC) [ 92 ]. Some rats received a single e-cigarette exposure for 2 h from a NC heating element (60 or 70 W); other rats received a similar exposure of e-cigarette vapor using a SS heating element for the same period of time (60 or 70 W) and, a final group of animals were exposed for 2 h to air. Neither the air‐exposed rats nor those exposed to e-cigarette vapor using SS heating elements developed respiratory distress. In contrast, 80% of the rats exposed to e-cigarette vapor using NC heating units developed clinical acute respiratory distress when a 70‐W power setting was employed. Thus, suggesting that operating units at higher than recommended settings can cause adverse effects. Nevertheless, there is no doubt that the deleterious effects of battery output voltage are not comparable to those exerted by CS extracts [ 30 ] (Figs. 1 and 2 ).
E-cigarettes as a smoking cessation tool
CS contains a large number of substances—about 7000 different constituents in total, with sizes ranging from atoms to particulate matter, and with many hundreds likely responsible for the harmful effects of this habit [ 93 ]. Given that tobacco is being substituted in great part by e-cigarettes with different chemical compositions, manufacturers claim that e -cigarette will not cause lung diseases such as lung cancer, chronic obstructive pulmonary disease, or cardiovascular disorders often associated with conventional cigarette consumption [ 3 , 94 ]. However, the World Health Organisation suggests that e-cigarettes cannot be considered as a viable method to quit smoking, due to a lack of evidence [ 7 , 95 ]. Indeed, the results of studies addressing the use of e-cigarettes as a smoking cessation tool remain controversial [ 96 , 97 , 98 , 99 , 100 ]. Moreover, both FDA and CDC are actively investigating the incidence of severe respiratory symptoms associated with the use of vaping products [ 77 ]. Because many e-liquids contain nicotine, which is well known for its powerful addictive properties [ 41 ], e-cigarette users can easily switch to conventional cigarette smoking, avoiding smoking cessation. Nevertheless, the possibility of vaping nicotine-free e-cigarettes has led to the branding of these devices as smoking cessation tools [ 2 , 6 , 7 ].
In a recently published randomised trial of 886 subjects who were willing to quit smoking [ 100 ], the abstinence rate was found to be twice as high in the e-cigarette group than in the nicotine-replacement group (18.0% vs. 9.9%) after 1 year. Of note, the abstinence rate found in the nicotine-replacement group was lower than what is usually expected with this therapy. Nevertheless, the incidence of throat and mouth irritation was higher in the e-cigarette group than in the nicotine-replacement group (65.3% vs. 51.2%, respectively). Also, the participant adherence to the treatment after 1-year abstinence was significantly higher in the e-cigarette group (80%) than in nicotine-replacement products group (9%) [ 100 ].
On the other hand, it is estimated that COPD could become the third leading cause of death in 2030 [ 101 ]. Given that COPD is generally associated with smoking habits (approximately 15 to 20% of smokers develop COPD) [ 101 ], smoking cessation is imperative among COPD smokers. Published data revealed a clear reduction of conventional cigarette consumption in COPD smokers that switched to e-cigarettes [ 101 ]. Indeed, a significant reduction in exacerbations was observed and, consequently, the ability to perform physical activities was improved when data was compared with those non-vapers COPD smokers. Nevertheless, a longer follow-up of these COPD patients is required to find out whether they have quitted conventional smoking or even vaping, since the final goal under these circumstances is to quit both habits.
Based on the current literature, it seems that several factors have led to the success of e-cigarette use as a smoking cessation tool. First, some e-cigarette flavours positively affect smoking cessation outcomes among smokers [ 102 ]. Second, e-cigarettes have been described to improve smoking cessation rate only among highly-dependent smokers and not among conventional smokers, suggesting that the individual degree of nicotine dependence plays an important role in this process [ 97 ]. Third, the general belief of their relative harmfulness to consumers' health compared with conventional combustible tobacco [ 103 ]. And finally, the exposure to point-of-sale marketing of e-cigarette has also been identified to affect the smoking cessation success [ 96 ].
Implication of e-cigarette consumption in COVID-19 time
Different reports have pointed out that smokers and vapers are more vulnerable to SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) infections or more prone to adverse outcomes if they suffer COVID-19 [ 104 ]. However, while a systematic review indicated that cigarette smoking is probably associated with enhanced damage from COVID-19, a meta-analysis did not, yet the latter had several limitations due to the small sample sizes [ 105 ].
Interestingly, most of these reports linking COVID-19 harmful effects with smoking or vaping, are based on their capability of increasing the expression of angiotensin-converting enzyme 2 (ACE2) in the lung. It is well known that ACE2 is the gate for SARS-CoV-2 entrance to the airways [ 106 ] and it is mainly expressed in type 2 alveolar epithelial cells and alveolar macrophages [ 107 ]. To date, most of the studies in this field indicate that current smokers have higher expression of ACE2 in the airways (reviewed by [ 108 ]) than healthy non-smokers [ 109 , 110 ]. However, while a recent report indicated that e-cigarette vaping also caused nicotine-dependent ACE2 up-regulation [ 42 ], others have revealed that neither acute inhalation of e-cigarette vapour nor e-cigarette users had increased lung ACE2 expression regardless nicotine presence in the e-liquid [ 43 , 110 ].
In regard to these contentions, current knowledge suggests that increased ACE2 expression is not necessarily linked to enhanced susceptibility to SARS-CoV-2 infection and adverse outcome. Indeed, elderly population express lower levels of ACE2 than young people and SARS-CoV-2/ACE2 interaction further decreases ACE2 expression. In fact, most of the deaths provoked by COVID-19 took place in people over 60 years old of age [ 111 ]. Therefore, it is plausible that the increased susceptibility to disease progression and the subsequent fatal outcome in this population is related to poor angiotensin 1-7 (Ang-1-7) generation, the main peptide generated by ACE2, and probably to their inaccessibility to its anti-inflammatory effects. Furthermore, it seems that all the efforts towards increasing ACE2 expression may result in a better resolution of the pneumonic process associated to this pandemic disease.
Nevertheless, additional complications associated to COVID-19 are increased thrombotic events and cytokine storm. In the lungs, e-cigarette consumption has been correlated to toxicity, oxidative stress, and inflammatory response [ 32 , 112 ]. More recently, a study revealed that while the use of nicotine/flavour-containing e-cigarettes led to significant cytokine dysregulation and potential inflammasome activation, none of these effects were detected in non-flavoured and non-nicotine-containing e-cigarettes [ 43 ]. Therefore, taken together these observations, e-cigarette use may still be a potent risk factor for severe COVID-19 development depending on the flavour and nicotine content.
In summary, it seems that either smoking or nicotine vaping may adversely impact on COVID-19 outcome. However, additional follow up studies are required in COVID-19 pandemic to clarify the effect of e-cigarette use on lung and cardiovascular complications derived from SARS-CoV-2 infection.
Conclusions
The harmful effects of CS and their deleterious consequences are both well recognised and widely investigated. However, and based on the studies carried out so far, it seems that e-cigarette consumption is less toxic than tobacco smoking. This does not necessarily mean, however, that e-cigarettes are free from hazardous effects. Indeed, studies investigating their long-term effects on human health are urgently required. In this regard, the main additional studies needed in this field are summarized in Table 3 .
The composition of e-liquids requires stricter regulation, as they can be easily bought online and many incidences of mislabelling have been detected, which can seriously affect consumers’ health. Beyond their unknown long-term effects on human health, the extended list of appealing flavours available seems to attract new “never-smokers”, which is especially worrying among young users. Additionally, there is still a lack of evidence of e-cigarette consumption as a smoking cessation method. Indeed, e-cigarettes containing nicotine may relieve the craving for smoking, but not the conventional cigarette smoking habit.
Interestingly, there is a strong difference of opinion on e-cigarettes between countries. Whereas countries such as Brazil, Uruguay and India have banned the sale of e-cigarettes , others such as the United Kingdom support this device to quit smoking. The increasing number of adolescent users and reported deaths in the United States prompted the government to ban the sale of flavoured e-cigarettes in 2020. The difference in opinion worldwide may be due to different restrictions imposed. For example, while no more than 20 ng/mL of nicotine is allowed in the EU, e-liquids with 59 mg/dL are currently available in the United States. Nevertheless, despite the national restrictions, users can easily access foreign or even counterfeit products online.
In regard to COVID-19 pandemic, the actual literature suggests that nicotine vaping may display adverse outcomes. Therefore, follow up studies are necessary to clarify the impact of e-cigarette consumption on human health in SARS-CoV-2 infection.
In conclusion, e-cigarettes could be a good alternative to conventional tobacco cigarettes, with less side effects; however, a stricter sale control, a proper regulation of the industry including flavour restriction, as well as further toxicological studies, including their chronic effects, are warranted.
Availability of data and materials
Not applicable.
Abbreviations
Angiotensin-converting enzyme 2
Angiotensin 1-7
Bronchoalveolar lavage fluid
Cinnamaldehyde
US Centers for Disease Control and Prevention
Carbon monoxide
Chronic obstructive pulmonary disease
Coronavirus disease 2019
Cigarette smoke
Electronic nicotine dispensing systems
e-cigarette or vaping product use-associated lung injury
Food and Drug Administration
Gas chromatography with a flame ionisation detector
Gas chromatography-mass spectrometry
Granulocyte–macrophage colony-stimulating factor
High performance liquid chromatography
Human umbilical vein endothelial cells
Interleukin
Interferon γ
Liquid chromatography-mass spectrometry
Monocyte chemoattractant protein-1
Matrix metallopeptidase 9
α7 Nicotinic acetylcholine receptor
Nickel‐chromium alloy
Nitric oxide
Propylene glycol
Regulated on activation, normal T cell expressed and secreted
Reactive oxygen species
Severe acute respiratory syndrome coronavirus 2
Stainless‐steel atomizer
Tetrahydrocannabinol
Tumour necrosis factor-α
Hiemstra PS, Bals R. Basic science of electronic cigarettes: assessment in cell culture and in vivo models. Respir Res. 2016;17(1):127.
Article PubMed PubMed Central CAS Google Scholar
Bertholon JF, Becquemin MH, Annesi-Maesano I, Dautzenberg B. Electronic cigarettes: a short review. Respiration. 2013;86(5):433–8.
Article CAS PubMed Google Scholar
Rowell TR, Tarran R. Will chronic e-cigarette use cause lung disease? Am J Physiol Lung Cell Mol Physiol. 2015;309(12):L1398–409.
Article CAS PubMed PubMed Central Google Scholar
Herrington JS, Myers C. Electronic cigarette solutions and resultant aerosol profiles. J Chromatogr A. 2015;1418:192–9.
Hutzler C, Paschke M, Kruschinski S, Henkler F, Hahn J, Luch A. Chemical hazards present in liquids and vapors of electronic cigarettes. Arch Toxicol. 2014;88(7):1295–308.
Pokhrel P, Herzog TA, Muranaka N, Fagan P. Young adult e-cigarette users’ reasons for liking and not liking e-cigarettes: a qualitative study. Psychol Health. 2015;30(12):1450–69.
Article PubMed PubMed Central Google Scholar
Harrell PT, Simmons VN, Correa JB, Padhya TA, Brandon TH. Electronic nicotine delivery systems (“e-cigarettes”): review of safety and smoking cessation efficacy. Otolaryngol Head Neck Surg. 2014;151(3):381–93.
Schober W, Szendrei K, Matzen W, Osiander-Fuchs H, Heitmann D, Schettgen T, et al. Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. Int J Hyg Environ Health. 2014;217(6):628–37.
Rubinstein ML, Delucchi K, Benowitz NL, Ramo DE. Adolescent exposure to toxic volatile organic chemicals from E-cigarettes. Pediatrics. 2018;141(4):e20173557.
Article PubMed Google Scholar
Staudt MR, Salit J, Kaner RJ, Hollmann C, Crystal RG. Altered lung biology of healthy never smokers following acute inhalation of E-cigarettes. Respir Res. 2018;19(1):78.
Nocella C, Biondi-Zoccai G, Sciarretta S, Peruzzi M, Pagano F, Loffredo L, et al. Impact of tobacco versus electronic cigarette smoking on platelet function. Am J Cardiol. 2018;122(9):1477–81.
Higham A, Rattray NJW, Dewhurst JA, Trivedi DK, Fowler SJ, Goodacre R, et al. Electronic cigarette exposure triggers neutrophil inflammatory responses. Respir Res. 2016;17(1):56.
Antoniewicz L, Bosson JA, Kuhl J, Abdel-Halim SM, Kiessling A, Mobarrez F, et al. Electronic cigarettes increase endothelial progenitor cells in the blood of healthy volunteers. Atherosclerosis. 2016;255:179–85.
Carnevale R, Sciarretta S, Violi F, Nocella C, Loffredo L, Perri L, et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest. 2016;150(3):606–12.
Vlachopoulos C, Ioakeimidis N, Abdelrasoul M, Terentes-Printzios D, Georgakopoulos C, Pietri P, et al. Electronic cigarette smoking increases aortic stiffness and blood pressure in young smokers. J Am Coll Cardiol. 2016;67(23):2802–3.
Franzen KF, Willig J, Cayo Talavera S, Meusel M, Sayk F, Reppel M, et al. E-cigarettes and cigarettes worsen peripheral and central hemodynamics as well as arterial stiffness: a randomized, double-blinded pilot study. Vasc Med. 2018;23(5):419–25.
Caporale A, Langham MC, Guo W, Johncola A, Chatterjee S, Wehrli FW. Acute effects of electronic cigarette aerosol inhalation on vascular function detected at quantitative MRI. Radiology. 2019;293(1):97–106.
von Hundelshausen P, Schmitt MM. Platelets and their chemokines in atherosclerosis-clinical applications. Front Physiol. 2014;5:294.
Google Scholar
Landmesser U, Hornig B, Drexler H. Endothelial function: a critical determinant in atherosclerosis? Circulation. 2004;109(21 Suppl 1):Ii27-33.
PubMed Google Scholar
Münzel T, Hahad O, Kuntic M, Keaney JF, Deanfield JE, Daiber A. Effects of tobacco cigarettes, e-cigarettes, and waterpipe smoking on endothelial function and clinical outcomes. Eur Heart J. 2020;41:4057–70.
Javelle E. Electronic cigarette and vaping should be discouraged during the new coronavirus SARS-CoV-2 pandemic. Arch Toxicol. 2020;94(6):2261–2.
Husari A, Shihadeh A, Talih S, Hashem Y, El Sabban M, Zaatari G. Acute exposure to electronic and combustible cigarette aerosols: effects in an animal model and in human alveolar cells. Nicotine Tob Res. 2016;18(5):613–9.
Zelikoff JT, Parmalee NL, Corbett K, Gordon T, Klein CB, Aschner M. Microglia activation and gene expression alteration of neurotrophins in the hippocampus following early-life exposure to E-cigarette aerosols in a murine model. Toxicol Sci. 2018;162(1):276–86.
Putzhammer R, Doppler C, Jakschitz T, Heinz K, Forste J, Danzl K, et al. Vapours of US and EU market leader electronic cigarette brands and liquids are cytotoxic for human vascular endothelial cells. PLoS One. 2016;11(6):e0157337.
Bernhard D, Pfister G, Huck CW, Kind M, Salvenmoser W, Bonn GK, et al. Disruption of vascular endothelial homeostasis by tobacco smoke: impact on atherosclerosis. Faseb J. 2003;17(15):2302–4.
Newby DE, Wright RA, Labinjoh C, Ludlam CA, Fox KA, Boon NA, et al. Endothelial dysfunction, impaired endogenous fibrinolysis, and cigarette smoking: a mechanism for arterial thrombosis and myocardial infarction. Circulation. 1999;99(11):1411–5.
Taylor M, Jaunky T, Hewitt K, Breheny D, Lowe F, Fearon IM, et al. A comparative assessment of e-cigarette aerosols and cigarette smoke on in vitro endothelial cell migration. Toxicol Lett. 2017;277:123–8.
Herr C, Tsitouras K, Niederstraßer J, Backes C, Beisswenger C, Dong L, et al. Cigarette smoke and electronic cigarettes differentially activate bronchial epithelial cells. Respir Res. 2020;21(1):67.
Alanazi H, Park HJ, Chakir J, Semlali A, Rouabhia M. Comparative study of the effects of cigarette smoke and electronic cigarettes on human gingival fibroblast proliferation, migration and apoptosis. Food Chem Toxicol. 2018;118:390–8.
Otreba M, Kosmider L. E-cigarettes: voltage- and concentration-dependent loss in human lung adenocarcinoma viability. J Appl Toxicol. 2018;38(8):1135–43.
Chaumont M, Bernard A, Pochet S, Melot C, El Khattabi C, Reye F, et al. High-wattage E-cigarettes induce tissue hypoxia and lower airway injury: a randomized clinical trial. Am J Respir Crit Care Med. 2018;198(1):123–6.
Chaumont M, van de Borne P, Bernard A, Van Muylem A, Deprez G, Ullmo J, et al. Fourth generation e-cigarette vaping induces transient lung inflammation and gas exchange disturbances: results from two randomized clinical trials. Am J Physiol Lung Cell Mol Physiol. 2019;316(5):L705–19.
European Parliament and the council of the European Union. Directive 2014/40/EU. 2014 (updated April 29, 2014). https://ec.europa.eu/health//sites/health/files/tobacco/docs/dir_201440_en.pdf . Accessed 17 April 2020.
Cameron JM, Howell DN, White JR, Andrenyak DM, Layton ME, Roll JM. Variable and potentially fatal amounts of nicotine in e-cigarette nicotine solutions. Tob Control. 2014;23(1):77–8.
Hahn J, Monakhova YB, Hengen J, Kohl-Himmelseher M, Schussler J, Hahn H, et al. Electronic cigarettes: overview of chemical composition and exposure estimation. Tob Induc Dis. 2014;12(1):23.
Omaiye EE, Cordova I, Davis B, Talbot P. Counterfeit electronic cigarette products with mislabeled nicotine concentrations. Tob Regul Sci. 2017;3(3):347–57.
Buettner-Schmidt K, Miller DR, Balasubramanian N. Electronic cigarette refill liquids: child-resistant packaging, nicotine content, and sales to minors. J Pediatr Nurs. 2016;31(4):373–9.
Jackson R, Huskey M, Brown S. Labelling accuracy in low nicotine e-cigarette liquids from a sampling of US manufacturers. Int J Pharm Pract. 2019;28(3):290–4.
Yingst JM, Foulds J, Veldheer S, Hrabovsky S, Trushin N, Eissenberg TT, et al. Nicotine absorption during electronic cigarette use among regular users. PLoS One. 2019;14(7):e0220300.
Farsalinos KE, Romagna G, Tsiapras D, Kyrzopoulos S, Voudris V. Evaluation of electronic cigarette use (vaping) topography and estimation of liquid consumption: implications for research protocol standards definition and for public health authorities’ regulation. Int J Environ Res Public Health. 2013;10(6):2500–14.
Mishra A, Chaturvedi P, Datta S, Sinukumar S, Joshi P, Garg A. Harmful effects of nicotine. Indian J Med Paediatr Oncol. 2015;36(1):24–31.
Wang Q, Sundar IK, Li D, Lucas JH, Muthumalage T, McDonough SR, et al. E-cigarette-induced pulmonary inflammation and dysregulated repair are mediated by nAChR α7 receptor: role of nAChR α7 in SARS-CoV-2 Covid-19 ACE2 receptor regulation. Respir Res. 2020;21(1):154.
Lee AC, Chakladar J, Li WT, Chen C, Chang EY, Wang-Rodriguez J, et al. Tobacco, but not nicotine and flavor-less electronic cigarettes, induces ACE2 and immune dysregulation. Int J Mol Sci. 2020;21(15):5513.
Article CAS PubMed Central Google Scholar
England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA. Nicotine and the developing human: a neglected element in the electronic cigarette debate. Am J Prev Med. 2015;49(2):286–93.
Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain. J Physiol. 2015;593(16):3397–412.
Holbrook BD. The effects of nicotine on human fetal development. Birth Defects Res C Embryo Today. 2016;108(2):181–92.
Sanner T, Grimsrud TK. Nicotine: carcinogenicity and effects on response to cancer treatment—a review. Front Oncol. 2015;5:196.
Waldum HL, Nilsen OG, Nilsen T, Rørvik H, Syversen V, Sanvik AK, et al. Long-term effects of inhaled nicotine. Life Sci. 1996;58(16):1339–46.
Cucina A, Dinicola S, Coluccia P, Proietti S, D’Anselmi F, Pasqualato A, et al. Nicotine stimulates proliferation and inhibits apoptosis in colon cancer cell lines through activation of survival pathways. J Surg Res. 2012;178(1):233–41.
Wu SY, Xing F, Sharma S, Wu K, Tyagi A, Liu Y, et al. Nicotine promotes brain metastasis by polarizing microglia and suppressing innate immune function. J Exp Med. 2020;217(8):e20191131.
Roemer E, Stabbert R, Rustemeier K, Veltel DJ, Meisgen TJ, Reininghaus W, et al. Chemical composition, cytotoxicity and mutagenicity of smoke from US commercial and reference cigarettes smoked under two sets of machine smoking conditions. Toxicology. 2004;195(1):31–52.
Mayer B. How much nicotine kills a human? Tracing back the generally accepted lethal dose to dubious self-experiments in the nineteenth century. Arch Toxicol. 2014;88(1):5–7.
Brown CJ, Cheng JM. Electronic cigarettes: product characterisation and design considerations. Tob Control. 2014;23(Suppl 2):ii4-10.
Food and Drug Administration. SCOGS (Select Committee on GRAS Substances). 2019 (updated April 29, 2019). https://www.accessdata.fda.gov/scripts/fdcc/index.cfm?set=SCOGS&sort=Sortsubstance&order=ASC&startrow=251&type=basic&search= . Accessed 14 April 2020.
Wieslander G, Norback D, Lindgren T. Experimental exposure to propylene glycol mist in aviation emergency training: acute ocular and respiratory effects. Occup Environ Med. 2001;58(10):649–55.
Choi H, Schmidbauer N, Sundell J, Hasselgren M, Spengler J, Bornehag CG. Common household chemicals and the allergy risks in pre-school age children. PLoS One. 2010;5(10):e13423.
Kienhuis AS, Soeteman-Hernandez LG, Bos PMJ, Cremers HWJM, Klerx WN, Talhout R. Potential harmful health effects of inhaling nicotine-free shisha-pen vapor: a chemical risk assessment of the main components propylene glycol and glycerol. Tob Induc Dis. 2015;13(1):15.
Renne RA, Wehner AP, Greenspan BJ, Deford HS, Ragan HA, Westerberg RB, et al. 2-Week and 13-week inhalation studies of aerosolized glycerol in rats. Inhal Toxicol. 1992;4(2):95–111.
Article CAS Google Scholar
Behar R, Wang Y, Talbot P. Comparing the cytotoxicity of electronic cigarette fluids, aerosols and solvents. Tob Control. 2018;27(3):325.
Massarsky A, Abdel A, Glazer L, Levin ED, Di Giulio RT. Neurobehavioral effects of 1,2-propanediol in zebrafish (Danio rerio). Neurotoxicology. 2018;65:111–24.
Geiss O, Bianchi I, Barrero-Moreno J. Correlation of volatile carbonyl yields emitted by e-cigarettes with the temperature of the heating coil and the perceived sensorial quality of the generated vapours. Int J Hyg Environ Health. 2016;219(3):268–77.
Counts ME, Morton MJ, Laffoon SW, Cox RH, Lipowicz PJ. Smoke composition and predicting relationships for international commercial cigarettes smoked with three machine-smoking conditions. Regul Toxicol Pharmacol. 2005;41(3):185–227.
Agency for Toxic Substances & Disease Registry. Toxicological Profile for Formaldehyde. 2019 (updated September 26, 2019). https://www.atsdr.cdc.gov/ToxProfiles/tp.asp?id=220&tid=39 . Accessed 9 April 2020.
Agency for Toxic Substances & Disease Registry. Toxicological Profile for Acrolein. 2019 (updated September 26, 2019). https://www.atsdr.cdc.gov/toxprofiles/TP.asp?id=557&tid=102 . Accessed 9 April 2020
Moghe A, Ghare S, Lamoreau B, Mohammad M, Barve S, McClain C, et al. Molecular mechanisms of acrolein toxicity: relevance to human disease. Toxicol Sci. 2015;143(2):242–55.
Seitz HK, Stickel F. Acetaldehyde as an underestimated risk factor for cancer development: role of genetics in ethanol metabolism. Genes Nutr. 2010;5(2):121–8.
Faroon O, Roney N, Taylor J, Ashizawa A, Lumpkin MH, Plewak DJ. Acrolein health effects. Toxicol Ind Health. 2008;24(7):447–90.
Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133–9.
Farsalinos KE, Voudris V. Do flavouring compounds contribute to aldehyde emissions in e-cigarettes? Food Chem Toxicol. 2018;115:212–7.
Kavvalakis MP, Stivaktakis PD, Tzatzarakis MN, Kouretas D, Liesivuori J, Alegakis AK, et al. Multicomponent analysis of replacement liquids of electronic cigarettes using chromatographic techniques. J Anal Toxicol. 2015;39(4):262–9.
Etter JF, Zather E, Svensson S. Analysis of refill liquids for electronic cigarettes. Addiction. 2013;108(9):1671–9.
Etter JF, Bugey A. E-cigarette liquids: constancy of content across batches and accuracy of labeling. Addict Behav. 2017;73:137–43.
Varlet V, Farsalinos K, Augsburger M, Thomas A, Etter JF. Toxicity assessment of refill liquids for electronic cigarettes. Int J Environ Res Public Health. 2015;12(5):4796–815.
McAuley TR, Hopke PK, Zhao J, Babaian S. Comparison of the effects of e-cigarette vapor and cigarette smoke on indoor air quality. Inhal Toxicol. 2012;24(12):850–7.
Cullen KA, Gentzke AS, Sawdey MD, Chang JT, Anic GM, Wang TW, et al. e-Cigarette use among youth in the United States, 2019. JAMA. 2019;322(21):2095–103.
Villanti AC, Johnson AL, Ambrose BK, Cummings KM, Stanton CA, Rose SW, et al. Flavored tobacco product use in youth and adults: findings from the first wave of the PATH Study (2013–2014). Am J Prev Med. 2017;53(2):139–51.
Food and Drug Administration. Vaporizers, E-Cigarettes, and other Electronic Nicotine Delivery Systems (ENDS) 2020 (updated April 13, 2020). https://www.fda.gov/tobacco-products/products-ingredients-components/vaporizers-e-cigarettes-and-other-electronic-nicotine-delivery-systems-ends . Accessed 15 April 2020
Omaiye EE, McWhirter KJ, Luo W, Tierney PA, Pankow JF, Talbot P. High concentrations of flavor chemicals are present in electronic cigarette refill fluids. Sci Rep. 2019;9(1):2468.
Bahl V, Lin S, Xu N, Davis B, Wang YH, Talbot P. Comparison of electronic cigarette refill fluid cytotoxicity using embryonic and adult models. Reprod Toxicol. 2012;34(4):529–37.
Behar R, Davis B, Wang Y, Bahl V, Lin S, Talbot P. Identification of toxicants in cinnamon-flavored electronic cigarette refill fluids. Toxicol In Vitro. 2014;28(2):198–208.
Morgan DL, Flake GP, Kirby PJ, Palmer SM. Respiratory toxicity of diacetyl in C57BL/6 mice. Toxicol Sci. 2008;103(1):169–80.
Hubbs AF, Cumpston AM, Goldsmith WT, Battelli LA, Kashon ML, Jackson MC, et al. Respiratory and olfactory cytotoxicity of inhaled 2,3-pentanedione in Sprague-Dawley rats. Am J Pathol. 2012;181(3):829–44.
Vas CA, Porter A, Mcadam K. Acetoin is a precursor to diacetyl in e-cigarette liquids. Food Chem Toxicol. 2019;133:110727.
Allen JG, Flanigan SS, LeBlanc M, Vallarino J, MacNaughton P, Stewart JH, et al. Flavoring chemicals in E-cigarettes: diacetyl, 2,3-pentanedione, and acetoin in a sample of 51 products, including fruit-, candy-, and cocktail-flavored E-cigarettes. Environ Health Perspect. 2016;124(6):733–9.
Park RM, Gilbert SJ. Pulmonary impairment and risk assessment in a diacetyl-exposed population: microwave popcorn workers. J Occup Environ Med. 2018;60(6):496–506.
Muthumalage T, Prinz M, Ansah KO, Gerloff J, Sundar IK, Rahman I. Inflammatory and oxidative responses induced by exposure to commonly used e-cigarette flavoring chemicals and flavored e-liquids without nicotine. Front Physiol. 2017;8:1130.
Sherwood CL, Boitano S. Airway epithelial cell exposure to distinct e-cigarette liquid flavorings reveals toxicity thresholds and activation of CFTR by the chocolate flavoring 2,5-dimethypyrazine. Respir Res. 2016;17(1):57.
Pinkston R, Zaman H, Hossain E, Penn AL, Noël A. Cell-specific toxicity of short-term JUUL aerosol exposure to human bronchial epithelial cells and murine macrophages exposed at the air–liquid interface. Respir Res. 2020;21(1):269.
Williams M, Villarreal A, Bozhilov K, Lin S, Talbot P. Metal and silicate particles including nanoparticles are present in electronic cigarette cartomizer fluid and aerosol. PLoS One. 2013;8(3):e57987.
Mikheev VB, Brinkman MC, Granville CA, Gordon SM, Clark PI. Real-time measurement of electronic cigarette aerosol size distribution and metals content analysis. Nicotine Tob Res. 2016;18(9):1895–902.
Williams M, Bozhilov K, Ghai S, Talbot P. Elements including metals in the atomizer and aerosol of disposable electronic cigarettes and electronic hookahs. PLoS One. 2017;12(4):e0175430.
Kleinman MT, Arechavala RJ, Herman D, Shi J, Hasen I, Ting A, et al. E-cigarette or vaping product use-associated lung injury produced in an animal model from electronic cigarette vapor exposure without tetrahydrocannabinol or vitamin E oil. J Am Heart Assoc. 2020;9(18):e017368.
Patnode CD, Henderson JT, Thompson JH, Senger CA, Fortmann SP, Whitlock EP. Behavioral counseling and pharmacotherapy interventions for tobacco cessation in adults, including pregnant women: a review of reviews for the U.S. preventive services task force. Ann Intern Med. 2015;163(8):608–21.
Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34(3):509–15.
Bansal V, Kim K-H. Review on quantitation methods for hazardous pollutants released by e-cigarette (EC) smoking. Trends Analyt Chem. 2016;78:120–33.
Mantey DS, Pasch KE, Loukas A, Perry CL. Exposure to point-of-sale marketing of cigarettes and E-cigarettes as predictors of smoking cessation behaviors. Nicotine Tob Res. 2019;21(2):212–9.
Selya AS, Dierker L, Rose JS, Hedeker D, Mermelstein RJ. The role of nicotine dependence in E-cigarettes’ potential for smoking reduction. Nicotine Tob Res. 2018;20(10):1272–7.
Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4(2):116–28.
Levy DT, Yuan Z, Luo Y, Abrams DB. The relationship of e-cigarette use to cigarette quit attempts and cessation: insights from a large, nationally representative U.S. survey. Nicotine Tob Res. 2017;20(8):931–9.
Article PubMed Central Google Scholar
Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, et al. A randomized trial of E-cigarettes versus nicotine-replacement therapy. N Engl J Med. 2019;380(7):629–37.
Polosa R, Morjaria JB, Caponnetto P, Prosperini U, Russo C, Pennisi A, et al. Evidence for harm reduction in COPD smokers who switch to electronic cigarettes. Respir Res. 2016;17(1):166.
Litt MD, Duffy V, Oncken C. Cigarette smoking and electronic cigarette vaping patterns as a function of e-cigarette flavourings. Tob Control. 2016;25(Suppl 2):ii67–72.
Palmer AM, Brandon TH. How do electronic cigarettes affect cravings to smoke or vape? Parsing the influences of nicotine and expectancies using the balanced-placebo design. J Consult Clin Psychol. 2018;86(5):486–91.
Majmundar A, Allem JP, Cruz TB, Unger JB. Public health concerns and unsubstantiated claims at the intersection of vaping and COVID-19. Nicotine Tob Res. 2020;22(9):1667–8.
Berlin I, Thomas D, Le Faou A-L, Cornuz J. COVID-19 and smoking. Nicotine Tob Res. 2020;22(9):1650–2.
Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh C-L, Abiona O, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–3.
Wang K, Gheblawi M, Oudit GY. Angiotensin Converting Enzyme 2: A Double-Edged Sword. Circulation. 2020;142(5):426–8.
Sharma P, Zeki AA. Does vaping increase susceptibility to COVID-19? Am J Respir Crit Care Med. 2020;202(7):1055–6.
Brake SJ, Barnsley K, Lu W, McAlinden KD, Eapen MS, Sohal SS. Smoking upregulates angiotensin-converting enzyme-2 receptor: a potential adhesion site for novel coronavirus SARS-CoV-2 (Covid-19). J Clin Med. 2020;9(3):841.
Zhang H, Rostamim MR, Leopold PL, Mezey JG, O’Beirne SL, Strulovici-Barel Y, et al. Reply to sharma and zeki: does vaping increase susceptibility to COVID-19? Am J Respir Crit Care Med. 2020;202(7):1056–7.
Cheng H, Wang Y, Wang GQ. Organ-protective effect of angiotensin-converting enzyme 2 and its effect on the prognosis of COVID-19. J Med Virol. 2020;92(7):726–30.
Lerner CA, Sundar IK, Yao H, Gerloff J, Ossip DJ, McIntosh S, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS ONE. 2015;10(2):e0116732.
Download references
Acknowledgements
The authors gratefully acknowledge Dr. Cruz González, Pulmonologist at University Clinic Hospital of Valencia (Valencia, Spain) for her thoughtful suggestions and support.
This work was supported by the Spanish Ministry of Science and Innovation [Grant Number SAF2017-89714-R]; Carlos III Health Institute [Grant Numbers PIE15/00013, PI18/00209]; Generalitat Valenciana [Grant Number PROMETEO/2019/032, Gent T CDEI-04/20-A and AICO/2019/250], and the European Regional Development Fund.
Author information
Authors and affiliations.
Department of Pharmacology, Faculty of Medicine, University of Valencia, Avda. Blasco Ibañez 15, 46010, Valencia, Spain
Patrice Marques, Laura Piqueras & Maria-Jesus Sanz
Institute of Health Research INCLIVA, University Clinic Hospital of Valencia, Valencia, Spain
CIBERDEM-Spanish Biomedical Research Centre in Diabetes and Associated Metabolic Disorders, ISCIII, Av. Monforte de Lemos 3-5, 28029, Madrid, Spain
Laura Piqueras & Maria-Jesus Sanz
You can also search for this author in PubMed Google Scholar
Contributions
All authors discussed and agreed to the scope of the manuscript and contributed to the development of the manuscript at all stages. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Maria-Jesus Sanz .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors of the manuscript declare no conflicts of interest and take sole responsibility for the writing and content of the manuscript. None of the authors have been involved in legal or regulatory matters related to the contents of this paper.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Marques, P., Piqueras, L. & Sanz, MJ. An updated overview of e-cigarette impact on human health. Respir Res 22 , 151 (2021). https://doi.org/10.1186/s12931-021-01737-5
Download citation
Received : 22 October 2020
Accepted : 03 May 2021
Published : 18 May 2021
DOI : https://doi.org/10.1186/s12931-021-01737-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Electronic cigarette
- E-cigarette
- Flavourings
- Smoking cessation tool
Respiratory Research
ISSN: 1465-993X
- General enquiries: [email protected]
- Essay Topic Generator
- Essay Grader
- Reference Finder
- AI Outline Generator
- Paragraph Expander
- Essay Expander
- Literature Review Generator
- Thesis Generator
- Text Editing Tools
- AI Rewording Tool
- AI Sentence Rewriter
- AI Article Spinner
- AI Grammar Checker
- Spell Checker
- PDF Spell Check
- Paragraph Checker
- Free AI Essay Writer
- Paraphraser
- Grammar Checker
- Citation Generator
- Plagiarism Checker
- AI Detector
- AI Essay Checker
- Proofreading Service
- Editing Service
- AI Writing Guides
- AI Detection Guides
- Citation Guides
- Grammar Guides
- Paraphrasing Guides
- Plagiarism Guides
- Summary Writing Guides
- STEM Guides
- Humanities Guides
- Language Learning Guides
- Coding Guides
- Top Lists and Recommendations
- AI Detectors
- AI Writing Services
- Coding Homework Help
- Citation Generators
- Editing Websites
- Essay Writing Websites
- Language Learning Websites
- Math Solvers
- Paraphrasers
- Plagiarism Checkers
- Reference Finders
- Spell Checkers
- Summarizers
- Tutoring Websites
- Essay Checkers
- Essay Topic Finders
Most Popular
12 days ago
Demure TikTok Trend Explained: What It Is and Why It’s Going Viral
How to develop a homework routine that works, how to reduce screen time in the era of tiktoks, and be a productive student, how to write a bridge in an essay.
13 days ago

What Should You Try Before Graduating? Senior Bucket List
Why e-cigarettes are better for smokers than regular ones essay sample, example.

Smoking tobacco is probably one of the worst habits humankind has developed. Originating as a tradition of the Native Americans, practiced mostly on special occasions, smoking has gradually become a kind of mass addiction. Due to the efforts of tobacco companies seeking to increase their sales, people started smoking more and more often; the evolution of a more traditional pipe to a cigarette took some time, but eventually tobacco became more affordable and easier to use (you now simply need to light it up, instead of having to always carry a tobacco pouch, stuff a pipe, puff it, and so on). As a result, deaths and health issues connected to tobacco consumption became a worldwide concern.
A popular belief is that it is nicotine that kills. It is only partially true: although nicotine does harm one’s health (mostly affecting the cardiovascular system), it is the tar, carbon monoxide, hard particles contained in cigarette smoke, and a bunch of toxic emissions and heavy metals that deal the most damage. Nicotine causes addiction, and the smoke does the rest.
Nowadays, there are alternatives to analogue tobacco smoking: the widely popular electronic cigarettes. Although it is hotly debated whether e-cigarettes are harmful to smokers’ health or not, it is hard to argue that substituting cigarettes with these devices does more good than bad, since they possess a number of advantages that cannot be neglected easily. And whereas smoking still remains a dangerous and unacceptable addiction, e-cigarettes might be a decent way to break free of it.
Electronic cigarettes deliver nicotine to a smoker not through burning (which obviously implies inhaling harmful and toxic smoke), but through the evaporation of nicotine-containing liquids. An e-cigarette heats up the liquid in a special container called an atomizer; the liquid evaporates, and through this vapor a smoker receives their dose of nicotine. Thus, the process of nicotine consumption in this case should be called “vaping,” not “smoking.” These liquids usually comprise glycerol, propylene glycol, ethylene glycol, propanediol, and some other components ( NCBI ). Although some of them are not completely harmless, the chemical composure of e-cigarette liquids is definitely safer than the one of a regular cigarette. However, thorough control over the composure of these liquids should be established, and the usage of such components as ethylene glycol and propanediol should probably be banned. Still, if a smoker does not plan to quit, he or she might want to consider using e-cigarettes instead of real tobacco.
Another good reason for a smoker to start using e-cigarettes is that the aforementioned liquids can contain different amounts of nicotine. A heavy smoker might want to start vaping using liquids containing up to 24 milligrams of nicotine, and the good news for them is that it is possible to gradually decrease the dose until zero milligrams are present.
Although some smokers might experience physical symptoms when trying to quit smoking tobacco, in the majority of cases, it is a strong psychological component that does not let a smoker give up their addiction. It can be assumed that there are five main components of this psychological addiction: 1) believing in the relaxing/stimulating effect of nicotine that helps a smoker deal with stressful situations; 2) a smoker’s need to “keep hands busy” when bored, waiting for something, feeling nervous, and so on; 3) socializing with “fellow smokers”; 4) unconsciously and “automatically” following the habit; 5) the fear that if a smoker quits, he or she will lose something valuable, a source of psychological support or pleasure. In addition, some smokers find it aesthetic to inhale/exhale smoke, or have other reasons to continue tobacco consumption. Generally speaking, smoking is a behavioral pattern consisting of repeating situations and reactions. Without neglecting or challenging these reasons, it can be said that an e-cigarette is probably a safer alternative for a person who does not want to give up nicotine. They still deliver nicotine to a smoker’s body (thus fulfilling the reasons 1 and 5); they disrupt automatic smoking described in points 2 and 4 (since e-cigarettes function differently from their traditional analogues); they allow a person to continue socializing with other smokers during breaks at work, or on other occasions, as mentioned in point 3. But, while performing the same functions as regular cigarettes, electronic devices are safer and more socially acceptable.
In addition, a purely aesthetic reason to prefer e-cigarettes over their analogues: when evaporated, the liquids taste and smell better than tobacco. They are sold in a variety of flavors: melons, apples, cherry, tropical fruit, mint, blueberry, and so on. At the same time, regular tobacco smells and tastes awful not only for the non-smokers, but for a smoking person as well. So, why not stop poisoning oneself with toxic smoke, and at least substitute it with pleasantly smelling vapor?
Nicotine addiction in any of its forms, regardless of whether it is smoking or vaping, is a huge problem for addicts. It leads to a number of severe, chronic diseases and even to death. At the same time, there might be a healthier alternative for those smokers who realize the harm they cause to themselves, but who cannot yet give up their addiction. Electronic cigarettes are nowadays considered to be safer than regular cigarettes. Liquids used in these e-cigarettes contain fewer toxic elements, and do not include the products that are commonly burned in cigarettes. Vapor from e-cigarettes is mostly harmless to non-smokers; it tastes and smells better, which makes smoking e-cigarettes a less reproached habit. Finally, many smokers might discover that e-cigarettes do not obstruct their reasons to continue smoking, while making it possible to decrease the amounts of consumed nicotine and to eventually break the habit. Therefore, without praising or advertising e-cigarettes, it can still be stated that they are a more preferable alternative for smokers.
Works Cited
- “Electronic Cigarettes: Overview of Chemical Composition and Exposure Estimation.” NCBI . BioMed Central, 2014. Web. 14 Nov. 2016.
Follow us on Reddit for more insights and updates.
Comments (1)
Welcome to A*Help comments!
We’re all about debate and discussion at A*Help.
We value the diverse opinions of users, so you may find points of view that you don’t agree with. And that’s cool. However, there are certain things we’re not OK with: attempts to manipulate our data in any way, for example, or the posting of discriminative, offensive, hateful, or disparaging material.
Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Who is the original author of this article?
More from Best Persuasive Essay Examples

May 28 2023
How does outdoor exercises impact our health and well-being? Essay Sample, Example

Should Screen Time Be Limited? Essay Sample, Example

Why Video Games are Good for the Brain. Essay Sample, Example
Remember Me
What is your profession ? Student Teacher Writer Other
Forgotten Password?
Username or Email
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
E-cigarettes are harmful to health
Globally, there are 1.1 billion adult smokers, 60% of them want or intend to quit. Much has been written and said about the potential of electronic nicotine delivery systems (ENDS) such as e-cigarettes to help tobacco users quit. While the evidence is still inconclusive, e-cigarettes are often used along with one or more tobacco products. As this is the practice with many ENDS users, the health effects of two or more products are combined. Governments who want to weigh the potential benefits and risks of e-cigarettes for their population should consider the following:
- Regarding the potential health effects for which the evidence is mounting, there is insufficient data to understand the full breadth of their impact on health as devices have not been on the market long enough. Especially the long-term effects of using e-cigarettes or being exposed to them are yet unknown.
- Nevertheless, the evidence is clear that the aerosols of the majority of ENDS contain toxic chemicals, including nicotine and substances that can cause cancer.ENDS on their own are associated with increased risk of cardiovascular diseases and lung disorders and adverse effects on the development of the fetus during pregnancy. ENDS are undoubtedly harmful, should be strictly regulated, and, most importantly, must be kept away from children. Nicotine is highly addictive and found in most e-cigarettes. Both tobacco products and e-cigarettes pose risks to health and the safest approach is not to consume either.
- It is of particular public health concern that increasingly children and adolescents take up the use of e-cigarettes in some countries. Most ENDS can be manipulated by the user. Some manufacturers also hold patents to remotely manipulate nicotine dosages and toxicant delivery. Furthermore, there is a growing body of evidence in some countries that never-smoker adolescents who use ENDS at least double their chance of starting to smoke cigarettes later in life. Exposing children and adolescents to nicotine can have long-lasting, damaging effects on brain development and lead to nicotine addiction.
WHO continues to monitor the evidence and technological developments and will adapt this statement accordingly.
Jump to navigation
- Bahasa Indonesia
- Bahasa Malaysia

Conclusions about the effects of electronic cigarettes remain the same

An updated Cochrane Review provides an independent, rigorous assessment of the best available evidence to date about electronic cigarettes for quitting smoking.
Scroll to the bottom of this article for a round-up of media coverage
The conclusions of this updated Review are unchanged since the last review was published two years ago: electronic cigarettes may help smokers stop their smoking, and the included studies did not find any serious side effects associated with their use for up to two years.
Many studies are now underway which may help us understand more about their effects in the future.
The first Cochrane Review, published in the Cochrane Library in December 2014, showed that electronic cigarettes may be an aid to smokers in stopping their smoking. The updated Review did not find any new randomized controlled trials (RCTs) with long-term outcomes looking at the effectiveness of electronic cigarettes in helping people to stop smoking. However, this is an active area of research, with a large number of ongoing studies that will add to the evidence in the next few years.
Smoking is a significant global health problem. Despite many smokers wanting to stop, they often find it difficult to succeed in the long term. One of the most effective and widely used strategies to help combat the cravings associated with nicotine addiction is to deliver nicotine by patches and chewing gum.
Electronic cigarettes have been around in some form for a number of years, but over the past few years their popularity has increased significantly, and they have begun to look and feel less like conventional cigarettes. Unlike chewing gum and patches, they mimic the experience of cigarette smoking because they are hand-held and generate a smoke-like vapour when used. They help to recreate similar sensations of smoking without exposing users or others to the smoke from conventional cigarettes, and can be used to provide smokers with nicotine. Though they are used by many smokers, little is still known about how effective they are at helping people stop smoking.
This version of the updated Cochrane Review includes no new RCTs. The original Review included two RCTs involving more than 600 participants, and found that electronic cigarettes containing nicotine may increase the chances of stopping smoking within six to 12 months, compared to using an electronic cigarette without nicotine. The researchers could not determine whether using electronic cigarettes was better than a nicotine patch in helping people stop smoking, because there were not enough people taking part in the study.
This updated Review now includes observational data from an additional 11 studies. Of the studies which measured side effects, none found any serious side effects of using electronic cigarettes for up to two years. The studies showed that throat and mouth irritation are the most commonly reported side effects in the short to medium term (up to two years).
The lead author of this Cochrane Review, Jamie Hartmann-Boyce from the Cochrane Tobacco Addiction Group, said, “The randomized evidence on smoking cessation is unchanged since the last version of the Review. We are encouraged to find many studies are now underway, particularly as electronic cigarettes are an evolving technology. Since the last version of the Review, 11 new observational and uncontrolled studies have been published. In terms of quitting, these can’t provide the same information we get from randomized controlled trials, but they contribute further information on the side effects of using electronic cigarettes to quit smoking. None detected any serious side effects, but longer term data are needed.”
Read this Press Release in French, Spanish or Polish .
Editor’s notes Full citation: Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation . Cochrane Database of Systematic Reviews 2016, Issue 9. Art. No.: CD010216. DOI: 10.1002/14651858.CD010216.pub3.
Cochrane Review Author contact details : [email protected]
For all media enquiries, please contact:
Jo Anthony Senior Media and Communications Officer, Cochrane M +44(0) 7582 726 634 E [email protected] or [email protected]
About Cochrane Cochrane is a global independent network of researchers, professionals, patients, carers, and people interested in health. Cochrane produces reviews which study all of the best available evidence generated through research and make it easier to inform decisions about health. These are called systematic reviews. Cochrane is a not-for-profit organization with collaborators from more than 130 countries working together to produce credible, accessible health information that is free from commercial sponsorship and other conflicts of interest. Our work is recognized as representing an international gold standard for high quality, trusted information.
Find out more at cochrane.org | Follow us on twitter @cochranecollab
If you are a journalist or member of the press and wish to receive news alerts before their online publication or if you wish to arrange an interview with an author, please contact the Cochrane press office: [email protected]
About Wiley Wiley is a global provider of knowledge and knowledge-enabled services that improve outcomes in areas of research, professional practice, and education. Through the Research segment, the Company provides digital and print scientific, technical, medical, and scholarly journals, reference works, books, database services, and advertising. The Professional Development segment provides digital and print books, online assessment and training services, and test prep and certification. In Education, Wiley provides education solutions including online program management services for higher education institutions and course management tools for instructors and students, as well as print and digital content. The Company's website can be accessed at http://www.wiley.com .
Selected Media Coverage:
E-cigarettes can help smokers quit, says study in The Guardian . Why can't scientists agree on e-cigarettes? blog post in The Guardian . E-Cigs Might Help Some Quit Smoking, New Study Reveals on Consumer Reports .
- Help & Support
- Quit Smoking
- E-Cigarettes & Vaping
The Impact of E-Cigarettes on the Lung
Download PDF En Español
E-cigarettes are a relatively new tobacco product that have been sold in the U.S. for about a decade The e-cigarettes currently in the U.S. marketplace have not been systemically reviewed by the Food and Drug Administration to determine their impact on lung health. While much remains to be determined about the lasting health consequences of these products, the American Lung Association is very troubled by the evolving evidence about the impact of e-cigarettes on the lungs.
The Inhalation of Harmful Chemicals Can Cause Irreversible Lung Damage and Lung Disease
In January 2018, the National Academies of Science, Engineering and Medicine 1 released a consensus study report that reviewed over 800 different studies.
That report made clear: using e-cigarettes causes health risks. It concluded that e-cigarettes both contain and emit a number of potentially toxic substances. The Academies' report also states there is moderate evidence that youth who use e-cigarettes are at increased risk for cough and wheezing and an increase in asthma exacerbations.
- A study from the University of North Carolina found that the two primary ingredients found in e-cigarettes—propylene glycol and vegetable glycerin—are toxic to cells and that the more ingredients in an e-liquid, the greater the toxicity. 2
- E-cigarettes produce a number of dangerous chemicals including acetaldehyde, acrolein, and formaldehyde. These aldehydes can cause lung disease, as well as cardiovascular (heart) disease. 3
- E-cigarettes also contain acrolein, a herbicide primarily used to kill weeds. It can cause acute lung injury and COPD and may cause asthma and lung cancer. 4
- Both the U.S. Surgeon General and the National Academies of Science, Engineering and Medicine have warned about the risks of inhaling secondhand e-cigarette emissions, which are created when an e-cigarette user exhales the chemical cocktail created by e-cigarettes.
- In 2016, the Surgeon General concluded that secondhand emissions contain, "nicotine; ultrafine particles; flavorings such as diacetyl, a chemical linked to serious lung disease; volatile organic compounds such as benzene, which is found in car exhaust; and heavy metals, such as nickel, tin, and lead."
- The Food and Drug Administration has not found any e-cigarette to be safe and effective in helping people who use tobacco products to quit. If people are ready to quit smoking and using other tobacco products for good, they should call 1-800-QUIT NOW or talk with their doctor about finding the best way to quit using proven methods and FDA-approved treatments and counseling.
NAM Report - https://www.nap.edu/resource/24952/012318ecigaretteConclusionsbyEvidence.pdf
Sassano MF, Davis ES, Keating JE, Zorn BT, Kochar TK, Wolfgang MC, et al. (2018) Evaluation of e-liquid toxicity using an open-source high-throughput screening assay. PLoS Biol 16(3): e2003904. https://doi.org/10.1371/journal.pbio.2003904
Ogunwale, Mumiye A et al. (2017) Aldehyde Detection in Electronic Cigarette Aerosols. ACS omega 2(3): 1207-1214. doi: 10.1021/acsomega.6b00489].
Bein K, Leikauf GD. (2011) Acrolein - a pulmonary hazard. Mol Nutr Food Res 55(9):1342-60. doi: 10.1002/mnfr.201100279.
Page last updated: July 31, 2024
A Breath of Fresh Air in Your Inbox
Want updates on the latest lung health news, including COVID-19, research, inspiring stories and health information?
You will now receive email updates from the American Lung Association.
Make a Donation
Your tax-deductible donation funds lung disease and lung cancer research, new treatments, lung health education, and more.
Become a Lung Health Insider
Join over 700,000 people who receive the latest news about lung health, including research, lung disease, air quality, quitting tobacco, inspiring stories and more!
Thank you! You will now receive email updates from the American Lung Association.
Select Your Location
Select your location to view local American Lung Association events and news near you.
Change Language
Lung helpline.
Talk to our lung health experts at the American Lung Association. Our service is free and we are here to help you.
1-800-LUNG-USA
(1-800-586-4872)
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- E-cigarettes: the best...
E-cigarettes: the best and the worst case scenarios for public health—an essay by Simon Chapman
- Related content
- Peer review
- Simon Chapman , professor of public health
- 1 School of Public Health, University of Sydney 2006, Australia
- simon.chapman{at}sydney.edu.au
Considerable energy is going into envisioning the likely benefits and harms of the proliferation of e-cigarettes, the use of which is growing exponentially in some countries. Simon Chapman reflects on two possible long term patterns of use and argues that we must not repeat the mistakes with the way in which tobacco was sold and marketed
The World Health Organization’s recent report on electronic nicotine delivery systems repeatedly notes the poverty of evidence to guide policy. It recommends that governments regulate the products, their promotion, and where they can be used in public as well as supporting research into their safety and efficacy in smoking cessation. 1 2 The report is due for consideration at the sixth conference of the parties to the WHO Framework Convention on Tobacco Control, which will be held on 13-18 October 2014 in Moscow.
In this essay, I consider the best and worst case scenarios for e-cigarettes; claims that they assist in smoking cessation and their value if users continue to smoke; and, finally, the tobacco industry’s interests in these products.
Best case scenario
The best outcome with e-cigarettes would be a massive, rapid migration of smokers into vaping, akin to the magnitude of the replacement of film by digital cameras. Unparalleled declines in diseases caused by smoking would occur, starting with cardiovascular and respiratory diseases and followed years later by cancers caused by smoking. Overwhelmingly, vapers would be smokers whose principal motivation was smoking cessation. Although some might vape and smoke (“dual users”) temporarily, nearly all would completely quit smoking.
Uptake of vaping among former smokers and never smoking children would be extremely low, and longitudinal studies of children who started vaping would show negligible transition to smoking. Like adults, children would use e-cigarettes as a gateway out of smoking, not into it.
Continuing research would affirm …
Log in using your username and password
BMA Member Log In
If you have a subscription to The BMJ, log in:
- Need to activate
- Log in via institution
- Log in via OpenAthens
Log in through your institution
Subscribe from £184 *.
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for: £50 / $60/ €56 ( excludes VAT )
You can download a PDF version for your personal record.
Buy this article
Discussion: Vaping and E-Cigarettes Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Electronic nicotine delivery systems cause the same harm to the human body as other tobacco products. Plus, polyhydric alcohol solvents kill cell membranes. All this can lead to severe illnesses. If the main harmful effect of conventional cigarettes comes from tar and combustion products, here it comes from solvents (Dinardo & Rome, 2019; National Institute on Drug Abuse (NIDA/NIH), 2018). It is severe harm to health, so creeping because not only the membranes and cells of the lungs are dissolved, but also the brain and heart.
In 2019, the discussion about the negative impact of vaping on health intensified in the United States. In August of that year, the Illinois Department of Public Health reported what was believed to be the first death in the country due to a severe respiratory illness dubbed EVALI. This acronym stands for lung injury associated with the use of e-cigarettes or vaping products. By the end of the year, doctors were already talking about almost forty dead (Irusa et al., 2020). In total, the country’s authorities have identified several thousand cases of such diseases. The age of the dead varies from 17 to 75 years.
Consequently, e-cigarettes must be subject to laws governing the sale and distribution of traditional tobacco products. Making them available to young people is dangerous for the reasons mentioned above. The absence of tar and an unpleasant odor is the only external differences between a regular cigarette and a vape, while in reality, all the harm is contained within the composition of the products themselves and the inhaled vapor (Kennedy et al., 2022). Sales should also be restricted in some cases to persons over the age of 18. As smoking can affect the lungs and some other chronic diseases, the damage to health is already proven and evident. At the legislative level, it is recommended that people be able to buy a vape only if, after a medical examination, the doctor concludes based on which the risks of illness from vaping will be reduced. According to the certificates, electronic cigarettes will be sold, reducing their consumption.
Dinardo, P., & Rome, E. S. (2019). Vaping: The new wave of nicotine addiction . Cleveland Clinic Journal of Medicine, 86 (12), 789-798. Web.
Irusa, K. F., Vence, B., & Donovan, T. (2020). Potential oral health effects of e‐cigarettes and vaping: A review and case reports . Journal of Esthetic and Restorative Dentistry, 32 (3), 260-264. Web.
Kennedy, V. Jendian, M. A. & Norwood, R. (2022). Think Critical Thinking About Social Problems . Kendall Hunt Publishing.
National Institute on Drug Abuse (NIDA/NIH). (2018). Why Teens are Attracted to Vaping [Video]. YouTube. Web.
- Depression and Anxiety Among Chronic Pain Patients
- Food Waste in American Hospitals
- Vaping: Negative Effects and Harm Reduction
- Laws Regarding Vaping and E-Cigarettes
- The Prevalence of Vaping Among Youths in Ireland
- Asthma: Description, Diagnosis and Treatment
- Applying Neural Stem Cells to Counteract Brain Aging
- “COVID-19: Impact on Nurses and Nursing” Study
- Data Collection in Healthcare Programs
- Effects of Aging on the Integumentary and Musculoskeletal Systems
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, January 8). Discussion: Vaping and E-Cigarettes. https://ivypanda.com/essays/discussion-vaping-and-e-cigarettes/
"Discussion: Vaping and E-Cigarettes." IvyPanda , 8 Jan. 2023, ivypanda.com/essays/discussion-vaping-and-e-cigarettes/.
IvyPanda . (2023) 'Discussion: Vaping and E-Cigarettes'. 8 January.
IvyPanda . 2023. "Discussion: Vaping and E-Cigarettes." January 8, 2023. https://ivypanda.com/essays/discussion-vaping-and-e-cigarettes/.
1. IvyPanda . "Discussion: Vaping and E-Cigarettes." January 8, 2023. https://ivypanda.com/essays/discussion-vaping-and-e-cigarettes/.
Bibliography
IvyPanda . "Discussion: Vaping and E-Cigarettes." January 8, 2023. https://ivypanda.com/essays/discussion-vaping-and-e-cigarettes/.

Public Health Consequences of E-Cigarettes (2018)
Chapter: summary.
E-cigarette aerosol contains fewer numbers and lower levels of most toxicants than does smoke from combustible tobacco cigarettes. Exposure to nicotine and to toxicants from the aerosolization of e-cigarette ingredients is dependent on user and device characteristics. Laboratory tests of e-cigarette ingredients, in vitro toxicological tests, and short-term human studies suggest that e-cigarettes are likely to be far less harmful than combustible tobacco cigarettes. However, the absolute risks of the products cannot be unambiguously determined at this time. Long-term health effects, of particular concern for youth who become dependent on such products, are not yet clear.
Although e-cigarette use might cause youth to transition to combustible tobacco products, it might also increase adult cessation of combustible tobacco cigarettes. The net public health effect, harm or benefit, of e-cigarettes depends on three factors: their effect on youth initiation of combustible tobacco products, their effect on adult cessation of combustible tobacco products, and their intrinsic toxicity. If e-cigarette use by adult smokers leads to long-term abstinence from combustible tobacco cigarettes, the benefit to public health could be considerable. Without that health benefit for adult smokers, e-cigarette use could cause considerable harm to public health in the short and long term due both to the inherent harms of exposure to e-cigarette toxicants and to the harms related to subsequent combustible tobacco use by those who begin using e-cigarettes in their youth.
Population modeling is a useful strategy to help estimate the balance of potential benefits and harms from e-cigarettes in the short term before more definite scientific data are available. Factors that would promote the potential health benefits associated with these products include determining with more precision
under which conditions e-cigarettes could serve as an effective smoking cessation aid, discouraging their use among youth through tobacco control strategies such as education and restrictions on products particularly appealing to youth, and increasing their safety through data-driven product engineering and design.
Millions of Americans use electronic cigarettes (e-cigarettes), even as rates of smoking 1 combustible tobacco cigarettes continue to decline among youth and adults. In 2016, youth e-cigarette use was substantially higher than cigarette smoking or use of any other tobacco product. A common picture emerges from national surveys. Prevalence of use increases with age in children and youth. E-cigarette use also varies by gender, with typically greater use among boys than girls. E-cigarette use also varies by race and ethnicity, with higher rates of use among youth who identify as Hispanic and non-Hispanic white compared with black, Asian, and other races. Early results suggest that use stabilized or decreased in youth between 2015 and 2016, despite increases between 2011 and 2015 across a range of measures and surveys. Substantial proportions of youth report using non-nicotine electronic cigarettes. Rates of e-cigarette use among adults are relatively low when compared with youth e-cigarette use and to adult combustible tobacco cigarette smoking. Most adult e-cigarette users report currently using other tobacco products. Among adults, as among youth, patterns of use vary by demographic subgroups—age, gender, and race and ethnicity. E-cigarette use is generally greatest among young adults and decreases with age in adults. Few adults begin using e-cigarettes who are not already using combustible tobacco cigarettes.
Despite their popularity, little is known about their health effects, and perceptions of potential risks and benefits of e-cigarette use vary widely among the public, users of e-cigarettes, health care providers, and the public health community. For example, whether e-cigarette use confers lower risk of addiction compared with combustible tobacco cigarettes is one point of controversy. Electronic cigarettes contain constituents that are not inert and are likely to have some negative health effects on their own. However, because the known risks of combustible tobacco are so great, understanding the net public health effect of e-cigarettes requires understanding not only the inherent risks of e-cigarettes, but also the relationship between e-cigarette use and combustible tobacco cigarette use.
Furthermore, concerns have been raised that e-cigarettes will induce youth to begin using combustible tobacco cigarettes. E-cigarette use among youth and young adults is especially worrying if e-cigarettes cause
___________________
1 The committee uses the verb “smoke” to refer to use of combustible tobacco cigarettes and “vape” to refer to use of e-cigarettes. Similarly “smoker” refers to someone who uses combustible tobacco cigarettes.
dependence or the normalization of smoking behavior, and subsequently lead youth and young adults to start smoking combustible tobacco cigarettes. This is of particular concern for youth who otherwise would never have smoked. Among adult populations, to the extent that e-cigarette use promotes either reduction or complete abstinence from combustible tobacco smoking, e-cigarettes may help to reduce health risks.
E-cigarettes are regulated as tobacco products 2 by the Center for Tobacco Products of the Food and Drug Administration (FDA), which requested that the National Academies of Sciences, Engineering, and Medicine convene a committee of experts to conduct a review of the emerging evidence about e-cigarettes and health, make recommendations for the improvement of this research, and highlight gaps that are a priority for future research. The Statement of Task can be found in Box S-1 .
The committee undertook a comprehensive review of the scientific literature regarding key constituents in e-cigarettes, human health effects, initiation and cessation of combustible tobacco cigarette use, and harm reduction. The committee considered the quality of individual studies, as well as the totality of the evidence to provide structured and consistent conclusions on the strength of the evidence. See Box S-2 for a summary of the framework the committee used for those conclusions. The committee notes that the framework is a guide, but that a great deal of expert judgment—in the evaluation of individual studies and in bodies of evidence—is always involved. The Annex to this Summary includes a compilation of the conclusions grouped by level of evidence, whereas they are listed by type of outcome in the sections that follow.
CONSTITUENTS
E-cigarettes contain liquids (referred to as e-liquids) that are aerosolized upon operation of the device. E-liquids typically contain nicotine (although some users prefer zero-nicotine solutions), flavorings, and humectants. Nicotine is a well-understood compound with known central and peripheral nervous system effects. It causes dependence and addiction, and exposure to nicotine from e-cigarettes likely elevates the cardiovascular disease risk in people with pre-existing cardiovascular disease(s), but the cardiovascular risk in people without cardiovascular disease(s) is uncertain. Based on studies of long-term users of nicotine replacement
2 If an e-cigarette manufacturer made a claim in packaging or advertising that the products were useful for smoking cessation, the product would be regulated as a drug-delivery device under different statutory authorities and not by the Center for Tobacco Products. E-cigarettes are regulated as tobacco products because the nicotine in the e-liquids derives from tobacco plants. The Food and Drug Administration recently exerted authority over e-cigarettes; those that do not contain nicotine may be reviewed on a case-by-case basis.
therapy or smokeless tobacco, nicotine exposure from e-cigarette use will likely pose minimal cancer risk to users. Most flavorings in e-liquids are designated as generally recognized as safe (also known as GRAS) by FDA, but those designations are for oral consumption in food and do not apply to flavorings used in e-cigarettes; most of these were never studied for toxicity via the inhalation route. The primary humectants are propylene glycol and glycerol, compounds also in widespread use for other purposes and about which significant scientific literature exists.
In reviewing the literature about the constituents in and exposures from e-cigarettes, the committee made nine conclusions:
Conclusion 3-1. There is conclusive evidence that e-cigarette use increases airborne concentrations of particulate matter and nicotine in indoor environments compared with background levels.
Conclusion 3-2. There is limited evidence that e-cigarette use increases levels of nicotine and other e-cigarette constituents on a variety of indoor surfaces compared with background levels.
Conclusion 4-1. There is conclusive evidence that exposure to nicotine from e-cigarettes is highly variable and depends on product characteristics (including device and e-liquid characteristics) and how the device is operated.
Conclusion 4-2. There is substantial evidence that nicotine intake from e-cigarette devices among experienced adult e-cigarette users can be comparable to that from combustible tobacco cigarettes.
Conclusion 5-1. There is conclusive evidence that in addition to nicotine, most e-cigarette products contain and emit numerous potentially toxic substances.
Conclusion 5-2. There is conclusive evidence that, other than nicotine, the number, quantity, and characteristics of potentially toxic substances emitted from e-cigarettes are highly variable and depend on product characteristics (including device and e-liquid characteristics) and how the device is operated.
Conclusion 5-3. There is substantial evidence that except for nicotine, under typical conditions of use, exposure to potentially toxic substances from e-cigarettes is significantly lower compared with combustible tobacco cigarettes.
Conclusion 5-4. There is substantial evidence that e-cigarette aerosol contains metals. The origin of the metals could be the metallic coil used to heat the e-liquid, other parts of the e-cigarette device, or e-liquids. Product characteristics and use patterns may contribute to differences in the actual metals and metal concentrations measured in e-cigarette aerosol.
Conclusion 5-5. There is limited evidence that the number of metals in e-cigarette aerosol could be greater than the number of metals in combustible tobacco cigarettes, except for cadmium, which is markedly lower in e-cigarettes compared with combustible tobacco cigarettes.
Taken together, the evidence in support of these conclusions suggests that e-cigarette aerosol contains fewer numbers and lower levels of toxicants than smoke from combustible tobacco cigarettes. Nicotine exposure can mimic that found with use of combustible tobacco cigarettes, but is highly variable. However, the exposure to nicotine and toxicants from the aerosolization of flavorings and humectants is dependent on user and device characteristics.
HUMAN HEALTH EFFECTS
Combustible tobacco cigarettes pose serious risks to human health; these risks are well documented and well understood. Many of those health effects emerge only after decades of cigarette smoking. E-cigarettes have only been on the market in the United States since 2006, making scientific comparisons between e-cigarettes and combustible tobacco cigarettes about most health effects difficult. However, research on short-term exposures to e-cigarettes and effects on disease symptoms and intermediate outcomes exist. An important distinction when considering these data
is whether the effects are seen in an e-cigarette user who had never used combustible tobacco cigarettes (usually children or youth) or in a combustible tobacco cigarette user, with and without preexisting tobacco-related disease, usually adults. The committee reviewed evidence on the effects of e-cigarettes in several health domains: dependence, cardiovascular disease, cancer, respiratory diseases, oral diseases, maternal and fetal outcomes, and injuries and poisonings. Although the amount of literature is relatively scant and complicated by the multiple types of e-cigarettes in use even within a given study, the committee made 26 conclusions about the effects of e-cigarettes on health.
Conclusion 7-1. There is substantial evidence that e-cigarette aerosols can induce acute endothelial cell dysfunction, although the long-term consequences and outcomes on these parameters with long-term exposure to e-cigarette aerosol are uncertain.
Conclusion 7-2. There is substantial evidence that components of e-cigarette aerosols can promote formation of reactive oxygen species/oxidative stress. Although this supports the biological plausibility of tissue injury and disease from long-term exposure to e-cigarette aerosols, generation of reactive oxygen species and oxidative stress induction is generally lower from e-cigarettes than from combustible tobacco cigarette smoke.
Conclusion 8-1. There is substantial evidence that e-cigarette use results in symptoms of dependence on e-cigarettes.
Conclusion 8-2. There is moderate evidence that risk and severity of dependence are lower for e-cigarettes than combustible tobacco cigarettes.
Conclusion 8-3. There is moderate evidence that variability in e-cigarette product characteristics (nicotine concentration, flavoring, device type, and brand) is an important determinant of risk and severity of e-cigarette dependence.
Conclusion 9-1. There is no available evidence whether or not e-cigarette use is associated with clinical cardiovascular outcomes (coronary heart disease, stroke, and peripheral artery disease) and subclinical atherosclerosis (carotid intima-media thickness and coronary artery calcification).
Conclusion 9-2. There is substantial evidence that heart rate increases shortly after nicotine intake from e-cigarettes.
Conclusion 9-3. There is moderate evidence that diastolic blood pressure increases shortly after nicotine intake from e-cigarettes.
Conclusion 9-4. There is limited evidence that e-cigarette use is associated with a short-term increase in systolic blood pressure, changes in biomarkers of oxidative stress, increased endothelial dysfunction and arterial stiffness, and autonomic control.
Conclusion 9-5. There is insufficient evidence that e-cigarette use is associated with long-term changes in heart rate, blood pressure, and cardiac geometry and function.
Conclusion 10-1. There is no available evidence whether or not e-cigarette use is associated with intermediate cancer endpoints in humans. This holds true for e-cigarette use compared with use of combustible tobacco cigarettes and e-cigarette use compared with no use of tobacco products.
Conclusion 10-2. There is limited evidence from in vivo animal studies using intermediate biomarkers of cancer to support the hypothesis that long-term e-cigarette use could increase the risk of cancer; there is no available evidence from adequate long-term animal bioassays of e-cigarette aerosol exposures to inform cancer risk.
Conclusion 10-3. There is limited evidence that e-cigarette aerosol can be mutagenic or cause DNA damage in humans, animal models, and human cells in culture.
Conclusion 10-4. There is substantial evidence that some chemicals present in e-cigarette aerosols (e.g., formaldehyde, acrolein) are capable of causing DNA damage and mutagenesis. This supports the biological plausibility that long-term exposure to e-cigarette aerosols could increase risk of cancer and adverse reproductive outcomes. Whether or not the levels of exposure are high enough to contribute to human carcinogenesis remains to be determined.
Conclusion 11-1. There is no available evidence whether or not e-cigarettes cause respiratory diseases in humans.
Conclusion 11-2. There is limited evidence for improvement in lung function and respiratory symptoms among adult smokers with asthma who switch to e-cigarettes completely or in part (dual use).
Conclusion 11-3. There is limited evidence for reduction of chronic obstructive pulmonary disease (COPD) exacerbations among adult smokers with COPD who switch to e-cigarettes completely or in part (dual use).
Conclusion 11-4. There is moderate evidence for increased cough and wheeze in adolescents who use e-cigarettes and an association with e-cigarette use and an increase in asthma exacerbations.
Conclusion 11-5. There is limited evidence of adverse effects of e-cigarette exposure on the respiratory system from animal and in vitro studies.
Conclusion 12-1. There is limited evidence suggesting that switching to e-cigarettes will improve periodontal disease in smokers.
Conclusion 12-2. There is limited evidence suggesting that nicotine- and non-nicotine–containing e-cigarette aerosol can adversely affect cell viability and cause cell damage of oral tissue in non-smokers.
Conclusion 13-1. There is no available evidence whether or not e-cigarettes affect pregnancy outcomes.
Conclusion 13-2. There is insufficient evidence whether or not maternal e-cigarette use affects fetal development.
Conclusion 14-1. There is conclusive evidence that e-cigarette devices can explode and cause burns and projectile injuries. Such risk is significantly increased when batteries are of poor quality, stored improperly, or modified by users.
Conclusion 14-2. There is conclusive evidence that intentional or accidental exposure to e-liquids (from drinking, eye contact, or dermal contact) can result in adverse health effects including but not limited to seizures, anoxic brain injury, vomiting, and lactic acidosis.
Conclusion 14-3. There is conclusive evidence that intentionally or unintentionally drinking or injecting e-liquids can be fatal.
Taken together, the evidence reviewed by the committee suggests that e-cigarettes are not without physiological activity in humans, but the implications for long-term effects on morbidity and mortality are not yet clear. Use of e-cigarettes instead of combustible tobacco cigarettes by those with existing respiratory disease might be less harmful.
INITIATION AND CESSATION
The Family Smoking Prevention and Tobacco Control Act of 2009, which is the basis for FDA’s regulatory authority over tobacco products,
including e-cigarettes, defined a unique regulatory standard, the public health standard. This requires that tobacco products introduced on the market after February 15, 2007, be shown to have a net population health benefit to users and non-users of the product. Operationally, if a product caused more people to begin harmful tobacco use and fewer people to quit tobacco use, even if the product itself poses less risk to the user than other products, it could be determined that the product poses a public health burden and would be kept off the market. Thus, the tobacco control field must pay close attention to the effects of e-cigarette use on initiation and cessation of combustible tobacco use, regardless of the effects of e-cigarettes on health outcomes. Although the studies reviewed had limitations, the committee was able to make seven conclusions:
Conclusion 16-1. There is substantial evidence that e-cigarette use increases risk of ever using combustible tobacco cigarettes among youth and young adults.
Conclusion 16-2. Among youth and young adult e-cigarette users who ever use combustible tobacco cigarettes, there is moderate evidence that e-cigarette use increases the frequency and intensity of subsequent combustible tobacco cigarette smoking.
Conclusion 16-3. Among youth and young adult e-cigarette users who ever use combustible tobacco cigarettes, there is limited evidence that e-cigarette use increases, in the near term, the duration of subsequent combustible tobacco cigarette smoking.
Conclusion 17-1. Overall, there is limited evidence that e-cigarettes may be effective aids to promote smoking cessation.
Conclusion 17-2. There is moderate evidence from randomized controlled trials that e-cigarettes with nicotine are more effective than e-cigarettes without nicotine for smoking cessation.
Conclusion 17-3. There is insufficient evidence from randomized controlled trials about the effectiveness of e-cigarettes as cessation aids compared with no treatment or to Food and Drug Administration–approved smoking cessation treatments.
Conclusion 17-4. While the overall evidence from observational trials is mixed, there is moderate evidence from observational studies that more frequent use of e-cigarettes is associated with an increased likelihood of cessation.
Taken together the evidence suggests that while e-cigarettes might cause youth who use them to transition to use of combustible tobacco products, they might increase adult cessation of combustible tobacco cigarettes.
HARM REDUCTION
The committee reviewed evidence from the sections discussed above to specifically look at what is known about e-cigarette exposures and health effects when compared with combustible tobacco cigarettes. The committee reached five conclusions.
Conclusion 18-1. There is conclusive evidence that completely substituting e-cigarettes for combustible tobacco cigarettes reduces users’ exposure to numerous toxicants and carcinogens present in combustible tobacco cigarettes.
Conclusion 18-2. There is substantial evidence that completely switching from regular use of combustible tobacco cigarettes to e-cigarettes results in reduced short-term adverse health outcomes in several organ systems.
Conclusion 18-3. There is no available evidence whether or not long-term e-cigarette use among smokers (dual use) changes morbidity or mortality compared with those who only smoke combustible tobacco cigarettes.
Conclusion 18-4. There is insufficient evidence that e-cigarette use changes short-term adverse health outcomes in several organ systems in smokers who continue to smoke combustible tobacco cigarettes (dual users).
Conclusion 18-5. There is moderate evidence that secondhand exposure to nicotine and particulates is lower from e-cigarettes compared with combustible tobacco cigarettes.
The evidence about harm reduction suggests that across a range of studies and outcomes, e-cigarettes pose less risk to an individual than combustible tobacco cigarettes.
The committee used population dynamic modeling to examine the possible effects of e-cigarette use at the population level. The specific time frame and magnitude of population health effects of e-cigarettes will depend on their impact on the rates of initiation and cessation of combus-
tible tobacco cigarettes and on their intrinsic harm. Any population health effect includes the possibility of some groups incurring harm (e.g., youth who initiate smoking combustible tobacco cigarettes), while others benefit (e.g., adult combustible tobacco cigarette users who completely quit or reduce smoking). As with other models of population health effects of tobacco use, the effects of changing cessation rates are seen earlier than effects of changing initiation rates, due to the lag time for serious chronic health effects of combustible tobacco cigarettes to manifest.
Under the assumption that the use of e-cigarettes increases the net cessation rate of combustible tobacco cigarette use among adults (i.e., the increase in permanent quitting offsets the potential relapse of former smokers because of e-cigarettes), the modeling projects that use of these products will generate a net public health benefit, at least in the short run. The harms from increased initiation by youth will take time to manifest, occurring decades after the benefits of increased cessation are seen. However, for long-range projections (e.g., 50 years out), the net public health benefit is substantially less and is negative under some scenarios. With the range of assumptions used, the model projects that there would be net public health harm in the short and long terms if the products do not increase combustible tobacco cessation in adults.
Factors that would maximize potential health benefits associated with these products include determining with more precision whether and under which conditions e-cigarettes could serve as an effective smoking cessation aid, discouraging their use among youth through standard tobacco control strategies such as education and access restrictions, and increasing their safety through data-driven product engineering and design.
RESEARCH RECOMMENDATIONS
Given the relatively short time that e-cigarettes have been used, it is understandable that the evidence base regarding their effects is limited. There is a great need for more evidence. Manufacturers will need to produce this research in a short amount of time if current statutory deadlines remain in place. Researchers from academia will also be involved directly (in contracts with manufacturers and in grants from government and others) in the generation of these data. Some types of research involve a long-term horizon; other important and informative research requires much less time to conduct. One type of research does not substitute for the other; a complete portfolio of research is needed. The committee understands that, in any new field, researchers struggle to conduct optimal research due to limitations of knowledge. Also, researchers feel the urgency to study an important new question and adapt what they know,
without complete adjustments in research design or methods sufficient to address the nuances of the problem. Finally, the rapidly changing nature of the devices has made comparisons among studies difficult.
The committee identified gaps in the literature in every aspect in its work and provides overarching categories of research needs and specific research suggestions within the final chapters of each of the three major sections of the report. These overarching categories include (1) address-
ing gaps in substantive knowledge and (2) improving research methods and quality through protocol and methods validation and development, including the use of appropriate study design. The six specific research recommendations and select suggestions can be found in Boxes S-3 , S-4 ,
and S-5 . The specific suggestions illustrate the range of priority research areas provided in the body of the report.
FINAL OBSERVATIONS
Much of the research on e-cigarettes suffers from methodological flaws, and many important areas have not yet been researched. Nonetheless, the committee found sufficient literature to suggest that, while there are risks associated with e-cigarettes, compared with combustible tobacco cigarettes, e-cigarettes contain fewer toxicants; can deliver nicotine in a manner similar to combustible tobacco cigarettes; show significantly less
biological activity in a number of in vitro, animal, and human systems; and might be useful as a cessation aid to smokers who use e-cigarettes exclusively. However, youth who begin with e-cigarettes are more likely to transition to combustible tobacco cigarette use and become smokers who may be at risk to suffer the known health burdens of combustible tobacco cigarettes. Moreover, although infrequent, e-cigarettes can explode, leading to burns and other injuries, and consumption of or dermal exposure to e-liquids is dangerous, even fatal.
More and better research on short- and long-term health effects of e-cigarettes, as well as their effects on initiation and cessation of combustible tobacco product use, will bring clarity to the question of whether e-cigarettes will prove to reduce harm or induce harm at the individual and the population levels. Given how rapidly the e-cigarette product marketplace and user population are changing, there will undoubtedly be many new issues, which are currently unknown and will require careful surveillance and scientific scrutiny. The approach taken by the committee to evaluate the health effects of e-cigarettes in this report is anticipated to provide a generalizable template for future evaluations of the evidence.
Millions of Americans use e-cigarettes. Despite their popularity, little is known about their health effects. Some suggest that e-cigarettes likely confer lower risk compared to combustible tobacco cigarettes, because they do not expose users to toxicants produced through combustion. Proponents of e-cigarette use also tout the potential benefits of e-cigarettes as devices that could help combustible tobacco cigarette smokers to quit and thereby reduce tobacco-related health risks. Others are concerned about the exposure to potentially toxic substances contained in e-cigarette emissions, especially in individuals who have never used tobacco products such as youth and young adults. Given their relatively recent introduction, there has been little time for a scientific body of evidence to develop on the health effects of e-cigarettes.
Public Health Consequences of E-Cigarettes reviews and critically assesses the state of the emerging evidence about e-cigarettes and health. This report makes recommendations for the improvement of this research and highlights gaps that are a priority for future research.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Argumentative Essay Sample E-Cigarette

Related Papers
Therapeutic advances in chronic disease
Riccardo Polosa
A growing body of scientific studies show that e-cigarettes may serve as an acceptable substitute for smoking tobacco cigarettes, thereby reducing or eliminating exposure to harmful elements in smoke. The success of e-cigarettes is such that sales of these products are rapidly gaining on traditional cigarettes. The rapidly evolving phenomenon is raising concerns for the health community, pharmaceutical industry, health regulators and state governments. Obviously, these products need to be adequately regulated, primarily to protect users. Depending on the form and intended scope, certain regulatory decisions may have diverse unintended consequences on public health and may face many different challenges. Ideally, before any regulations are enacted, the regulatory body will require sufficient scientific research to verify that a problem does exist, quantify the problem, explore all potential solutions including making no change at all, determine the possible consequences of each, and ...
Joy K Chakma
Electronic nicotine delivery systems (ENDS) or e-cigarettes are battery-powered devices used to smoke or 'vape', a flavoured solution containing a varying concentration of nicotine, an addictive chemical found in cigarettes and other forms of tobacco products. There are various types of ENDS devices. The most common type is an e-cigarette that produces an aerosolized mixture of the flavoured liquids and nicotine, which is inhaled by the user. Nicotine is considered as one of the most addictive substances. The rapidity at which it is introduced into the body, age of first exposure and the dosage administered all add to determine the potential risk of a person being addicted to it throughout life. The various flavours and attractive designs also add to the allure of these products to the young population. ENDS or e-cigarettes are manufactured in such a way to resemble conventional tobacco products such as cigarettes, pipes and cigars and common gadgets such as flash drives, flashlights or pens. Currently, there are more than 460 different e-cigarette brands with varied configuration of nicotine delivery available in the market, for example, cigar-likes (first generation), tank systems (second generation) and personal vaporizers (third generation) with over 7700 flavours. This makes collation of data on health effects more difficult for the generation of scientific evidence. Increasing use by youth and adolescents There is an increasing trend for the use of ENDS or e-cigarettes amongst the youth and adolescents in many countries where these products were introduced. E-cigarettes are the most commonly used nicotine products in the [Downloaded free from http://www.ijmr.org.in on Friday, May 31, 2019, IP: 49.248.114.2]
Hannah Farrimond
Background and aims The rapid increase in use of electronic cigarettes (e-cigarettes) has created an international policy dilemma concerning how to use these products. This study assesses the types of beliefs that e-cigarette users in the UK may hold concerning regulation. Design Qualitative thematic analysis of written answers to open-ended questions. Setting UK, questionnaire conducted by post, 44% recruited from online forums/56% non-online. Participants Fifty-five UK vapers, 55% male, mean age 46, 84% sole users of e-cigarettes, 95% vaping daily. Measurements Open-ended questions on regulatory and policy options. Findings ‘Protecting youth’ was seen as a fundamental regulatory requirement which should be achieved through childproofing, age limits, no advertising aimed at children and health warnings about addictiveness of nicotine, but not the restriction of flavours. There was little support for regulating e-cigarettes as medicines or limiting the strength of nicotine liquids. In terms of public use, participants argued against a blanket ban on public vaping given perceptions of a lack of scientific evidence of harm. However, they supported the principle of autonomy, that individuals and organizations have the right to restrict vaping. Some participants suggested banning vaping in places such as schools, hospitals or around food, in line with current smoking norms. Vapers’ regulatory positions were accompanied by political concerns about the use (and misuse) of scientific evidence. Conclusions With regard to regulation of e-cigarettes, issues that are salient to UK vapers may include the need for youth protection, regulation as medicines, strength of e-liquids, bans on public vaping and concerns about the misuse of scientific evidence.
Addiction (Abingdon, England)
Hayden McRobbie
We reviewed available research on the use, content and safety of electronic cigarettes (EC), and on their effects on users, to assess their potential for harm or benefit and to extract evidence that can guide future policy. Studies were identified by systematic database searches and screening references to February 2014. EC aerosol can contain some of the toxicants present in tobacco smoke, but at levels which are much lower. Long-term health effects of EC use are unknown but compared with cigarettes, EC are likely to be much less, if at all, harmful to users or bystanders. EC are increasingly popular among smokers, but to date there is no evidence of regular use by never-smokers or by non-smoking children. EC enable some users to reduce or quit smoking. Allowing EC to compete with cigarettes in the market-place might decrease smoking-related morbidity and mortality. Regulating EC as strictly as cigarettes, or even more strictly as some regulators propose, is not warranted on curren...
International Journal of Environmental Research and Public Health
Giorgio Romagna , Konstantinos Farsalinos , Αλκέτα Σπύρου
The International Journal of Tuberculosis and Lung Disease
Tara Bam , I. Berezhnova
Eric N Lindblom
International Journal of Drug Policy
Riccardo Polosa , Pasquale Caponnetto , Daniela Saitta , David Sweanor
Abstract Background: The aim of this study was to identify and differentiate socially shared accounts of e-cigarette use (vaping) using Q-methodology, combining factor analysis with qualitative comments. Methods: Seventy statements on e-cigarettes, drawn from media, academic and online discussions, were sorted by participants along a continuum of agreement/disagreement, commenting on strongly ranked items. Each participant thus created their own ‘account’ of their vaping. A by-person correlation matrix of the sorts was conducted, then factor analysed, to identify similar accounts (p<0.01). Fifty-five UK vapers participated by post, 55% male, mean age of 46, 84% only vaping/16% vaping and smoking, 95% vaping daily. Results: Three accounts of e-cigarettes were identified. The first two were associated with having quit smoking; the third with ongoing tobacco smoking and vaping. In Factor One, ‘Vaping as Pleasure’, vaping was characterized as enjoyable, with long-term use envisaged and a medical model of vaping rejected. Factor One participants also held a strong vaping identity and were politically motivated to maintain the rights of adults to vape. In Factor Two, ‘Vaping as Medical Treatment’, vaping was understood as a pragmatic choice about how to medicate one’s smoking addiction, with the aim being to treat and ultimately reduce nicotine dependence. In Factor Three, ‘Ambivalent E-Cigarette Use’, participants reported fewer benefits and harboured more negative beliefs about e-cigarettes; they also strongly rejected a vaper identity, having no interest in online forums or being labelled a ‘vaper’ themselves. Conclusion: The UK e-cigarette users in this sample were not a homogeneous group; differing in their beliefs, motivations for use, identity and political interest. In particular they diverged on whether they accepted a medicalized account of vaping and identified as a vaper. Public health messages targeted to one group of e-cigarette users may not resonate with others.
Tobacco Induced Diseases
Muhammad Aziz Rahman
Background Electronic cigarettes (e-cigarettes) are battery-powered devices that vaporize a liquid solution to deliver a dose of inhaled nicotine to the user. There is ongoing debate regarding their regulation. Objectives This comprehensive narrative review aimed to discuss key issues including usage patterns, health effects, efficacy in smoking cessation and regulatory concerns with a view to informing future regulation and research agendas. Methods PubMed, Scopus and Web of Science databases were searched using the terms (electronic cigarettes OR e-cigarettes) for articles in English, relevant to humans and published during January 2009-January 2014. Results The literature search revealed 37 relevant articles. Findings suggest that e-cigarettes are mostly used by middle-aged current smokers, particularly males, to help them for quitting or for recreation. E-cigarettes contain very low levels of multiple toxic substances such as formaldehyde and acrolein, but these levels are many times lower than those found in cigarettes. They were found to have effectiveness in aiding smoking cessation to a limited degree. Debate continues regarding regulating their use for cessation versus heavy restrictions to control recreational use on the basis that it perpetuates nicotine addiction. Conclusions The cytotoxicity and long term health effects of e-cigarettes are unknown. Nevertheless the e-cigarette market continues to expand, largely driven by middle-aged smokers who claim to be using e-cigarettes in an attempt to reduce or quit smoking. E-cigarettes may have some potential as smoking cessation aids and, in the researchers? view, should therefore be subject to further research and regulation similar to other nicotine replacement therapies. The complete article is available as a provisional PDF. T
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Tobacco control
Noel Brewer
Food and Drug Law Journal
British dental journal
Devina Worsley , Zoe Marshman
Harm Reduction Journal
Riccardo Polosa , Pasquale Caponnetto
Jacques Le Houezec , Konstantinos Farsalinos
Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine
Lena Gray , Ted Niemiec , Lavaughn Palma-Davis
BMJ Case Reports
Mir Inzamam
Nicotine and Tobacco Research
Elisha R Oliver, PhD
Expert Review of Respiratory Medicine
Pasquale Caponnetto , Gabriella Papale , Davide Campagna
Husnul Khotimah Matoha
Innovative Publication
IP Innovative Publication Pvt. Ltd.
Robert McMillen
Louise cyferman
Lawrence Gostin
Merlyn Griffiths
Tobacco induced diseases
Riccardo Polosa , Jaymin Morjaria , Pasquale Caponnetto , Massimo Caruso , Davide Campagna
Coral Gartner
Judith Dean
Preventive Medicine
Martin Døssing
Journal of Medical Case Reports
Riccardo Polosa , Pasquale Caponnetto , Davide Campagna
Rachel A Barry
Otolaryngology -- Head and Neck Surgery
Vani Simmons
Current Cardiovascular Risk Reports
Alayna P Tackett
Society for Research on Nicotine and Tobacco
Duygu Sarıkaya
Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco
Michael Fiore , Kevin Walton
American journal of preventive medicine
Rebecca Bunnell
Arja Rimpelä
Guy Richards
divine macaranas
Open journal of preventive medicine
Cam Escoffery
Journal of Health Inequalities
Lukasz Gruszczynski
Therapeutic advances in drug safety
Riccardo Polosa , Konstantinos Farsalinos
Martin Dockrell , Rosemary Hiscock
Jamien Bontigao
Adele Phillips
Richard Bonnie
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Home — Essay Samples — Law, Crime & Punishment — Smoking Ban — E-Cigarettes and Vaping Epidemic across the United States
E-cigarettes and Vaping Epidemic Across The United States
- Categories: Smoking Ban
About this sample

Words: 1155 |
Published: Apr 8, 2022
Words: 1155 | Pages: 3 | 6 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Law, Crime & Punishment

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 615 words
4 pages / 1817 words
6 pages / 2592 words
2 pages / 842 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Smoking Ban
In the "should smoking be illegal argumentative" debate, one of the primary concerns is the well-known harmful effects of cigarettes on the human body. Many people are aware that smoking cigarettes is detrimental. Cigarettes [...]
Smoking has numerous health effects, both short-term and long-term. Some of the short-term effects include bad breath, yellow teeth, and decreased sense of taste and smell. The long-term effects, however, are much more severe. [...]
Good afternoon, ladies and gentlemen. Today, I would like to talk to you about the dangers of smoking and the impact it has on individuals and society as a whole. Smoking is a prevalent habit that has been around for centuries, [...]
Smoking has been a prevalent issue in society for decades, and despite the numerous health warnings and anti-smoking campaigns, it continues to be a significant public health concern. Anti-smoking quotes have been used as a [...]
For years there has been conflicting research whether smoking should be banned or not and it is a significant issue today. Many people have given up smoking while others still continue to smoke. Smoking is the inhalation and [...]
This article talks about how the “number of children admitted to hospital with severe asthma” has decreased by 12% in the first year after the ban on smoking in public places. It is also thought that people are opting for smoke [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Introduction
- Conclusions
- Article Information
Panel A shows unadjusted weighted proportions aggregated by quarter (Q). Panel B shows modeled monthly time trends: lines represent modeled weighted prevalence by monthly survey wave (modeled nonlinearly using restricted cubic splines, 5 knots), shaded bands represent SEs, and points represent observed weighted prevalence by quarter. Vertical lines indicate the timing of the start of the e-cigarette, or vaping product, use-associated lung injury (EVALI) outbreak (March 2019), 9 COVID-19 pandemic (March 2020), and the rapid increase in prevalence of disposable vaping among young people in England (June 2021). 14 Corresponding figures excluding don’t know responses are provided in eFigure 1 in Supplement 1 .
a Quarter 4 2014 includes data from November to December only.
Graphs show data by age (A), occupational social grade (B; ABC1 refers to managerial, professional, or intermediate workers, and C2DE refers to skilled manual workers, semiskilled and unskilled manual workers, state pensioners, casual and lowest grade workers, and those who are unemployed with state benefits only), and vaping status (C). Lines represent point estimates from logistic regression allowing an interaction between age and survey wave, modeled nonlinearly using restricted cubic splines (5 knots). Shaded bands represent SEs. Points represent observed weighted prevalence by quarter. From left to right, vertical lines indicate the timing of the start of the e-cigarette, or vaping product, use-associated lung injury outbreak (March 2019), 9 COVID-19 pandemic (March 2020), and the rapid increase in prevalence of disposable vaping among young people in England (June 2021). 14 Figures for trends in the perception of e-cigarettes as equally harmful, more harmful, or don’t know are shown in eFigure 2 in Supplement 1 . Corresponding figures excluding those who responded “don’t know” from the sample are shown in eFigure 3 in Supplement 1 .
eAppendix. Literature Review
eReferences
eTable 1. Harm Perceptions, Aggregated Across Survey Waves, Excluding Don’t Know Responses (Unweighted n=24,088)
eFigure 1. Harm Perceptions of e-Cigarettes Compared With Cigarettes Among Adults Who Smoke in England, November 2014 to June 2023, Excluding Don’t Know Responses (n=24,088)
eTable 2. Changes in Harm Perceptions From the Start to the End of the Study, Excluding Don’t Know Responses
eFigure 2. Trends in Harm Perceptions of e-Cigarettes Compared With Cigarettes Among Adults Who Smoke in England, by Age (A-C), Occupational Social Grade (D-F), and Vaping Status (G-I), November 2014 to June 2023: Equally Harmful, More Harmful, and Don’t Know
eFigure 3. Trends in Harm Perceptions of e-Cigarettes Compared With Cigarettes Among Adults Who Smoke in England, by Age (A-C), Occupational Social Grade (D-F), and Vaping Status (G-I), November 2014 to June 2023, Excluding Don’t Know Responses
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Jackson SE , Tattan-Birch H , East K , Cox S , Shahab L , Brown J. Trends in Harm Perceptions of E-Cigarettes vs Cigarettes Among Adults Who Smoke in England, 2014-2023. JAMA Netw Open. 2024;7(2):e240582. doi:10.1001/jamanetworkopen.2024.0582
Manage citations:
© 2024
- Permissions
Trends in Harm Perceptions of E-Cigarettes vs Cigarettes Among Adults Who Smoke in England, 2014-2023
- 1 Department of Behavioural Science and Health, University College London, London, United Kingdom
- 2 SPECTRUM Consortium, Edinburgh, United Kingdom
- 3 Department of Addictions, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, United Kingdom
Question How have harm perceptions of electronic cigarettes (e-cigarettes) compared with combustible cigarettes changed since 2014 among adults who smoke in England?
Findings This survey study of 28 393 adults who smoke found that harm perceptions of e-cigarettes have worsened substantially over the last decade, such that in 2023, most (57.0%) believed e-cigarettes to be equally (33.7%) or more (23.3%) harmful than cigarettes. The timing of the 2 most notable changes in harm perceptions coincided with the e-cigarette, or vaping product, use-associated lung injury outbreak in 2019 and the recent increase in youth vaping in England since 2021.
Meaning These findings provide evidence of substantial misperceptions about the harms of vaping compared with smoking and underscore the need to clearly communicate the risks so that adults who smoke can make informed choices about the nicotine products they use.
Importance Electronic cigarettes (e-cigarettes) are less harmful to users than combustible cigarettes. However, public health and media reporting have often overstated the potential risks of e-cigarettes, and inaccurate perceptions of the harms of vaping relative to smoking are pervasive.
Objective To examine time trends in harm perceptions of e-cigarettes compared with combustible cigarettes among adults who smoke.
Design, Setting, and Participants This nationally representative monthly cross-sectional survey study was conducted from November 2014 to June 2023 in England. Participants were adults who currently smoke.
Main Outcomes and Measures Participants were asked whether they thought e-cigarettes were less harmful, equally harmful, or more harmful than cigarettes, or did not know, with the proportion responding less harmful (vs all other responses) as the primary outcome. Logistic regression was used to test associations between survey wave and participants’ perceptions of the harms of e-cigarettes.
Results Data were collected from 28 393 adults who smoke (mean [SD] age, 43.5 [17.3] years; 13 253 [46.7%] women). In November 2014, 44.4% (95% CI, 42.0%-46.8%) thought e-cigarettes were less harmful than cigarettes, 30.3% (95% CI, 28.2%-32.6%) thought e-cigarettes were equally harmful, 10.8% (95% CI, 9.4%-12.3%) thought they were more harmful, and 14.5% (95% CI, 12.9%-16.4%) did not know. However, by June 2023, the proportion who thought e-cigarettes were less harmful had decreased by 40% (prevalence ratio, 0.60; 95% CI, 0.55-0.66), and the proportion who thought e-cigarettes were more harmful had more than doubled (prevalence ratio, 2.16; 95% CI, 1.84-2.54). Changes over time were nonlinear: late 2019 saw a sharp decline in the proportion who thought e-cigarettes were less harmful and increases in the proportions who thought they were equally or more harmful. These changes were short-lived, returning to pre-2019 levels by the end of 2020. However, perceptions worsened again from 2021 up to the end of the study period: the proportion who thought e-cigarettes were more harmful increased to a new high, and the proportion who thought e-cigarettes were less harmful decreased to levels comparable to those in late 2019. As a result, in June 2023, the perception that e-cigarettes were equally as harmful as cigarettes was the most commonly held view among adults who smoke (33.7%; 95% CI, 31.4%-36.1%), with roughly similar proportions perceiving e-cigarettes to be less (26.7%; 95% CI, 24.6%-28.9%) and more (23.3%; 95% CI, 21.1%-25.7%) harmful.
Conclusions and Relevance This survey study of adults who smoke in England found that harm perceptions of e-cigarettes have worsened substantially over the last decade, such that most adults who smoked in 2023 believed e-cigarettes to be at least as harmful as cigarettes. The timing of the 2 most notable changes in harm perceptions coincided with the e-cigarette, or vaping product, use-associated lung injury outbreak in 2019 and the recent increase in youth vaping in England since 2021.
Electronic cigarettes (e-cigarettes) are effective for helping people to stop smoking 1 and are less harmful than combustible cigarettes (referred to hereafter as cigarettes). 2 However, many adults who smoke in England (as in many other countries) believe that e-cigarettes are at least as harmful to health as cigarettes, 2 - 4 which can dissuade adults who smoke from switching to e-cigarettes (and thus reducing their exposure to harmful toxicants). 2 Several factors may have contributed to increased confusion about the harms of e-cigarettes relative to cigarettes over recent years (see the eAppendix in Supplement 1 for a full literature review). Media reporting often has overstated the risks of e-cigarettes, 5 , 6 and evidence suggests that this could exacerbate misperceptions. 2 , 7 There has been comparatively little reporting on the deaths caused by smoking; for example, smoking kills approximately 75 000 people each year in England. 8 Risk messages such as those provided by public health organizations can also change harm perceptions of e-cigarettes. 2 , 7 For example, in 2019, there was an outbreak of acute lung injuries that were primarily attributable to vaping contaminated tetrahydrocannabinol products; yet, before the cause was identified, the Centers for Disease Control and Prevention misattributed this to vaping generally and labeled the disease e-cigarette, or vaping product, use-associated lung injury (EVALI). 9 The following year, COVID-19, a disease that primarily impairs the respiratory system, prompted concerns that e-cigarette use may increase infection risk and disease severity 10 - 12 ; however, there is little evidence this was true. 11 , 13 Several studies documented short-term increases in the harm perceptions of e-cigarettes following the EVALI outbreak. 2 How harm perceptions of e-cigarettes have continued to change beyond 2020, in the context of the COVID-19 pandemic (since March 2020) and the growing concern about youth vaping (use of disposable e-cigarettes among young people in England has grown rapidly since June 2021, 14 leading to calls for a ban on disposable vapes 15 and widespread news coverage stating potential risks to youth), and the extent to which changes differ between key population subgroups, is not known.
It is important to understand whether there have been changes over time in perceptions of the relative harms of different nicotine products among adults who smoke, because this will have implications for accurate messaging and support. Identifying groups with particularly poor or worsening harm perceptions can inform targeted campaigns to address misperceptions, particularly because campaigns are perceived to negatively portray vaping. 16 Using data from a nationally representative survey in England, this study aimed to examine how harm perceptions of e-cigarettes compared with cigarettes have changed over time among adults who currently smoke, and the extent to which changes have differed by age, socioeconomic position, and vaping status (variables known to be associated with smoking, vaping, and harm perceptions of e-cigarettes vs cigarettes). 17 - 20
The study protocol and analysis plan for this survey study were preregistered on Open Science Framework 21 and were followed without amendment. Ethical approval for the Smoking and Alcohol Toolkit Study was granted originally by the University College London ethics committee. The data are collected by Ipsos Mori and are anonymized when received by University College London. All participants provided informed verbal consent. The study conformed to the American Association for Public Opinion Research ( AAPOR ) reporting guidelines for survey research.
Data were drawn from the ongoing Smoking Toolkit Study, a monthly cross-sectional survey of a representative sample of adults in England. 22 The study uses a hybrid of random probability and simple quota sampling to select a new sample of approximately 1700 adults each month. Comparisons with other national surveys and sales data indicate that sociodemographic characteristics, smoking prevalence, and cigarette consumption are nationally representative. 22 , 23
Data were initially collected through face-to-face computer-assisted interviews. However, social distancing restrictions under the COVID-19 pandemic meant that no data were collected in March 2020, and data from April 2020 onward were collected via telephone. The telephone-based data collection uses sampling and weighting approaches similar to the face-to-face interviews, and comparisons of the 2 data collection modalities indicate good comparability. 24 - 26
For the present study, we used data from survey respondents between November 2014 (the first wave to assess harm perceptions of e-cigarettes) and June 2023 (the most recent data available at the time of analysis). We restricted our sample to those aged 18 years or older who reported current smoking (see the Measures section), because the item assessing harm perceptions of e-cigarettes was only asked to those who smoke.
Smoking status was assessed with the question, “Which of the following best applies to you? Please note we are referring to cigarettes and other kinds of tobacco that you set light to and NOT electronic or ‘heat-not-burn’ cigarettes?: (a) I smoke cigarettes (including hand-rolled) every day; (b) I smoke cigarettes (including hand-rolled), but not every day; (c) I do not smoke cigarettes at all, but I do smoke tobacco of some kind (eg, pipe, cigar, or shisha); (d) I have stopped smoking completely in the last year; (e) I stopped smoking completely more than a year ago; (f) I have never been a smoker (ie, smoked for a year or more).” Responses a, b, and c were considered current smoking. Those who responded d, e, or f were excluded from the sample.
Harm perceptions of e-cigarettes was assessed with the question, “Compared to regular cigarettes, do you think electronic cigarettes are more, less, or equally harmful to health?” Response options were “more harmful,” “less harmful,” “equally harmful,” or “don’t know.” We analyzed the proportion responding less harmful (vs all other responses) as our primary outcome, consistent with current evidence that e-cigarettes are less harmful than cigarettes, 2 and the proportions responding equally harmful (vs all other), more harmful (vs all other), and don’t know (vs all other) as secondary outcomes. We conducted sensitivity analyses with don’t know responses excluded.
Age was categorized as 18 to 34 years, 35 to 64 years, and 65 years or older. Occupational social grade was categorized as ABC1 (managerial, professional, or intermediate) and C2DE (skilled manual workers, semiskilled and unskilled manual workers, state pensioners, casual and lowest grade workers, and unemployed with state benefits only).
Vaping status was assessed with a series of questions that ask participants whether they are using an e-cigarette or vaping device to help them stop smoking, cut down the amount smoked, in situations when smoking is not permitted, or for any other reason at all. Those who reported e-cigarette use in response to any of these questions were considered current vapers.
Data were analyzed using R statistical software version 4.2.2 (R Project for Statistical Computing). We excluded participants with missing data on harm perceptions.
The Smoking Toolkit Study uses raking to weight the sample to match the population in England on age, social grade, region, housing tenure, ethnicity, and working status within sex. This profile is determined monthly by combining data from the UK Census, the Office for National Statistics midyear estimates, and the annual National Readership Survey. 22 The following analyses used weighted data.
We used logistic regression to test associations between survey wave and perception of e-cigarettes as (a) less harmful than cigarettes (primary outcome), and (b) equally harmful, (c) more harmful, and (d) don’t know (secondary outcomes). Survey wave was modeled using restricted cubic splines with 5 knots, to allow relationships with time to be flexible and nonlinear.
To explore moderation by age, occupational social grade, and vaping status, we repeated the models including the interaction between the moderator of interest and survey wave, thus allowing time trends to differ across subgroups. Each interaction was tested in a separate model. Two-sided P < .05 was considered statistically significant.
We used estimates from our models to plot the estimated prevalence of each harm perception over the study period (overall and by moderating variables), alongside unmodeled observed (weighted) data aggregated by quarter (to increase sample size contributing to each data point and reduce noise). We also used our modeled estimates to derive prevalence ratios (PRs) for the change in prevalence across the whole time series (June 2023 vs November 2014) alongside 95% CIs calculated using bootstrapping.
Of 169 433 participants surveyed in eligible waves, 28 393 (16.8%) reported current smoking. There were no missing data on e-cigarette harm perceptions (or age, occupational social grade, or vaping status), leaving a final sample for analysis of 28 393 adults who smoke (mean [SD] age, 43.5 [17.3] years; 13 253 [46.7%] women; 15 415 [54.3%] social grades C2DE; 5879 [20.7%] reported current vaping).
Table 1 shows descriptive data on harm perceptions, aggregated across survey waves (corresponding estimates excluding those who responded don’t know from the sample are shown in eTable 1 in Supplement 1 ). Overall, 35.2% (95% CI, 34.6%-35.8%) of adults who smoke perceived e-cigarettes to be less harmful than cigarettes, 36.7% (95% CI, 36.0%-37.3%) said it was equally harmful, 13.4% (95% CI, 12.9%-13.8%) said it was more harmful, and 14.8% (95% CI, 14.3%-15.2%) did not know. The proportion who thought e-cigarettes were less harmful was higher among those who currently vaped (56.7% [95% CI, 55.4%-58.1%] vs 29.4% [95% CI, 28.8%-30.1%] among those who did not currently vape), those from more advantaged social grades ABC1 (41.9% [95% CI, 41.0%-42.9%] vs 30.7% [95% CI, 29.9%-31.5%] among social grades C2DE), and those aged 35 to 64 years (37.6% [95% CI, 36.7%-38.5%] vs 34.1% [95% CI, 33.1%-35.0%] among those aged 18-34 years and 29.2% [95% CI, 95% CI, 27.7%-30.7%] among those aged ≥65 years). Younger participants (18-34 years) were more likely than middle-aged (35-64 years) and older (≥65 years) participants to perceive e-cigarettes as equally or more harmful than cigarettes, whereas older participants (≥65 years) were more likely to say they did not know. Approximately one-third (34.9% [95% CI, 33.6%-36.2%]) of dual users (who both smoked and vaped) reported perceiving that e-cigarettes were equally or more harmful than cigarettes.
Figure 1 A shows descriptive data on e-cigarette harm perceptions across the study period, aggregated by quarter (corresponding figures excluding don’t know responses are provided in eFigure 1 in Supplement 1 ). Models revealed significant changes in harm perceptions between the start and end of the study period ( Table 2 and Table 3 ) (corresponding estimates excluding those who responded don’t know from the sample are shown in eTable 2 in Supplement 1 ). In November 2014, when e-cigarette harm perceptions were first assessed, the most common perception among adults who smoke was that e-cigarettes were less harmful than cigarettes (44.4%; 95% CI, 42.0%-46.8%), similar to the proportions perceiving e-cigarettes to be equally harmful (30.3%; 95% CI, 28.2%-32.6%) or more harmful (10.8%; 95% CI, 9.4%-12.3%) combined, with 14.5% (95% CI, 12.9%-16.4%) saying they did not know. However, by June 2023, the proportion who thought e-cigarettes were less harmful had decreased by 40% (PR, 0.60; 95% CI, 0.55-0.66) and the proportion who thought they were more harmful had more than doubled (PR, 2.16; 95% CI, 1.84-2.54). Hence, in June 2023, the perception that e-cigarettes were equally as harmful as cigarettes was the most commonly held view among adults who smoke (33.7%; 95% CI, 31.4%-36.1%), with roughly similar proportions perceiving e-cigarettes to be less (26.7%; 95% CI, 24.6%-28.9%) and more (23.3%; 95% CI, 21.1%-25.7%) harmful.
Changes in harm perceptions over time were nonlinear ( Figure 1 B). From November 2014 to July 2019, the proportion of adults who smoke who thought e-cigarettes were less harmful than cigarettes declined steadily to 33.2% (95% CI, 32.0%-34.5%) and the proportion who thought they were equally harmful increased to 42.5% (95% CI, 41.1%-43.8%). The proportions who thought they were more harmful or who did not know were relatively stable up to the end of 2016; the former increased over subsequent years to a high of 14.1% (95% CI, 13.1%-15.1%) in April 2019, and the latter decreased to a low of 8.9% (95% CI, 8.3%-9.7%) in October 2018.
Inspection of the unmodeled data points (ie, observed weighted prevalence by quarter, shown as points in Figure 1 and Figure 2 ) suggests there was then a marked shift in perceptions in late 2019: a sharp decline in the proportion who thought e-cigarettes were less harmful than cigarettes to a low of 25.1% (95% CI, 21.0%-29.3%) in quarter 1 of 2020 and increases in the proportions who thought they were equally or more harmful, reaching highs of 50.6% (95% CI, 45.7%-55.5%) in quarter 1 of 2020 and 19.7% (95% CI, 16.6%-22.9%) in quarter 4 of 2019 ( Figure 1 B). Changes in the proportions who thought e-cigarettes were less or more harmful were short-lived, returning to pre-2019 levels by the end of 2020. However, the proportion who thought e-cigarettes were equally harmful decreased to below 2018 levels and remained lower, offset by an increase in the proportion who did not know how the harms of e-cigarettes compared with cigarettes in quarter 2 of 2020 ( Figure 1 B). From 2021 to the end of the study period in mid-2023, the proportion who thought e-cigarettes were more harmful than cigarettes increased to a new high (surpassing the previous peak in the unmodeled data points in late 2019), the proportion who thought they were less harmful decreased to levels comparable to those in late 2019, the proportion who thought they were equally harmful was stable, and the proportion who did not know declined ( Figure 1 B).
The decline over the study period in the proportion who thought e-cigarettes were less harmful than cigarettes was similar across age groups ( Figure 2 A). The decline in the proportion who thought e-cigarettes were equally harmful since 2019 was most pronounced among the oldest group (≥65 years) and least pronounced among the youngest group (18-34 years; P for interaction = .001) (eFigure 2A in Supplement 1 ). The increase in the proportion who thought e-cigarettes were more harmful since 2021 was most pronounced among the youngest group and was absent in the oldest group ( P for interaction = .001) (eFigure 2B in Supplement 1 ).
The decline in the proportion who thought e-cigarettes were less harmful than cigarettes since 2021 was more pronounced among social grades ABC1, with less change observed for C2DE ( P for interaction = .005) ( Figure 2 B). Over the same period, there was also an increase in the proportion who thought e-cigarettes were equally harmful among social grades ABC1 but not C2DE ( P for interaction = .003) (eFigure 2D in Supplement 1 ). By the end of the study period, the inequality gap in harm perceptions had closed, such that those from social grades ABC1 had perceptions similar to those from C2DE.
There were similar declines in the proportion who thought e-cigarettes were less harmful by vaping status across the period ( Figure 2 C). Notably, the proportion who believed e-cigarettes were less harmful was consistently lower among those who did not vape, and only 19.0% (95% CI, 17.0%-21.3%) of this group thought this by June 2023. There was an increase in the proportion who thought e-cigarettes were equally harmful since 2021 among those who currently vaped but no change among those who smoked but did not vape (eFigure 2G in Supplement 1 ). As a result, in June 2023, 33.4% (95% CI, 30.7%-36.3%) of participants who smoked but did not vape thought e-cigarettes were equally harmful as cigarettes, 27.7% (95% CI, 24.9%-30.6%) thought they were more harmful, and 19.9% (95% CI, 17.7%-22.3%) were unsure. Corresponding figures excluding those who responded don’t know from the sample are shown in eFigure 3 in Supplement 1 .
This survey study found that among adults who smoke in England, harm perceptions of e-cigarettes compared with cigarettes have worsened considerably over the past decade. In 2014, the most common perception was that e-cigarettes were less harmful than cigarettes. However, by June 2023, the proportion who thought e-cigarettes were less harmful had decreased by 40% and the proportion who thought they were more harmful had more than doubled. Although perceptions were generally more positive among those aged 35 to 64 years, those from more advantaged social grades, and those who currently vaped, deterioration was observed across all subgroups. As a result, only a minority (26.7%) of adults who smoke now think e-cigarettes are less harmful than cigarettes, including only 19.0% of smokers who do not vape, who would most benefit from switching to a reduced harm product. More than one-half (57.0%) of all adults surveyed think e-cigarettes are equally (33.7%) or more (23.3%) harmful than cigarettes. Among those who did not vape, 61.1% overall think e-cigarettes are equally (33.4%) or more (27.7%) harmful than cigarettes, and 19.9% are unsure.
Changes over time were nonlinear. Consistent with previous studies, 2 , 27 , 28 including from the same data set up to 2019, 4 we observed a sharp decline in late 2019 in the proportion who thought e-cigarettes were less harmful than cigarettes and increases in the proportions who thought e-cigarettes were equally or more harmful. This coincided with the timing of the EVALI outbreak, which was at its peak in September 2019. 9 EVALI cases declined to virtually zero by February 2020, at which point the Centers for Disease Control and Prevention stopped publishing updates on case numbers. 9 Likewise, changes in the proportions who thought e-cigarettes were less or more harmful were short-lived, returning to pre-2019 levels by the end of 2020. 27 Interestingly, changes in harm perceptions around the timing of EVALI appeared similar across age groups, despite EVALI predominantly affecting young people 9 and this being highlighted in media coverage at the time. 5
Following EVALI, the COVID-19 pandemic did not coincide with substantial changes in harm perceptions of e-cigarettes, with the only notable change being an increase in don’t know responses. This may be linked to an increase in confusion about public health risks resulting from misinformation transmitted during the pandemic. 29 However, perceptions worsened again from 2021 to the end of the study period. The proportion who thought e-cigarettes were more harmful increased to a new high (surpassing the previous peak in late 2019), and the proportion who thought they were less harmful decreased to levels comparable to those from late 2019. These changes coincided with the timing of concerns about an increase in youth vaping in England 30 since new disposable e-cigarettes have become popular. 14 This trend has been widely reported in the media (with a substantial increase in news reporting of vaping in 2022 and 2023) 31 and is a priority issue for policymakers 32 and practitioners. 15 We observed a clear age gradient in changing harm perceptions since 2021, with the increase in the proportion who thought e-cigarettes were more harmful than cigarettes most pronounced among those younger than 35 years and absent in those older than 65 years. This aligns with the emphasis on risks to young people in reports on youth vaping. 15 It suggests there is a disconnect between young people’s risk perceptions of e-cigarettes and their behavior (ie, that use of e-cigarettes is more common among younger age groups, despite a larger proportion thinking they are at least as harmful as smoking).
The deterioration in evidence-based harm perceptions since 2021 was also much more prominent among those from more advantaged social grades, with little change among less advantaged social grades. Overall, the more advantaged social grades held more positive views of e-cigarettes’ relative harms. However, the decline since 2021 closed the inequality gap, bringing their perceptions in line with the (more negative) views of those from less advantaged social grades. Although reducing inequalities is important, it does not improve public health unless it is achieved by correcting misperceptions in the less advantaged group, rather than worsening in the more advantaged group.
These findings have important implications for public health. Misperceptions about the risks of e-cigarettes compared with cigarettes are a health risk in and of themselves. If people who smoke think vaping is equally or more harmful than smoking, they may be less inclined to try and switch to vaping, leaving them using a more harmful product. 2 In April 2023, the English government announced a national swap to stop campaign, which aims to offer 1 million people a free vaping starter kit with behavioral support, to help them quit smoking. 33 Strategies such as these could be undermined if people who smoke are unwilling to try vaping because of safety concerns. In addition, if people who both smoke and vape (dual users) think the risks are similar, they may not see any benefit of stopping smoking and instead continue both behaviors. Our data suggest that 1 in 2 dual users now think e-cigarettes are equally or more harmful than cigarettes, so there is substantial opportunity to correct misperceptions. Similarly, if young vapers who have never smoked think the risks are similar, they may be equally likely to start smoking as to start vaping. To date, smoking prevalence among young people in England has remained low despite an increase in vaping prevalence, 2 although there are warning signs that the decline in smoking may have leveled off or reversed in recent years. 2 , 34 There is a need to clearly communicate the risks of vaping compared with smoking to ensure this pattern does not change.
This study had several limitations. Only adults who currently smoke were asked about harm perceptions of e-cigarettes, so we were unable to explore changes among nonsmokers or youth. We included all adults who reported current smoking but did not separate noncigarette tobacco (eg, cigars and pipes) users, who may hold different harm perceptions compared with those who smoke cigarettes, because of their small sample size. In addition, findings are unlikely to generalize beyond England; cross-national comparisons could help to understand potential factors contributing to changing vaping perceptions. Although we speculated on the potential causes of the changes in harm perceptions we observed, further research (eg, qualitative) is required to provide deeper insight into the factors that have caused people’s perceptions of e-cigarettes to change and why changes have been different across population subgroups. Further research could explore differences in intersectional subgroups (eg, age by socioeconomic position) to gain more nuanced insights into unequal harm perceptions.
Harm perceptions of e-cigarettes have worsened substantially over the last decade, such that the vast majority of adults who smoke and do not vape in England do not believe e-cigarettes are less harmful than cigarettes. The timing of the most notable changes in harm perceptions coincided with the EVALI outbreak and the recent increase in youth vaping.
Accepted for Publication: January 7, 2024.
Published: February 28, 2024. doi:10.1001/jamanetworkopen.2024.0582
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Jackson SE et al. JAMA Network Open .
Corresponding Author: Sarah E. Jackson, PhD, Department of Behavioural Science and Health, University College London, 1-19 Torrington Pl, London WC1E 7HB, United Kingdom ( [email protected] ).
Author Contributions: Dr Jackson had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Jackson, Tattan-Birch, Cox, Shahab, Brown.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Jackson, Shahab.
Critical review of the manuscript for important intellectual content: Tattan-Birch, East, Cox, Shahab, Brown.
Statistical analysis: Jackson .
Obtained funding: Shahab, Brown.
Supervision: Brown.
Conflict of Interest Disclosures: Dr Shahab reported being a Higher Education Funding Council for England–funded member of staff at University College London; receiving honoraria for talks, an unrestricted research grant, and travel expenses to attend meetings and workshops from Pfizer; receiving an honorarium to sit on advisory panel from Johnson & Johnson; acting as paid reviewer for grant awarding bodies and as a paid consultant for health care companies; and receiving research funding from the government, a community-interested company (National Centre for Smoking Cessation), and other charitable sources outside the submitted work. Dr Brown reported receiving grants from Johnson & Johnson and Pfizer outside the submitted work. No other disclosures were reported.
Funding/Support: Cancer Research UK (PRCRPG-Nov21\100002) funded the Smoking Toolkit Study data collection and the salaries of Drs Jackson, Tattan-Birch, and Cox. Dr East is supported by a fellowship from the Society for the Study of Addiction.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

COMMENTS
This Surgeon General's report focuses on the history, epidemiology, and health effects of e-cigarette use among youth and young adults; the companies involved with marketing and promoting these products; and existing and proposed public health policies regarding the use of these products by youth and young adults.
The electronic cigarette (e-cigarette), for many considered as a safe alternative to conventional cigarettes, has revolutionised the tobacco industry in the last decades. In e-cigarettes, tobacco combustion is replaced by e-liquid heating, leading some manufacturers to propose that e-cigarettes have less harmful respiratory effects than tobacco consumption. Other innovative features such as ...
Essay On E Cigarettes. The question should not be if e-cigarettes are bad or not, but if they are better for you than the alternative. Many people believe that since vaporizers have only been around for a little over ten years, people do not know what the long term effects from them will be. Cigarettes have thousands of chemicals in them, with ...
Persuasive Essay Sample about e-cigarettes: Smoking tobacco is probably one of the worst habits humankind has developed. Originating as a tradition of Nat...
Especially the long-term effects of using e-cigarettes or being exposed to them are yet unknown. Nevertheless, the evidence is clear that the aerosols of the majority of ENDS contain toxic chemicals, including nicotine and substances that can cause cancer.ENDS on their own are associated with increased risk of cardiovascular diseases and lung ...
The paper indicates that e-cigarettes are more effective in influencing smoking cessation than the use of smoking therapies such as nicotine-replacement therapy.
Conclusions about the effects of electronic cigarettes remain the same An updated Cochrane Review provides an independent, rigorous assessment of the best available evidence to date about electronic cigarettes for quitting smoking.
E-cigarettes are a relatively new tobacco product that have been sold in the U.S. for about a decade The e-cigarettes currently in the U.S. marketplace have not been systemically reviewed by the Food and Drug Administration to determine their impact on lung health. While much remains to be determined about the lasting health consequences of these products, the American Lung Association is very ...
ESSA Y E-cigarettes: the best and the worst case scenarios for public health—an essay by Simon Chapman Considerable energy is going into envisioning the lik ely benefits and har ms of the ...
Argumentative Essay On E-Cigarettes. Invented in the early 2000s, e-cigarettes intended to become a replacement for conventional cigarettes. Due to the proven health deficits of conventional cigarettes, e-cigarettes have become a safer alternative to smoking over the past two decades. However, there are still active debates about whether e ...
In this essay, I consider the best and worst case scenarios for e-cigarettes; claims that they assist in smoking cessation and their value if users continue to smoke; and, finally, the tobacco industry's interests in these products.
Discussion: Vaping and E-Cigarettes Essay. Exclusively available on IvyPanda®. Electronic nicotine delivery systems cause the same harm to the human body as other tobacco products. Plus, polyhydric alcohol solvents kill cell membranes. All this can lead to severe illnesses. If the main harmful effect of conventional cigarettes comes from tar ...
Summary E-cigarette aerosol contains fewer numbers and lower levels of most toxicants than does smoke from combustible tobacco cigarettes. Exposure to nicotine and to toxicants from the aerosolization of e-cigarette ingredients is dependent on user and device characteristics. Laboratory tests of e-cigarette ingredients, in vitro toxicological tests, and short-term human studies suggest that e ...
Essay On E-Cigarettes. E-cigarettes run on a lithium battery and contain a vaporization chamber and a cartridge filled with liquid. When you puff on your e-cig as you would a regular cigarette, the battery powers the device to heat the liquid and vaporize it. Some e-cigarettes have a cigarette-like LED tip that glows red (or another color ...
Essay On E-Cigarette. 1585 Words7 Pages. E-cigarette: Is it safe? Kristy grew up in a small town in Tennessee and smoked her first cigarette at age 13 with an older sister. Many of her friends and family members smoked. Kristy followed in their footsteps and became a regular smoker. By age 33, Kristy had been smoking for 20 years.
The topic of e-cigarettes is controversial. Opponents focus on e-cigarettes' risks for young people, while supporters emphasize the potential for e-cigarettes to assist smokers in quitting smoking. Most US health organizations, media coverage, and policymakers have focused primarily on risks to youths. Because of their messaging, much of the public—including most smokers—now consider e ...
Electronic Cigarettes Essay. 748 Words3 Pages. Electronic Cigarettes: A Healthy Alternative? The use of electronic cigarettes has more than doubled among United State middle and high school students from 2011 to 2012 ("Press Release"). The number of people purchasing electronic cigarettes is growing without buyers understanding the ...
The success of e-cigarettes is such that sales of these products are rapidly gaining on traditional cigarettes. The rapidly evolving phenomenon is raising concerns for the health community, pharmaceutical industry, health regulators and state governments. Obviously, these products need to be adequately regulated, primarily to protect users.
E-cigarettes and Vaping Epidemic Across The United States. As a middle schooler, my father warned me of the dangers of smoking. His incessant resistance to cigarette use began after he saw its deteriorating effects on my late grandmother. Both his warnings and her struggle to breathe discouraged me from using cigarettes.
Electronic Cigarette Essay. 1050 Words5 Pages. Electronic Cigarettes: The New Cig It seems as if the traditional nicotine cigar has become a puff of the past with the rising popularity of the electronic cigarette, due to its easy portability and addictive contents. Electronic cigarettes are known as e-cigs, e-vapes, or hookah pens (McMillen).
Electronic cigarettes (e-cigarettes) are effective for helping people to stop smoking 1 and are less harmful than combustible cigarettes (referred to hereafter as cigarettes). 2 However, many adults who smoke in England (as in many other countries) believe that e-cigarettes are at least as harmful to health as cigarettes, 2-4 which can dissuade ...
This essay will discuss the intentions of E-cigarettes as a whole, the targeted and proposed demographics, and whether or not allegations made against or towards E-cigarettes retain any crucial validity. To fully understand the nature of this topic, one should first be made aware of the inner-workings of an E- cigarette.
Argumentative Essay On E-Cigarettes. 512 Words3 Pages. E-cigarettes have positive affects that are less harmful for people to get cancer. Most people who use traditional cigarettes are exposed to toxins that cost health issues. This new technology was designed this device to imitate the feeling of smoking without the harmful effects.